Journal of
eISSN: 2373-4310


Research Article Volume 4 Issue 3
1Jean Mayer USDA Human Nutrition Research Center on Aging, Tufts University, USA
2Department of Nutritional Sciences and Food Hygiene, Shandong University, China
3Shandong Mental Health Center, China
Correspondence: Xinying Lin, Department of Nutritional Sciences and Food Hygiene, College of Public Health, Shandong University, Jinan, 44 Wenhuaxi Road, Jinan 250012, People's Republic of China, Tel +86-531-88382135, Fax +86-531-88382553
Received: April 26, 2016 | Published: May 20, 2016
Citation: Meng H, Lin X, Hu L. Evaluation of nutritional status and dietary intake in older adults living at home and nursing homes in Dongying, China. J Nutr Health Food Eng. 2016;4(3):451-458. DOI: 10.15406/jnhfe.2016.04.00134
Objective: The current study determined the nutritional status and dietary intake of older adults living at home and nursing homes (NH) in Dongying district of the city of Dongying.
Methods: Nutritional status and dietary intake of older adults living at home and NH were analyzed using 24h recalls questionnaires, and evaluated based on the recommended intake and DRIs from dietary guidelines for Chinese older adults. Comparisons between two groups were also measured.
Results: The intake of grains and yams, vegetables, meat, eggs, and legumes in older adults living at home, and the intake of grains and yams and eggs in older adults living at NH meet the recommended intake for Chinese older adults. The intake of carbohydrate, vitamin B3, selenium, and potassium in older adults living at home, and the intake of carbohydrate in older adults living at NH meet the corresponding DRIs. Older adults living at home had higher intake of vegetables, meat, seafood, legumes, macronutrients, vitamin B, C, E, calcium, iron, zinc, potassium, and lower intake of sodium compared to older adults living at NH.
Conclusions: Overall, older adults living at home had better food and nutrient intake compared to older adults living at NH. The intake of many food and nutrients in older adults with both living patterns did not meet recommended intake levels. Improvement in the nutritional status of older adults is needed to guarantee successful aging among Chinese populations.
Keywords: older adults, living patterns, nutritional status, dietary intake
NH, nursing homes; DRIs, dietary reference intakes; BMI, body mass index
The proportion of older adults in overall population in China has been increasing rapidly since the beginning of 21 centuries, and the Chinese government faces economic, social and public health challenges due to the fast-growing elderly population. To increase life expectancy and quality of life of older adults, it is essential to guarantee that they are maintaining physical and mental health and function. However, a recent study of China’s aging population reports that a third of older people have poor health due to various reasons.1 One of the fundamental factors that impact health of older adults is nutritional status.2‒4 Adequate and balanced dietary intake and eating behaviors of older people enables maintenance of physical and cognitive function and refrains from age-related increase in infectious diseases and chronic diseases (e.g. cardiovascular disease, type II diabetes, osteoporosis, cancer).3,5
The most commonly used living patterns of older people in China include living at home (either alone or with spouse or children) and living at nursing home (NH). Although most of the healthy older adults still prefer to live at home, living at NH has become a trend among seniors due to the improvement in professional care and service, safety and rewarding environment. One major difference between the older adults living at home and NH is their dietary intake pattern. Older people living at home have more freedom in choice of food compared to people living at NH, while the nurses and staff at NH may provide guidance on dietary intake and eating behavior. However, it is unclear if the nutritional status and dietary intake differ between older adults living at home and NH.
The objectives of our current study are to determine if the nutritional status and dietary intake of older adults living at home and NH in Dongying district of the city of Dongying meet recommended levels in the dietary guidelines, and if these values differ between two groups. Better understanding of this topic is necessary to design effective strategies and policies to ensure better health care and quality of life of older populations and successful aging in China.
Participants
Healthy subjects (n=156) who were 60-85years of age and had been living in Dongying district of the city of Dongying for more than 10years were enrolled in the study during January to April of 2010. Of the total 156 participants, 89 were randomly selected from older adults who lived at home (either alone or with spouse or children), and 67 were randomly selected from 2 NH in Dongying district. Older adults who were not able to answer questions without aid of another person were excluded from the study.
Trained study personnel conducted face-to-face interviews with the participants. On the day of interviews, participants were given information about the study. After written informed consent was signed, demographic and anthropometric information, medical history, and alcohol consumption were obtained using a series of medical and lifestyle questionnaires. Body weight and height of participants were measured by trained study personnel, and BMI was calculated according to body weight and height measured. BMI was categorized based on the Ministry of Health of the People’s Republic of China guidelines. An individual with BMI <18.5kg/m2 was consider underweight, 18.5-23.9kg/m2healthy, 24-28kg/m2 overweight, and ≥28kg/m2obese. All study procedures were performed with approval of the Institutional Review Board of Baotuquan campus of Shandong University (Jinan, Shandong, China).
Dietary intake assessment tool
Dietary intake of the participants was obtained via 24hour dietary recalls for 3 days, including one weekend day. Briefly, participants were asked to recall their intake of food and beverages during breakfast, lunch, dinner, and snakes in the three days according to detailed instructions provided by trained staff. Portion size of each of the food items was also provided. Intake of macronutrients, vitamins, and minerals was analyzed based on the recorded food intake of participants using CFC software. Recommended food intake as categorized in food groups and dietary reference intakes (DRIs) of nutrients were obtained according to the 2010 dietary guideline for Chinese older adults.
Statistical analyses
All data were analyzed using Graphpad Prism 5. Comparisons of total energy intake, food and nutrient intake between two groups were analyzed using student’s t test if the parameters were under normal distribution and Mann-Whitney test if the parameters were nonparametric. Comparisons of qualify rate of food and nutrient intake between two groups were analyzed using Chi Square. Statistical significance was accepted at p≤0.05 levels.
Participant characteristics
Descriptive data are presented in Table 1. Of the 156 older adults who provided complete demographic information and dietary questionnaires, 89 were living at home and 67 were from NH. The mean age of older adults living at home was 67.0±0.7years old, ranging from 60 to 85. The mean age of older adults living at nursing homes was 78.9±0.9years old, ranging from 60 to 90. The average age of subjects living at home was significantly smaller compared to subjects living at NH. The average BMI of older adults living at home and NH was 23.7±0.3 and 23.7±0.4 kg/m2, respectively. The percentage of lean older adults was 3.4% in those living at home, and 1.5% in those living at NH. The percentage of older adults who were overweight and obese was 44.9% and 46.3% in those living at home and NH respectively. The percentage of lean, normal weight, overweight and obese older adults were similar between two groups. The average alcohol consumption was 18.3±3.8 and 16.8±4.9 grams/day in older adults living at home and NH, respectively. All the subjects did not have self-reported chronic diseases. Overall, all the subjects were healthy older adults.
Variables |
Values |
|
|---|---|---|
|
Older Adults |
Older Adults |
Age (yr) |
67.0 ± 0.7* |
78.9 ± 0.9 |
Male, n (%) |
46 (51.7) |
25 (37.3) |
Height (m) |
1.7 ± 0.0 |
1.6 ± 0.0 |
Weight (kg) |
65.1 ± 1.2 |
60.6 ± 1.1 |
Body mass index (kg/m2) |
23.7 ± 0.3 |
23.7 ± 0.4 |
Lean (≤18.5), n (%) |
3 (3.4) |
1 (1.5) |
Normal weight (18.5-23.9), n (%) |
46 (52.7) |
35 (52.2) |
Over weight (24.0-28.0), n (%) |
33 (37.0) |
24 (35.9) |
Obese (≥28.0), n (%) |
7 (7.9) |
7 (10.4) |
Alcohol consumption (g/day) |
18.3±3.8 |
16.8±4.9 |
Difference in daily energy and food intake between older adults living at home and NH
The average total daily energy intake was 1948.9kcal and 1482.1kcal in older adults living at home and NH, respectively. The average total daily energy intake was significantly greater in older adults living at home compared to NH (p<0.0001).
The total daily food intake as illustrated by 8 food groups in older adults living at home and NH and recommended intake for Chinese older people was presented in Table 2. The recommended daily food intake for older adults living at home and NH was chosen based on 2000kcal and 1600kcal total daily energy intake, respectively. The daily intake of grains and yams (p<0.0001), vegetables (p<0.05), and eggs (p<0.0001) in older adults living at home was significantly greater than recommended intake. Daily meat intake was slightly higher than recommended intake, although it did not reach statistical significance. However, the daily intake of fruits (p<0.0001), seafood (p<0.0001) and dairy products (p<0.0001) was significantly lower compared to recommended intake. Unlike older adults living at home, the daily intake of only grains and yams (p<0.0001) and eggs (p<0.0001) in older people living at NH was significantly higher than recommended intake values. The daily intake of vegetables in older adults living at NH was close to the recommended intake. Their daily intake of fruits, meat, seafood, and dairy products was significantly lower compared to recommended intake (p<0.0001).
Food Groups |
Older Adults At Home |
Older Adults Lat NH |
||
|---|---|---|---|---|
Value (G) |
Recommended Intake (G) |
Value (G) |
Recommended Intake (G) |
|
Grains and Yams |
487.57±21.48a |
300 |
483.71±5.38a |
225 |
Vegetables |
406.09±26.21b |
350 |
291.12±13.47 |
300 |
Fruits |
123.43±9.30a |
300 |
137.80±4.44a |
200 |
Meat |
52.90±5.80 |
50 |
30.20±2.96a |
50 |
Seafood |
11.95±2.88a |
75 |
2.09±0.20a |
75 |
Eggs |
51.97±4.06a |
25 |
51.24±5.52a |
25 |
Dairy |
43.30±7.75a |
300 |
41.39±8.44a |
300 |
Legumes |
90.86±9.53a |
40 |
10.94±1.75a |
30 |
The comparisons in daily food intake between older adults living at home and NH were presented in Figure 1. The daily intake of vegetables (p=0.0005), meat (p=0.0018), and seafood (p=0.0035) was significantly greater in older adults living at home than NH. The daily intake of grains and yams, fruits, eggs, and dairy products was similar in older adults in two groups.
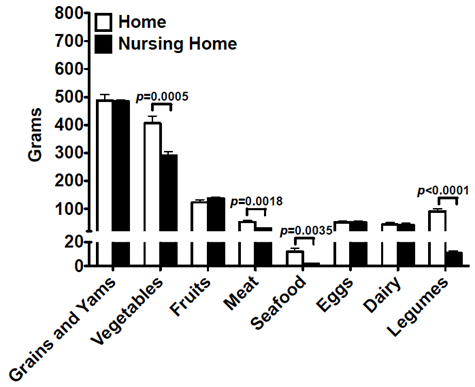
Figure 1 Difference in daily food intake between older adults living at home and NH. Comparisons in daily intake of food categorized in food groups were measured between older adults living at home and NH. Data are presented as mean ± SEM.
Difference in daily nutrient intake between older adults living at home and NH
The total daily nutrient intake as classified by macronutrients, micronutrients, and minerals in older adults living at home and NH and dietary reference intake (DRI) for Chinese older people was presented in Table 3. The DRIs for older adults living at home and NH was chosen based on 2000 and 1600 kcal total daily energy intake, respectively.
|
Older Adults At Home |
Older Adults At Nursing Home |
||
|---|---|---|---|---|
Nutrients |
Values |
DRIS |
Values |
DRIS |
Macronutrients (g) |
||||
Carbohydrate |
310.55±10.47c |
282 |
261.00±6.05a |
210.9 |
Protein |
73.94±2.77 |
75 |
52.76±2.21c |
58.8 |
Lipid |
51.48±3.55d |
59.6 |
29.31±1.09a |
55 |
Micronutrients (mg) |
||||
Vitamin A |
388.29±26.99a |
821.7 |
322.03±27.53a |
687 |
Vitamin B1 |
1.01±0.05c |
1.2 |
0.65±0.03a |
1.0 |
Vitamin B2 |
0.93±0.04a |
1.2 |
0.69±0.02a |
1.1 |
Vitamin B3 |
16.31±1.17c |
13 |
7.34±0.29a |
13 |
Vitamin C |
117.04±7.64a |
150 |
41.31±3.39a |
116.9 |
Vitamin E |
24.78±1.60a |
37.7 |
11.66±0.12a |
32.3 |
Minerals (mg) |
||||
Calcium |
540.59±29.67a |
724.8 |
355.41±17.42a |
625.5 |
Iron |
22.35±0.96 |
23.8 |
15.88±0.51a |
18.5 |
Zinc |
10.24±0.41a |
12 |
7.48±0.28a |
9.6 |
Selenium |
50.89±1.63 |
50 |
47.51±0.78c |
50 |
Potassium |
2377.34±112.69a |
2000 |
1380.21±59.02a |
2000 |
Sodium |
4397.26±63.16a |
2200 |
4649.74±26.52a |
2200 |
The daily intake of carbohydrates in older adults living both at home (p<0.01) and NH (p<0.0001) was significantly greater than corresponding DRIs. The daily lipid intake in both home (p<0.05) and NH (p<0.0001) groups was significantly lower than DRIs. The daily intake of protein in older adults living at homes was close to the DRI. However, the daily intake of protein in older adults living at NH was significantly lower compared to DRI (p<0.01).
The daily intake of vitamin A (p<0.0001), B1 (p<0.01), B2 (p<0.0001), C (p<0.0001), and E (p<0.0001) in older adults living at home was significantly lower than DRIs, while the vitamin B3 (p<0.01) intake was significantly greater than DRI. Daily intake of all the micronutrients measured in the study in older adults living at NH was significantly lower than DRIs (p<0.0001).
The daily potassium and sodium intake in older adults living at home was significantly higher than DRIs (p<0.0001), and selenium intake was slightly higher than DRI. The daily intake of calcium and zinc in older adults living at home was significantly lower than DRIs (p<0.0001). Their daily iron intake was also lower than recommended intake, although it did not reach statistical significance. The daily sodium intake in older adults living at NH was significantly higher than DRI (p<0.0001). However, their daily intake of selenium (p<0.01) and all other minerals (p<0.0001) was significantly lower than recommended intake.
The comparisons in daily nutrient intake between older adults living at home and NH were presented in Figure 2. The daily intake of all carbohydrate (p=0.0003), lipid (p<0.0001) and protein (p<0.0001) was significantly greater in older adults living at home than NH. The daily intake of vitamin B1, B2, C, and E and niacin was significantly greater in older adults living at home than NH (p<0.0001), and vitamin A intake was similar between two groups. Moreover, older adults living at home had significantly higher daily calcium, iron, zinc and potassium intake (p<0.0001), and lower sodium intake (p=0.0012) compared to older adults living at NH. Daily selenium intake was similar between two groups.
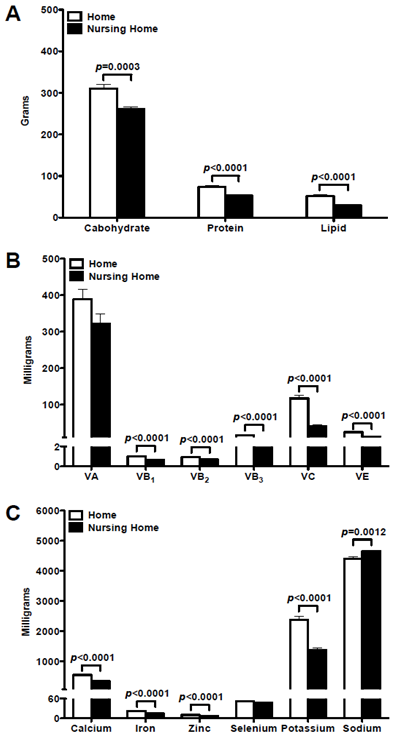
Figure 2 Difference in daily nutrient intake between older adults living at home and NH. Comparisons in daily intake of macronutrients, vitamins, and minerals were measured between older adults living at home and NH. Data are presented as mean ± SEM.
Comparisons in food and nutrient intake qualify rate between older adults living at home and NH
Due to the age difference between older adults living at home and NH, their recommended intake and DRIs were different. In order to adequately compare the food and nutrient intake between two groups, qualify rates were calculated as the percentage of older adults whose intake meet their corresponding DRIs, and presented in Table 4. Among older adults living at home, less than 50% met the requirements for the intake of vegetables, fruits, seafood, protein, lipid, all micronutrients, calcium, iron, and zinc, and nobody met the requirements for dairy and sodium intake. Among older adults living at NH, less than 50% met the requirements for the intake of vegetables, meat, eggs, protein, vitamin B1 and B2, calcium, iron, zinc, selenium, and potassium, and nobody met the requirements for fruits, seafood, dairy, legume, lipid, vitamin A, B3, C and E, and sodium intake.
|
Older Adults At Home |
Older Adults At NH |
|
||
|---|---|---|---|---|---|
Food Or Nutrients |
Qualified Rate (%) |
Non-Qualified Rate (%) |
Qualified Rate (%) |
Non-Qualified Rate (%) |
P Value |
Food Groups |
|
|
|
|
|
Grains and Yams |
82.02 |
17.98 |
100.00 |
0.00 |
0.0002 |
Vegetables |
49.44 |
50.56 |
37.31 |
62.69 |
0.1312 |
Fruits |
5.62 |
94.38 |
0.00 |
100.00 |
0.0486 |
Meat |
50.56 |
49.44 |
37.31 |
62.69 |
0.0996 |
Seafood |
6.74 |
93.26 |
0.00 |
100.00 |
0.0302 |
Eggs |
77.53 |
22.47 |
37.31 |
62.69 |
<0.0001 |
Dairy |
0.00 |
100.00 |
0.00 |
100.00 |
N/A |
Legumes |
62.92 |
37.08 |
0.00 |
100.00 |
<0.0001 |
Macronutrients |
|
|
|
|
|
Carbohydrate |
62.92 |
37.08 |
100.00 |
0.00 |
<0.0001 |
Protein |
43.82 |
56.18 |
37.31 |
62.69 |
0.4134 |
Lipid |
33.71 |
66.29 |
0.00 |
100.00 |
<0.0001 |
Micronutrients |
|
|
|
|
|
Vitamin A |
6.74 |
93.26 |
0.00 |
100.00 |
0.0302 |
Vitamin B1 |
33.71 |
66.29 |
10.45 |
89.55 |
0.0007 |
Vitamin B2 |
25.84 |
74.16 |
2.99 |
97.01 |
0.0001 |
Vitamin B3 |
46.07 |
53.93 |
0.00 |
100.00 |
<0.0001 |
Vitamin C |
30.34 |
69.66 |
0.00 |
100.00 |
<0.0001 |
Vitamin E |
20.22 |
79.78 |
0.00 |
100.00 |
<0.0001 |
Minerals |
|
|
|
|
|
Calcium |
22.47 |
77.53 |
4.48 |
95.52 |
<0.0001 |
Iron |
35.96 |
64.04 |
37.31 |
62.69 |
0.8615 |
Zinc |
25.84 |
74.16 |
37.31 |
62.69 |
0.1244 |
Selenium |
53.93 |
46.07 |
37.31 |
62.69 |
0.0395 |
Potassium |
55.06 |
44.94 |
10.45 |
89.55 |
<0.0001 |
Sodium |
0.00 |
100 |
0.00 |
100 |
N/A |
Table 4 Percentage of older adults living at home and nursing home with food and nutrient intake meet DRIs
The qualify rate for intake of grains and yams (p=0.0002), fruits (p=0.0486), seafood (p=0.0302), eggs (p<0.0001), legumes (p<0.0001), carbohydrate (p<0.0001), lipids (p<0.0001), vitamin A (p=0.0303), B1 (p=0.0007), B2 (p=0.0001), B3 (p<0.0001), C (p<0.0001), E (p<0.0001), calcium (p<0.0001), selenium (p=0.0395) and potassium (p<0.0001) was significantly greater in older adults living at home than NH. The qualify rate for intake of vegetables, meat, dairy, protein, iron, zinc, and sodium was similar between two groups.
To our knowledge, this study provides the first documentation in evaluating nutritional status and dietary intake in healthy older adults living at home and NH in Dongying district of the city of Dongying, and comparing the differences between older adults with different living patterns. We found that older adults living at home had better food and nutrient intake than older adults living at NH. However, the intake of many food and nutrients in older adults with both living patterns did not meet the recommended intake levels.
The daily intake of fruits, seafood and dairy in older adults living at home, and the daily intake of fruits, legumes, meat, seafood and dairy in older adults living at NH did not reach recommended intake. Overall, the food intake in older adults living at homes was better than older adults living at NH. The daily intake of fruits, seafood and dairy in older adults at both groups did not reach their corresponding recommended intake. Fruits are low-energy-dense food, and increase in fruit consumption can increase satiety and restrict total calorie intake, which helps to maintain body weight of older adults.6,7 Fruits contain a lot of vitamins, minerals and fibers, which are essential in lowering the risk of numerous chronic diseases and infectious diseases.8,9 An epidemiologic study has shown that an increase in the daily intake of 50g of fruits contributes to a 20% reduction in the mortality from cancer of numerous types, and cardiovascular diseases.10 Evidence also shows that intake of 5 servings of fruits and vegetables a day can lead to the blood vitamin C level of greater than 60mmol/L, which is associated with a 4-fold reduction in mortality in individuals aging from 40 to 79years old.11 Seafood is good sources of high quality protein and n-3 and n-6 polyunsaturated fatty acids, which decreases the risk of cardiovascular diseases in older individuals.12,13 Calcium content and bioavailability in dairy products are high, and thus increase in dairy intake can prevent older adults from osteoporosis and fracture.14,15 Combined, older adults living at home and NH should increase their daily fruits, seafood and dairy intake. Older adults living at NH had low intake of meat and legumes, leading to low intake of high quality proteins. Prolonged inadequate protein intake may cause loss in skeletal muscle and malnutrition in older populations.5,16,17 Therefore, older adults living at NH should increase their daily meat and legume intake.
The daily intake of macronutrients was significantly higher in older adults living at home compared to older adults living at NH, which could also explain the greater total energy intake in the former group. The daily carbohydrate intake was higher than DRIs in older people of both groups, which may be due to their large consumption of grains and yams. In contrast, the daily intake of proteins and lipids in older adults of both groups were significantly lower than DRIs, which may be due to the inadequate consumption of meat, seafood, legume and dairy products. The total body protein, skeletal muscle mass and functional proteins involved in important physiological processes reduce as people get older. This situation contributes to slow enzyme activities, decreased immune function and increased susceptibility to infections, and prolonged time for wound healing.17 Thus, inadequate dietary protein intake is deleterious in older adults due to the acceleration of the above problems.16,17 Although excessive lipid intake may increase the serum levels of triglyceride, total cholesterol, and low-density lipoprotein, high intake of monounsaturated fatty acids and n-3 and n-6 polyunsaturated fatty acids have been shown to contribute to reducing the mortality from cardiovascular diseases.12,13 Therefore, older adults in both living patterns should achieve a balanced macronutrient ratio via decreasing carbohydrate consumption and increase consumption of high quality proteins and mono- and polyunsaturated fatty acids.
Vitamin A, B1, B2, B3, C, and E are critical for the health of older populations.5,18 According to our observations, the daily vitamin intake was higher in older adults living at home compared to older adults living at NH. However, the daily intake of vitamin A, B1, B2, C, and E in older adults in both groups did not reach DRIs. This was partially due to the low intake of fruits, red meat and legumes in both groups. Inadequate intake of vitamin A can cause vision problem, impaired immune function and increased risk of infection and various cancer.18‒20 Vitamins B1, B2, B3 are key elements involved in energy production pathways, and deficiencies in B vitamins cause peripheral neuropathy, dementia, and muscle tenderness, etc.18 Vitamin C and E are important antioxidants to human body, and deficiencies in vitamin C and E were associated with increased susceptibility to infection, inflammation, and numerous chronic diseases and decreases quality of life in older populations5,8,11,18,21 Combined, older adults living at home and NH should increase consumption of fruits, vegetables, legumes and meat to meet their needs for vitamins.
Minerals are also crucial for older adults. Older adults living at home had higher daily calcium, iron, zinc and potassium intake, and lower sodium intake compared to older adults living at NH. However, the daily intake of calcium, zinc, and iron in older adults living at home and intake of calcium, zinc, selenium, iron and potassium in older adults living at NH did not reach DRIs. Calcium plays an important role in multiple physiologic processes, among which bone health is vital in older populations.5,4,15 Osteoporosis and bone fractures are major public health problems among older populations in China, and they contribute to both morbidity and mortality in older adults.14 The number of Chinese older adults who are susceptible to osteoporosis has been increasing due to their low intake of calcium, which is partially caused by low consumption of dairy products, such as milk and yogurt.5,14,22 Zinc is vital in numerous physiologic processes, including immune responses, enzyme activities, cell growth and development, etc.23 The immune function of individuals declines with age, and immune responses of older adults (>65years old) have been demonstrated to be lower compared to younger people (<65years old).24 The impairment in immune function in older adults is partially due to zinc deficiency.18,21 Low serum zinc levels have also been shown to increase the risk of Alzheimer disease in older populations.25 Iron is needed to maintain normal immune function and prevention from anemia.22,26 Although the iron intake in older adults in both groups was only a little less than DRIs, they need to maintain adequate iron intake via consuming enough red meat, legumes, fruits, and whole grains. However, excessive iron intake has been reported to increase the risk of Alzheimer disease in older populations.27 Thus, balanced iron consumption is needed in older populations. Older adults living at NH had low selenium intake compared to DRI. Previous studies reported selenium deficiency was associated with reduction in immune function and increased risk of anemia and cancer in older populations.28,29 Older adults living at NH also had inadequate intake of potassium. Higher potassium consumption is associated with greater bone mineral density and lower risk of hypertension and stroke in older populations.30,31 However, the sodium intake in older adults in both groups had doubled the recommended intake level. Strong evidence shows that excessive sodium consumption increases the risk of hypertension and cardiovascular disease in people including older populations.5,32 Therefore, older adults should restrict their sodium consumption via reducing the intake of processed food and table salts and increasing the intake of potassium-rich food.
Overall, older adults living at home had better nutritional and dietary intake status than older adults living at NH in Dongying district of the city of Dongying. NH should hire experienced dietitians who can provide advices and recommendations to older adults, and help prepare food that meet the nutritional needs of older adults to improve their nutritional status and maintain health. However, older adults in both living patterns had several problems in dietary intake, including inadequate consumption of fruits, vegetables, legumes, and dairy products, which resulted in low intake of various macronutrients, vitamins, and minerals. Nutritional status and dietary intake are crucial in the overall health and quality of life of older populations. Therefore, policies that can improve the nutritional status of older populations are needed to guarantee the successful ageing among Chinese populations.
None.
Author declares that there is no conflict of interest.

©2016 Meng, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.