Journal of
eISSN: 2373-6410


Case Report Volume 7 Issue 1
1Neurology, Sincan Nafiz Korez State Hospital, Turkey
2Institute of Neurological Sciences and Psychiatry, Hacettepe University, Turkey
3Department of Medical Genetics, Ankara Numune Training and Research Hospital, Turkey
4Department of Neurology, Ankara Numune Training and Research Hospital, Turkey
Correspondence: Aslihan TASKIRAN SAG, Institute of Neurological Sciences and Psychiatry, Hacettepe University, Sihhiye, Ankara, Turkey, Tel +90312 3052130
Received: January 15, 2017 | Published: June 27, 2017
Citation: Altas S, Sag AT, Cavdarli B, Oztekin N (2017) Multiple Sclerosis in a Patient with Psudopseudohypoparathyroidism. J Neurol Stroke 7(1): 00229. DOI: 10.15406/jnsk.2017.07.00229
Multiple sclerosis and pseudopseudohypoparathyroidism have not been reported in the same patient before. Here, we present a case that was diagnosed as multiple sclerosis and appeared to have a form of osteodystrophy that was not known to her before. A 30-year old woman admitted with right hemiparesis and diagnostic work-up showed bilateral multiple demyelinating lesions in brain MRI. Cerebrospinal fluid examination revealed oligoclonal band positivity and IgG index was 0,76. Pulse steroid treatment was started and the patient recovered completely. Besides, her phenotype was remarkable on physical examination. She had short stature, brachydactyly, round face, short neck and obesity. She looked like her father, who had died a few years ago, in physical appearance. Radiological evaluation of the hands revealed short 4th and 5th metacarpals. She had been operated for scoliosis. On suspicion, she was evaluated for endocrinopathies with skeletal abnormalities and the final diagnosis for the patient was pseudopseudohypoparathyroidism. Whether this is a coincidence or there is a linkage between these two disorders remains uncertain.
Keywords: multiple sclerosis, pseudopseudohypoparathyroidism, demyelinating disease, osteodystrophy
MS, multiple sclerosis; CSF, cerebrospinal fluid; CT, computerized tomography; MRI, magnetic resonance imaging; PPH, pseudopseudohypoparathyroidism; AHO, albright’s hereditary osteodystrophy; CNS, central nervous system
The coexistence of multiple sclerosis and pseudopseudohypoparathyroidism (PPH) is not reported in the literature till now. Here, we document an adult female who presented with a demyelinating attack and had features of PPH, finally diagnosed with multiple sclerosis.
A 30-year old woman admitted to the emergency department with a complaint of sudden weakness in her right arm and right leg. She had right hemihypoesthesis and 4/5 (MRC scale) right motor deficit on neurological examination. While there was no pathological sign in the initial brain CT scan, a hypodense area that was interpreted as an infarct was seen in the right posterior periventricular white matter in the control CT scan. Detailed studies were started for the etiology of stroke in a young patient. There was a 40 % stenosis in the left internal carotid artery in CT angiography. Cardiological studies (transthorasic echocardiography, holter test), lipid profile, homocysteine level, procoagulant factors and serological biomarkers of vasculitis were all in normal ranges.
Cranio-cervical MRI revealed T1-iso/hypointense, T2- and FLAIR hyperintense demyelinating lesions located in the right side of bulbus and pons, and in the bilateral periventricular white matter; large demyelinating lesions with marked contrast enhancement in the left supraventricular white matter and right frontal subcortical white matter; thinning in the corpus callosum and a demyelinating lesion in the dorsal of the spinal cord at C3 vertebral level. In the CSF analysis, IgG index was 0,76 (0,28-0,66) and oligoclonal band was detected. There were 8-10 erythrocytes and 10 leucocytes in the CSF microscopy. There was no atypical cell. Visual evoked potentials and sensory evoked potentials were in normal ranges. The patient was diagnosed as multiple sclerosis. Intravenous methylprednizolone 1 g/day was given for 5 days. The deficits disappeared in the follow-up of the patient. Immunomodulatory therapy was started.
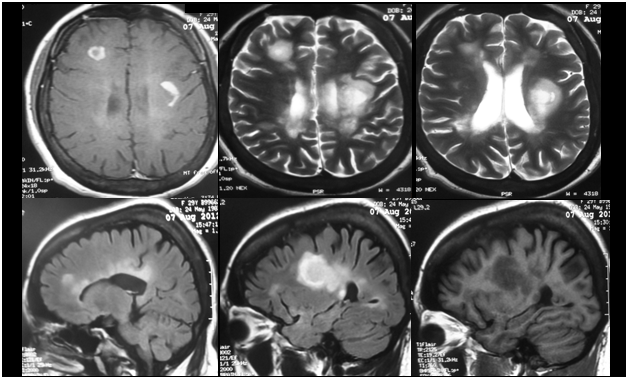
Figure 2 MRI of the patient revealing contrast-enhancing (upper left), T2-hyperintense (upper middle and right), FLAIR-hyperintense (lower left and middle) and T1-hypointense demyelinating lesions.
The patient had a dysmorphic round face, bradydactyly, scoliosis, obesity and short stature. There was no chromosomal anomaly in cytogenetic analysis. The patient had bone deformities and her father had also had similar phenotypic features. The patient was presumed to have pseudopseudohypoparathyroidism and further biochemical and radiological investigations were hold. Serum calcium, ionized calcium and phosphate levels were in normal ranges. Parathormone level was also normal. The diagnosis of pseudopseudohypoparatirodism was established regarding the normal calcium homeostasis and possible paternal inheritance.
The patient presented with a clinical demyelinating attack, and had multiple demyelinating lesions characterizing dissemination in time and space. Positive CSF findings of the patient supported the diagnosis. The physical examination of the patient revealed findings such as short stature, round face, shortness and wideness in long bones of hands and feet (bradydactyly), obesity and scoliosis. These constitute some of the somatic features of Albright’s Hereditary Osteodystrophy (AHO), or pseudohypoparathyroidism Ia. If parathormone resistance does not accompany these features, the disease is called pseudopseudohypoparathyroidism. It was first described in 1952 by Albright et al..1 The disease results from diminished Gs (stimulatory G protein) α subunit activity and mutation in the GNAS gene on the paternal copy is the underlying cause of haploinsufficiency.2-4 Our patient was biochemically normal and the family history suggested a possible paternal inheritance of PPH.
The coexistence of this genetic disorder and demyelinating disease is not published before. There is a single report of an autopsy case, which presents a young patient having PPH and chronic inflammatory demyelinating polyneuropathy, in the literature.5 However, central nervous system demyelination is not reported. Whether there is causality or a correlation between these rare disorders remains unknown. The fact that GNAS gene (20q13.32) is located in close proximity with some of the MS susceptibility gene loci is noteworthy and warrants further investigation.6
None.
None.
None.

©2017 Altas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.