eISSN: 2572-8474


Commentary Volume 5 Issue 1
Department of Nursing, National University of Singapore, Singapore
Correspondence: Department of Nursing, National University of Singapore, Singapore
Received: July 04, 2017 | Published: February 12, 2018
Citation: Simone QQM, Xuan OZ. Improving mentoring through a blend of novice and peer, near peer and group mentoring: a commentary. Nurse Care Open Acces J. 2018;5(1):43-44. DOI: 10.15406/ncoaj.2018.05.00117
Mentoring is increasingly seen as a means of providing appropriate, personalised, timely and holistic support for learners.1–5 Recent reviews suggest that a particularly effective means of providing such support lies in novice mentoring or mentoring between senior clinicians and medical students or junior doctors. However shortages of mentors, time constraints both on the part of mentees and mentors and concerns about the timeliness of mentoring support have raised concerns as to the viability of novice mentoring on a larger scale.
Our experiences with mentoring in the Palliative Medicine Initiative (PMI) run by the Division of Palliative Medicine at the National Cancer Centre Singapore offers a potential solution for this problem. Here novice mentoring is coupled with near peer and peer mentoring to provide timely mentoring support (Figure 1).
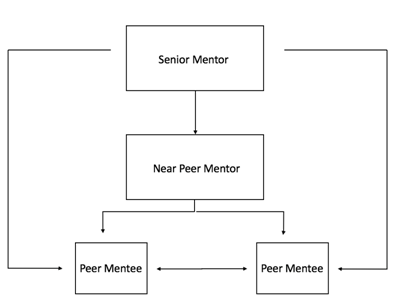
Figure 1 Mentoring in the Palliative Medicine Initiative that sees mentoring support also provided through phone contact, email and text and whatsapp messaging.
Peer mentorship is widely employed by various medical institutions and can take the form of peer, near peer and group mentoring. Junior doctors mentor each other and or medical students in groups or on a one to one basis guided by a senior mentor. This achieves the dual function of encouraging peers to share resources and help each other, while providing a guide who crucially possesses the necessary professional, academic and psychosocial experience that can translate into practical advice and help. Near peer mentorship from housemen to students for example has proven more experientially relevant to the struggles of the student. Kman et al.6 notes that peer mentorship “avoids the common mentoring pitfall known as the “authority gradient” in which the gap between mentor and mentee leads to an ineffective relationship”.7,8 Also significantly noted that peer mentorship usually evolved into a connection that more resembled a friendship than a mere working relationship which has been found to sustain effective mentoring relationships.4 Peer and near peer mentorship allows students to appreciate the value of working together as a team, whether it is with peers or a senior mentor, to achieve both overall and individual success. Similar struggles, interests and aspirations discussed forges bonds that are gradually strengthened over the period of mentorship.6 The process is also mutually beneficial with senior members of the near peer mentoring dyad “developed essential attributes of time management, communication and leadership for mentors”.7 The combination of group, near peer, peer and novice mentoring also rewards mentors with “the recognition… the teaching can be enjoyable, rewarding and beneficial to them’’ which in turn urges them to continue capitalizing on their strengths and improve on their weaknesses.
Overall the PMI mentoring model also creates an environment in which experiential learning empowers mentors to make a difference and witness that change for themselves. We believe the cycle of affirmation constructed between mentor and mentee in PMI style mentoring creates a positive culture of constant learning and improvement, which may continue to have an extensive impact on the individual as well as future generations of medical students even as they prepare to enter the medical profession.
None.
The author declares no conflict of interest.

©2018 Simone, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.