Journal of
eISSN: 2373-6410


Case Report Volume 1 Issue 6
1Guilan University of Medical Sciences, Iran
2Department of Neurosurgery, Guilan University of Medical Sciences, Iran
Correspondence: Shervin Ghadarjani, Department of Neurosurgery, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran, Tel -3227379
Received: September 19, 2014 | Published: October 3, 2014
Citation: Emamhady M, Ghadarjani S. Rapid spontaneous resolution of acute cranial subdural hematomas - two case reports. J Neurol Stroke. 2014;1(6):178-180. DOI: 10.15406/jnsk.2014.01.00035
Acute cranial subdural hematoma (aSDH) is the consequence of traumatic brain injury, which most of them require immediate surgical intervention, especially when they have more than 10 mm of thickness. There are, however, reports of spontaneous resolution in some cases who were considered for conservative treatment. Two important mechanisms explained for this spontaneous resolution are “blood push-out” and “blood wash-out”. In this article, we discuss two cases of spontaneous resolution of acute cranial SDH, in addition to the reviewing proposed theories. It is possible to consider conservative management with ICU care for such patients if clinical and para-clinical conditions support this decision.
Keywords:Acute, Redistribution, Spontaneousresolution, Subduralhematoma, Cranial
aSDH, acute Subdural Hematoma; GCS, Glasgow Coma Scale; CT, Computed Tomography; MRI, Magnetic Resonance Imaging; ICU, Intensive Care Unit
Acute Subdural Hematoma (aSDH) is the consequence of major trauma and occurs in 10-20% of all trauma cases, with a mortality rate of 50 to 85%.1 The most common sites for aSDH are: fronto-parietal convexity, middle cranial fossa, and inter-hemispheric fissure.2 Approach to an aSDH can be made based on the features of the hematoma on CT scan (i.e. A hematoma with a thickness greaterthan10mmor a midline shift greater than 5 mm almost always needs emergent surgery).3,4 On the other hand, conservative treatment is considered for anaSDHwith3mmorlessindiameter. There is, however, controversy for an intermittent group of patients, in whom the hematoma has a thickness of5–10mmand their Glasgow Coma Scaleis between9 and 13.
Most of these intermittent cases will undergo urgent neurosurgical intervention,2 but there are rare reports of spontaneous resolution of an acute SDH,5-20 hence, a true estimate of their incidence is not available.The time required for spontaneous resolution in these reports differed between a few hours and a few days after injuries,5-16, 18-21 There are also reports of spontaneous resolution in patients with chronic SDHs.22,23
In this article, we represent two cases of adult patients with post-traumatic aSDH, which were spontaneously resolved. We will also review some mechanisms described for this phenomenon.
Case 1
A 17 years old man was transferred to our hospital with a GCS score of 13 with the history of recent high-speed motor vehicle accident. The head CT scan demonstrated an aSDH with 1cm thickness in the left fronto-temporal area with 1 mm midline shift (Figure 1A).
Based on the general status of the patient and the relative high GCS score, he was considered for close monitoring. Another head CT scan was obtained approximately 6 hours later, which showed almost complete resolution of the SDH. The level of consciousness of the patient, also, maintained constant (Figure 1B). On next days, he progressively became more alert and was discharged, 7 days after his admission, without neurological deficits. He was visited at follow-up clinic two weeks later with no neurological deficits.
Case 2
A 17-year-old female was admitted to the emergency room after being involved in a high-speed motor vehicle accident with the initial GCS score of 12. Her regular blood work-up were within normal range. A head CT scan showed a right-sided fronto-temporal SDH (10 mm in its largest diameter) (Figure 1C), which was completely resolved in the control CT scan obtained 6 hours later (Figure 1D).
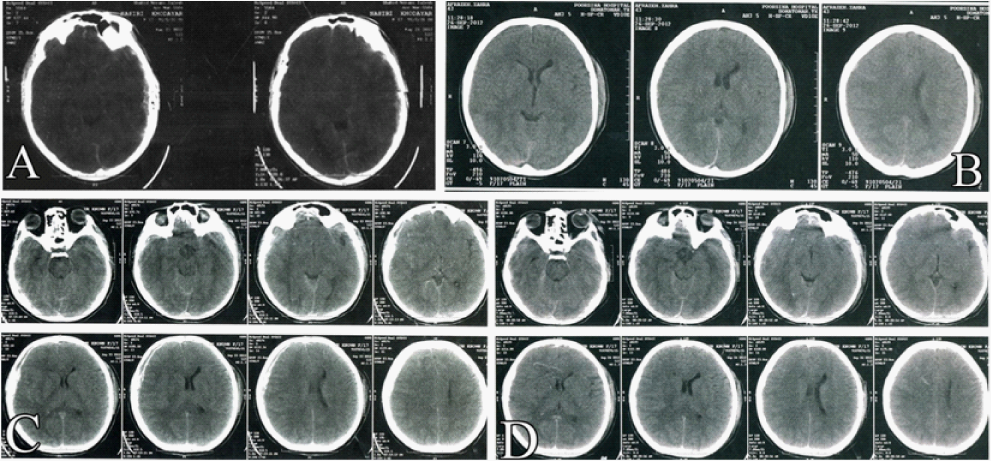
Figure 1 A. Case 1 Brain CT on admission and B. at 6 hours later. C. Case 2 Brain CT on admission and D. at 6 hours later.
She became progressively more alert and finally discharged from the hospital ambulatory and neurologically intact seven days after her admission.
The presence of an aSDH with a thickness more than 10 mm needs emergent surgical intervention, especially in the presence of loss of consciousness, mydriasis, or other neurological deficits.3-5 But there are reports of some spontaneous resolutions of acute SDH which happened between first 2 and 72 hours after the initial diagnosis.5-15,18-21,24-30 There are generally two important theories explaining this phenomenon:“CSF wash-out effect” through a tear in the arachnoid membrane,27 and “hematoma push-out” via a tear in Dura.26
It has been demonstrated that most cases of acute SDHs also have arachnoid tears permitting the CSF to transfer into the subdural space.31 The former theory explains that CSF comes out from these tears, washes the clots out, and this liquefied blood clot is redistributed to the subdural and subarachnoid spaces.12,15, 24,27,31 This is shown by the presence of a low-density band between the subdural hematoma and inner table of the skull, and could be considered as a useful sign for a good prognosis.21 This mechanism is also supported by MRI findings27,31,32 that, redistribution of subdural hematoma was seen over both the cerebral convexities and the tentorium, forming a very thin and sharply demarcated layer.15,27 Some studies demonstrated a sub-acute spinal SDH after the spontaneous resolution of an acute cranial SDH.6,7 There is electron microscopic evidence of anatomical continuity of the intracranial and spinal subdural spaces.33 These support the theory of redistribution of “blood clot-CSF” mixture to more dependent areas.6,7 We had not, unfortunately, an MRI confirmation for our patients to assess this theory.
The latter theory explains that the aSDH is being forced out of the subdural space via a tear in overlying Dura,20,26 or even to extra-cranial space via a fracture in the skull.16,34 The force for exiting the hematoma is made by the edema which has been shown to occur within 20–60 min after a severe head injury.35,36 In our series, however, no skull fractures were seen on the obtained CT scans.
Factors in favor of spontaneous resolution of subdural hematomas are: less than 30 mL of volume, fronto-temporal or temporo-parietal hematomas near the Sylvain fissure, association with iso-dense or hypo-dense space between the hematoma and the intracranial wall on CT scan, and association with cerebral edema and/or contusion and laceration, in neurologically stable patients of young age.3 It has been suggested that the young elastic brain parenchyma facilitates forcing out of the subdural brain clot,7,15,18 although, the presence of cortical atrophy is considered as a facilitator factor.8,9,15,32
For the patients planned to undergo conservative management, close monitoring in an ICU is of importance. In addition, serial head CT scans are necessary for detecting any changes in the size of the SDH or finding any other concomitant brain injuries. It is apparent that any deterioration in the clinical neurological examination or changes in the appearance of the SDH on CT scan represents strong indications for emergent surgery.
None.
None.

©2014 Emamhady, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.