Journal of
eISSN: 2373-4426


Case Report Volume 6 Issue 6
1Departments of Paediatric Surgery, B J Medical Government College and Sassoon Hospital, India
2Departments of Pediatrics, B J Medical Government College and Sassoon Hospital, India
Correspondence: Minakshi Bhosale, Departments of Paediatric Surgery, B J Medical Government College and Sassoon Hospital, G / 101, Sudarshan Apartments, Behind Spencers Daily, Karvenagar, Pune-411 052, Maharashtra, India, Tel 91- 93254 27226
Received: June 08, 2017 | Published: June 12, 2017
Citation: Bhosale M, Valvi C (2017) A Rare Case of Neonatal Colonic Mucormycosis. J Pediatr Neonatal Care 6(6): 00267. DOI: 10.15406/jpnc.2017.06.00267
Mucormycosis of the neonatal gut is a rare disease, with uniformly fatal prognosis. It has occasionally been reported involving the stomach and ileum in immunocompromised hosts. However, mucormycosis of the colon is very rare. We report case of a preterm, low birth weight (LBW) neonate with clinical features of necrotizing enterocolitis found to have characteristic black-velvety colonic gangrene on exploratory laparotomy. The baby initially improved but succumbed to sepsis eventually. Tissue histology diagnosed mucormycosis of the colon. The diagnosis of colonic mucormycosis was unsuspected. This report is presented to create awareness about this rare entity so that it is suspected and diagnosed early.
Keywords: colon, mucormycosis, neonate, low birth weight, necrotizing enterocolitis
LBW, low birth weight; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit
Neonatal gastrointestinal mucormycosis is a rare, opportunistic fungal infection, with dismal prognosis. Since, the diagnosis is based on histopathological examination of the resected segment (specimen) of stomach and/or bowel, it cannot be diagnosed preoperatively.1,2 These cases are initially diagnosed as necrotizing enterocolitis (NEC), but later on are confirmed as gastrointestinal (colonic) mucormycosis. Hence, there is delay in specific treatment.
Eight-day-old male neonate was admitted in neonatal intensive care unit (NICU) for preterm care. He was born vaginally to an adolescent primigravida mother at 32 weeks gestational age. His birth weight was 1.2 Kg. The mother had received regular antenatal care and had no identifiable risk factors. Baby had not cried immediately following spontaneous vaginal delivery and had required bag and mask ventilation. There were no obvious congenital anomalies. He was on oral Sildenofil for management for pulmonary hypertension.
On tenth day of life, he developed feeding intolerance and per rectal bleeding. A soft to firm lump of about 2×3 cm in size was palpable in the right hypochondriac region. Nasogastric tube aspirate was bilious. Erect X-ray abdomen showed dilated stomach with paucity of gas in lower abdomen and pelvis (Figure 1). Dye study done for confirmation of diagnosis showed the same picture i.e. only gastric shadow could be visualized. Ultrasonography of the abdomen showed dilated, peristaltic bowel loops. Haematologic investigations showed raised WBC counts of 16,000/cmm and low Platelet count of 100,000/cmm. The differential diagnosis was malrotation with volvulus or necrotizing enterocolitis. In view of poor general condition, the child was explored under local anaesthesia. He had characteristic black-velvety gangrene confined to middle 8-10 cm of the mid-transverse colon without any frank / impending perforation. Initial 5-7 cm of mid-transverse colon from the hepatic flexure was normal. Rest of the colon and small bowel was healthy looking. The non-viable colon was excised. After resection, the free ends were brought out as colostomy and mucus fistula through either end of the incision. Blood loss of about 20 cc was replaced on table. Post-operatively the activity improved. Nasogartric feeds were started on post-operative day three, once colostomy was functioning. Initially they were well-tolerated.

Figure 1 Erect X-ray abdomen showed dilated stomach with paucity of gas in lower abdomen and pelvis.
Histopathological diagnosis of colonic mucormycocis was a surprise and totally unsuspected. The excised large bowel wall demonstrated significant tissue infiltration by fungal organism. This fungal organism had irregular branching, nonseptated appearance and vascular invasion of intestinal blood vessel lumina by the fungal hyphae (Figure 2).
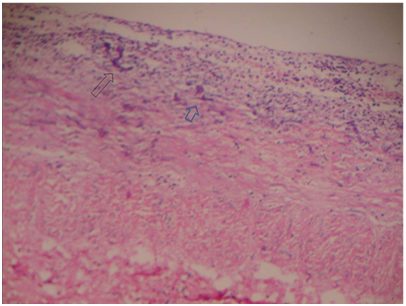
Figure 2 Histopathology slide showing colonic wall with significant infiltration by branching fungal hyphae. Also note colonic vascular invasion by the hyphae (H and E 40 ×).
Intravenous Liposomal Amphotericin B was commenced on postoperative day six, based on the histopathological diagnosis. However, reports of Bacterial and fungal cultures of blood and peritoneal fluid, received subsequently were negative for mucormycosis. Initially, baby tolerated the Antifungal therapy well. There was superficial wound gape (Figure 3), for which regular dressings were done. However, he developed renal failure and eventually succumbed to sepsis on postoperative day 10.
Low birth weight babies are at risk of mucormycosis infection if exposed to Mucorales. The speculations being immature immune system, requirement of lengthy NICU stay (with increased invasion), nursing in environment of high ambient humidity (around 85%) and fragile skin barrier. All these factors may enhance growth of and exposure to Mucorales. Also, they receive broad-spectrum intravenous antibiotics, which affect healthy gastrointestinal flora; and they are often given steroids to assist weaning off from the ventilator.3 Interventions such as oro-gastric tube placement,4 endotracheal intubation, and Indomethacin therapy are speculated to increase risk of contracting gastrointestinal mucormycosis by causing mucosal injury.5
In childhood gastrointestinal mucormycosis, stomach is the most commonly involved organ,5 whereas in neonates, the colon is predominantly involved. Alexander P et al have reported 3 babies with colonic necrosis with multiple perforations.2 The clinical manifestation of majority of these patients mimicked those of NEC. However, only 3 babies presented with an abdominal mass in the initial course of the illness.
Uniformly, the prognosis has been grave with only 4 cases being diagnosed antemortem leading to surgical intervention, antifungal therapy and out of this only three survived.2 Two of the babies who survived, needed a second laparotomy and surgical debridement few months after the neonatal period. The high mortality rate may be due to lack of clinical suspicion, coupled with inadequate surgical debridement and antifungal therapy.
Our patient was preterm, LBW at the time of presentation and had NICU stay of about 10 days before he developed feeding intolerance. He was explored with the suspicion of NEC, as happens in many cases, but was found to have colonic mycormycosis only on histopathological examination of the resected colon. Though, he was started on antifungal therapy on day 16 of life, the sepsis was overhelming and baby could not withstand it.
To conclude, colonic mucormycosis should be suspected in any preterm neonate with clinico-radiological features of NEC and non-response to conservative line of management involving antibacterial therapy.5 As the diagnosis is based on histological examination, in most of the cases, maintaining strict aseptic precautions in neonatal nurseries, a high index of suspicion for mucormycosis, early laparotomy, aggressive surgical debridement, early processing of the specimen for histopathological evaluation and early institution of antifungal drugs would go a long way in treating these neonates.
We gratefully acknowledge the assistance of Dr. Anita Kalaskar, Associate Professor from department of Pathology, for preparation and interpretation of the histology slides.
The authors declare no conflicts of interest.

©2017 Bhosale, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.