eISSN: 2373-6372


Research Article Volume 5 Issue 5
1General surgery department, CHU Blaise Compaoré, Burkina Faso
2Radiology department, Hôpital de District de Bogodogo, Burkina Faso
3General surgery department, CHU Yalgado Ouédraogo, Burkina Faso
Correspondence: Sanou Adama, General surgery department, CHU Blaise Compaoré, Burkina Faso
Received: August 15, 2016 | Published: November 25, 2016
Citation: Ouedraogo NA, Bambara HA, Zongo N, SissokoML, Kambou BMAT, et al. (2016) Primary Liver Cancer, Ultrasound and CT scan Aspects. Gastroenterol Hepatol Open Access 5(5): 00156. DOI: 10.15406/ghoa.2016.05.00156
Introduction: Primary malignant tumors have an important place in the liver disease in Burkina Faso. Objectives: To describe aspects in ultrasound and CT scan of primary liver cancer at Ouagadougou.
Materials and methods: Retrospective study conducted on 7 years in 4 referral health centers in Ouagadougou. Patients witch present liver cancer with radio‒biological and / or histological evidence was included.
Results: We collected 233 primary malignant liver tumors. The average age was 46 years. Male dominance was marked with a sex ratio of 3.9. The alpha‒fetal protein level was greater than 400 UI/L in 75.7% of cases and HBs Ag was positive in 80.4% of cases. Abdominal ultrasound had found multiple nodules in 65.5% of cases with an average size of 107.3 mm and a portal invasion in 34.7% of cases. Enhancement of lesions in the liver CT scanner was highly suggestive in 77% of cases. Histological confirmation was made in 44 cases (18.8%) in liver biopsies. There were 42 cases of hepatocellular carcinoma (95.5%).
Conclusion: The primary liver cancers are common in our context and diagnosed at a late stage. Viral hepatitis B often seems concerned. Awareness is essential to improve the prevention and access to surgery.
Keywords: primary tumor, liver cancer, hepatocellular carcinoma, ultrasound‒CT scanner
Primary liver cancer is the sixth most common cancer worldwide and the third leading cause of cancer deaths.1 In Africa, it is the second cancer in men and the third in women.2 In Burkina Faso, liver cancers dominate digestive tumors. The most frequent etiology seems to be infection with hepatitis B virus. In fact, according a study in Burkina Faso about the health workforce in 2010, the prevalence of HBS antigen was 13.8%.3
The prognosis is even worse than they are often discovered late, limiting treatment options. The role of imaging is, to suggest the diagnosis by identifying liver damage, doing the staging and contributing to the positive diagnosis by performing liver biopsies for micro‒histological confirmation. Otherwise imaging is important in the achievement of certain curative (radio frequency) or palliative (chemo embolization) therapeutic procedures of malignant liver tumors.4 The objective of this study was to describe the aspects of imaging, including ultrasound and CT scan of the primary malignant liver tumors and highlight their pathological aspects.
We conducted a descriptive cross‒sectional study, covering a period of seven years (1 July 2008 to 31 June 2014). Four referral health centers in the city of Ouagadougou, capital of Burkina Faso, were interested by this study. Were included, a subject of both sexes, with a primary malignancy of the liver witch was diagnosed on histological arguments (liver biopsy) or a combination of imaging and biological arguments:nodular liver on ultrasound or computed tomography (CT) suggesting a malignancy associated with a higher rate of alpha‒fetoprotein to 10 UI/L. We have compiled 233 cases of primary malignant liver tumors. Data were analyzed using Epi‒Info in its 7.0.9.7 version Excel 2013. The alpha‒fetoprotein rate was considered negative when it was less than 10 UI/L, suggestive between 10 and 400 UI/L and very suggestive at levels greater than 400 UI/L.
The average age of patients was 46 + 12 years and the most represented age group was the 30 to 50 years (55.8%). There were 186 men (79.8%) and 47 women (20.2%) with a sex ratio of 3.9. The tumor was discovered following symptoms in 203 cases (87.1%) at monitoring of cirrhosis in 26 cases (11.2%) or at a checkup in 4 cases (1.7 %). HBsAg was positive in 156 patients (80.4%). Abdominal ultrasound was performed in 225 cases (96.5%). There was hepatomegaly in 198 cases (88%) and liver nodules were noted in 215 cases (95.6%). The distribution of cases of primary carcinoma of the liver (CPF) in the number of nodules and their headquarters in ultrasound is noted in Table 1. The mean nodule size was 107.3 mm (range 8‒214 mm) and nodules were hyperechoic in 202 cases (89.7%). We noted the presence of an effusion intraperitoneal in 119 cases (52.9%). Liver cirrhosis (hepatic dysmorphia, irregular contours, micro nodular appearance) was found in 110 patients (47.2%). All patients with ultrasound signs of cirrhosis were positive for HBsAg. A tumor invasion in the venous system was found in 77 cases in the portal vein (34.2%) and 1 case in the inferior vena cava (0.4%) (Figure 1). Deep adenomegalies were visualized in 16 (7.1%).
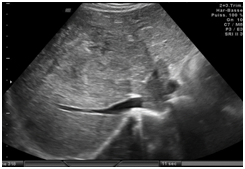
Figure 1 Ultrasound cutt through the hepatic veins. The tumor is heterogenous and locatein the segments IVand VIII (yellow arrow). It invaded themediane and left hepatic veins and the inferior cava vein (withe arrow).
|
Ultrasound Characteristics of Nodules |
Effectifs |
Frequency (%) |
|
|
Number |
Multiples |
148 |
65.8 |
|
2 or 3 nodules |
9 |
4 |
|
|
Unique |
68 |
30.2 |
|
|
Location |
Diffuse |
129 |
57.3 |
|
Right liver |
65 |
28.9 |
|
|
Left liver |
31 |
13.8 |
|
Table 1 Distribution of primary liver cancer cases in ultrasonography depending on number and location of nodules
Abdominal CT scan was performed in 79 patients (34%). It was performed in conjunction with ultrasound in 71 patients (90%). There was hepatomegaly in 70 patients (88.6%). The nodules were noted in 76 cases (96.2%), with an average size of 98.9 mm (range 13 to 223 mm). The distribution of lesions according to the number of nodule and headquartered in CT is noted in Table 2. Early contrast enhancement during the arterial phase, with a washing portal phase was present in 61 cases (77.2%) Figure 2. These aspects were not specified in 16 cases (20.2%). The nodules were hypo‒vascular in 2 cases (2.6%). The effusion intraperitoneal was visualized in 30 cases (38%). The presence of a venous invasion was noted in 22 cases (27.8%). Deep adenomegalies were present in 9 cases (11.4%). The alpha‒fetoprotein levels were performed in 230 cases (88.1%). The rate was very suggestive in 174 cases (75.7%), reminiscent in 38 cases (16.5%) and negative in 18 cases (7.8%). Histological confirmation was performed in 44 cases (18.8%). Hepatocellular carcinomas (HCC) accounted for the majority of the lesions found in 42 cases (95.5%). Of these lesions, 33 were poorly differentiated, moderately differentiated 4 and 5 well differentiated. We also noted one case of fibro‒lamellar carcinoma and 1 case of cholangio carcinoma. The staging had identified 18 cases (8%) of lung metastases (13 cases of 37 chest X‒ray front and 5 cases of 7 chest CT).

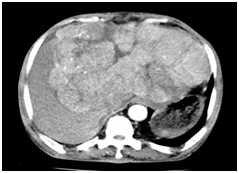

Figure 2 Axial cuts in CT scan of liver.
|
Characteristics of Nodules in CT Scan |
Effectifs |
Frequency (%) |
|
|
Number |
Multiples |
40 |
50.6 |
|
|
2 or 3 nodules |
6 |
7.6 |
|
Unique |
33 |
41.8 |
|
|
Location |
Right liver |
42 |
53.1 |
|
|
Left liver |
11 |
13.9 |
|
Diffuse |
26 |
33 |
|
Table 2 Distribution of primary liver cancer cases in CT scan depending on number and location of nodules
Liver primary cancers in Africa are the second leading cause of cancer in men and the third cause in women.2 The average age of our sample is similar to that found by Nikièma in Burkina Faso and Sylvester in Nigeria, which founded respectively 45.6 and 43.7 years.5,6 In Europe, the average age appears higher, goshawks 60 years.7 Probably due to the difference of etiological factors of this disease, according to geographical areas. Indeed, in Africa the hepatitis B virus (HBV) is the most commonly involved; there is a strong transmission from mother to child with a chronic carriers of HBs Ag in young adults (HBs Ag positive in 80.4%). This may explain the occurrence of cancers in younger populations, in midlife.8 While in Europe, the HCC is often secondary to alcoholic cirrhosis or post transfusion related to hepatitis C (HCV).9 As in several studies, male dominance was clear in our serie highlighting greater exposure of men with risk factors for HCC.10,11 The appearance of cirrhosis was found in almost half of cases (47.2%), and the rate of HBs Ag was positive in 80.4%. These results are consistent with several studies showing the association between HBV infection, cirrhosis and HCC.8 Ntagirabiri in Burundi had highlighted a 9 times higher risk of developing HCC when cirrhosis is present.12
Ultrasonography and CT scan had shown that the primary malignant liver tumors occurred most often in the form of hepatomegaly multi nodular in Ouagadougou. These hepatic nodules were explored at a late stage, mainly to the onset of symptoms (87.1% of cases). This is corroborated by the large size of the nodules in the first radiological investigation. Indeed, the nodules in our sample had an ultrasound average size of 107.3 mm. The importance of the average size of liver nodules in our sample contrasts with that found on average in Europe, which is about 3 cm.13 This difference can be explained by regular preventive monitoring of patients at risk in Europe, accessibility and availability of means of explorations in medical imaging such as ultrasound, ultrasound contrast, CT scan and MRI. In our context by cons, even when the preventive monitoring is possible and available, in current practice, patients are seeking care centers after practicing self‒medication and traditional treatments, allowing tumors to grow in this time interval. Vascular invasion is another element that confirms the advanced stage of the CPF, as noted in our cases. There was a portal invasion in 34.2% of cases. These results are in agreement with those of Nikiéma and Kyelem in Burkina Faso and Bouglouga in Togo.5,14,15
The typical enhancement of HCC, namely hyper vascularization in the arterial phase and washing in the portal time was found in 77% of cases. The appearance hyper vascular HCC is explained by the loss of portal vascularization during the evolution of cirrhotic nodules, replaced by a neo‒angiogenesis.16 HCC irrigated by hepatic artery, thus sees its maximum enhancement in the arterial phase (wash in) unlike the rest of the liver, which receives its blood supply primarily from the portal system has a maximum increase in venous time. The relative hypo density of the tumor in venous time is called wash out or washing. Whatever, there are genuine HCC does not obey this principle named hypo vascular tumors, expressed in 20% of cases.17 Some authors suggested a correlation between the degree of tumor vascularization and the dedifferentiation of the tumor.18 These HCC hypo vascular be worse17 prognosis.
The alpha‒fetoprotein level was very suggestive in 75.7%, in agreement with Bagny et al who found themselves a significant elevation of alpha‒fetoprotein levels in 90.9% in their sample.8 However, this hormone is not specific to malignant liver tumors and can be raised under germ or gastrointestinal tumor. Although the cross‒sectional imaging with contrast medium injection associated with elevated alpha‒fetal protein, can be strongly suggestive of the diagnosis, histology remains the gold standard for the definitive diagnosis of hepatocellular carcinoma.4 In cases where the tumor enhancement is not typical or the alpha protein rate is not suggestive, a micro hepatic biopsy is indicated.15 Besides, after encouraging the methods of non‒invasive detection of HCC based on contrast imaging and alpha‒fetoprotein levels, there is a return of liver biopsy for histological confirmation, to prevent false positives one hand and participate in therapeutic research.4 Liver biopsies performed helped to highlight the preponderance of HCC samples (95.5%), in agreement with Nikiéma in Burkina Faso who found a rate of 90% in its5 sample. The other cases were represented by fibro lamellar carcinones and cholangiocacinome. The results of loco‒regional extension found a secondary preferential localization to the lung in agreement with Ayol et al.19
This study highlighted that infection with hepatitis B virus and presence of cirrhosis are important risk factors for primary malignant liver tumor at Ouagadougou. These tumors are diagnosed late, evidenced by the major cases of large hepatocellular carcinoma, within multi nodular hepatomegaly. These advanced stages often limited treatment options available in our context and are mostly very poor prognosis for the patient. Then it is important to raise awareness about the reality of infection whith hepatitis B, taxed of "forgotten epidemy" and "time bombe" by Feray.20
None.
None.

©2016 Ouedraogo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.