eISSN: 2377-4304


Case Report Volume 8 Issue 1
1Department of Obstetrics and Gynaecology, Sikkim Manipal Institute of Medical Sciences, Gangtok, India
2Department of Radiodiagnosis, Sikkim Manipal Institute of Medical Sciences, Gangtok, India
3Department of Pathology, Sikkim Manipal Institute of Medical Sciences, Gangtok, India
Correspondence: Hafizur Rahman, Professor of Obstetrics & Gynecology, Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok, Sikkim-737102, India, Tel 919733400336(R); +913592-231137/232041 (128), Fax 91-3592-231496
Received: August 03, 2017 | Published: September 27, 2017
Citation: Rahman H, Sharma BK, Sherpa ML, Khalda E (2017) Ruptured Primary Ovarian Pregnancy Presented in Advanced Gestation without Amenorrhoea: A Rare Case Report. Obstet Gynecol Int J 8(1): 00275. DOI: 10.15406/ogij.2017.08.00275
Primary ovarian pregnancy is one of the rarest types of ectopic pregnancy where the gestational sac is implanted within the ovary and its incidence ranges from 1:6000 to 1:40 000 pregnancies. Its presentation often is difficult to distinguish from that of tubal ectopic pregnancy and hemorrhagic ovarian cyst. Spigelberg criteria are historically used for diagnoses which are based on surgical and histopathological observations. Management is surgical despite the advance in medical treatment. We present a rare case of ruptured primary ovarian ectopic pregnancy in which patient presented in advanced gestation without any history of amenorrhea.
Keywords: Ectopic pregnancy, Ovarian pregnancy, Tubal pregnancy
Primary ovarian pregnancy is one of the rarest types of ectopic pregnancy where the gestational sac is implanted within the ovary. It accounts for 0.5% to 1% of all ectopic gestations,1 and its incidence ranges from 1:6000 to 1:40 000 pregnancies. It is responsible for 10% of pregnancy related deaths. In recent years, there has been an increase in the incidence of ovarian pregnancies due to better diagnostic modalities and wider use of intrauterine contraceptive device (IUCD), ovulatory drugs, assisted reproductive techniques such as in vitro fertilization.2
A 28 year old gravid 2 para 1 living attended emergency department of our hospital complaining of pain in the abdomen for one day and light vaginal bleeding for one hour duration. She did not give any history of amenorrhea even after repeated enquiry and her previous menstrual cycles were reported to be normal in amount, duration and flow. She gave no history of sexually transmitted disease, pelvic inflammatory disease or any previous gynecological surgery. Her first pregnancy was a spontaneous conception and she had a full term normal vaginal delivery which was a hospital delivery. There were no post partum complications and no history of contraceptive use.
Physical examination revealed she had moderate pallor with pulse 104beats/min, low volume, blood pressure 80/40mmHg, and body temperature 37.4◦C. On speculum examination there was a small amount of dark coloured vaginal discharge but the cervical os was closed. On bimanual examination her uterus was of normal size anteverted and cervical motion tenderness was present. The right adnexa were tender on palpation but no adnexal mass could be elicited. A urine pregnancy test was done as a suspicion which reported positive.
An urgent ultrasonography was done, which reported Single gestational sac with a foetal pole of 9weeks 1day in right adnexal region close to right ovary. Foetal cardiac activity was not present (Figure 1). Uterus was normal in size and echotexture with normal endometrial thickness (Figure 2a). Gross free fluid was noted in peritoneal cavity which on ultrasound guided aspiration came out to be blood suggesting hemoperitoneum (Figure 2b). Ultrasonographic features were consistent with ruptured right adnexal ectopic gestation with possibility of ruptured right ovarian ectopic pregnancy. Her initial blood results were Blood group B positive and Hemoglobin (Hb) 8.7 gm%.
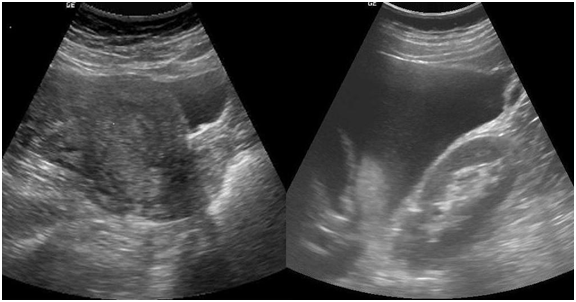
Figure 2 2a-ultrasonography showing uterus with normal endometrial cavity. 2b-ultrasonography showing gross hemoperitoneum.
She was rushed for emergency laparotomy. On exploration of abdomen approximately 1.5 liters clotted blood were removed from peritoneal cavity. A recently ruptured ovarian pregnancy was noted with placenta still attaching to ovary (Figure 3). Right ovary was actively bleeding to which gestational sac and embryo was found partially attached. Initially wedge resection was tried, but since haemostasis couldn’t be achieved, so right sided ovariotomy was performed. Right side fallopian tube was found to be completely normal and separate from ovary. The left ovary and left fallopian tube were also normal.
Intra operative and immediate postoperative patient received 2 units of blood transfusion. Her postoperative period was uneventful and was discharged 3 day after operation. On histopathological examination, villous structures embedded in the ovarian tissue were seen, which was confirmatory of primary ovarian pregnancy (Figure 4).
Primary ovarian pregnancy is one of the rarest types of ectopic pregnancy. The cause of primary ovarian pregnancy is exactly not known, and it may be secondary to reflux of the fertilized oocyte to the ovary.3 Bouyer et al.4 reported that ovarian pregnancy is neither associated with pelvic inflammatory disease nor infertility, unlike tubal ectopic gestation. The only risk factor associated with the development of ovarian pregnancy is the current use of intrauterine device.4 However in our case there was no history of use of any intrauterine device.
Spigelberg criteria are historically used for intraoperative diagnosis which include intact fallopian tube on the affected side, fetal sac must occupy the position of the ovary on the affected side, ovary connected to the uterus by ovarian ligament, ovarian tissue must be located in the sac wall, which is confirmed by histopathology.5 In our case all the criteria’s laid down by Spigelberg were present.
The signs and symptoms of ovarian pregnancy are similar to tubal pregnancy. Therefore, a differential diagnosis must be considered with tubal pregnancy, ruptured hemorrhagic corpus luteum, or chocolate cyst. With the improvement in ultrasonographic skills and instrumentation, a proportion of ovarian pregnancies can be diagnosed preoperatively.6 A gestational sac adjacent to the ovary can be seen or a double echogenic ring within a hypoechoic latero-uterine mass can be seen.7 The ovarian pregnancy is definitely diagnosed peroperatively. Misdiagnosis of this entity is common because it is confused with a ruptured corpus luteum in up to 75% of cases.8
The traditional method for management of an ovarian pregnancy is wedge resection or the removal of the effected adnexa by laparoscopy or laparotomy.9 Systemic methotrexate administration has become apparent in the recent years. But, it is not the first-line treatment of choice for ovarian pregnancy even if the patient is candidate meeting the criteria for medical treatment. In our case the patient was haemodynamically unstable so, an emergency laparotomy had to be performed.
Several surgical techniques have been described: ovarian wedge resection for ovarian pregnancy, ovarian pregnancy enucleation, corpus luteum cystectomy for the trophoblast, trophoblast curettage with coagulation or hemostatic suture of the bed of ovarian pregnancy10 with total conservation of the ovary. Occasionally due to the advanced development of pregnancy, ovariectomy and oophorectomy may be necessary11 as we had to do in our case as the pregnancy was more than 9 weeks gestation and ovary was badly damaged and profusely bleeding.
Recurrence of ovarian ectopic pregnancy is rare. A single case of recurrence of ovarian pregnancy has been described in the literature which involved the contra lateral ovary10 in contrast to approximately 15% recurrence risks of tubal ectopic pregnancies.12
Primary ovarian pregnancy is a rare entity that has some peculiarities. There might not be predisposing factor. Its diagnosis is difficult and relies on criteria based on intraoperative findings and confirmed on histopathology. Its management is surgical despite the advance in medical treatment. With the help of ultrasounds having better imaging quality it is now becoming more probable to make the diagnosis preoperatively.
None.
None.
Nil.

©2017 Rahman, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.