eISSN: 2377-4304


Review Article Volume 5 Issue 2
1Department of Obstetrics and Gynaecology, Catharina hospital, Netherlands
2Department of Radiology, Maastricht University Medical Center, Netherlands
3Department of Radiology, Catharina hospital, Netherlands
4Department of Pathology, Catharina hospital, Netherlands
Correspondence: JMJ Piek, Department of Obstetrics and Gynaecology, Catharina hospital, Netherlands
Received: July 29, 2016 | Published: September 21, 2016
Citation: Benali F, Gooszen AD, Wetzels C, et al. Cyst of nuck: the importance of histopathological evaluation. Obstet Gynecol Int J. 2016;5(2):303-308. DOI: 10.15406/ogij.2016.05.00152
A cyst of Nuck or hydrocele of Nuck, also called the forgotten diagnosis,1 is a rare anatomical anomaly in women. Because of its rarity it is often misdiagnosed and due to the treatment pittfalls it is important to properly diagnose this tumour. Clinical examination and imaging must be performed to differentiate and diagnose the cyst correctly. However, even these modalities are not specific enough as we present in this case of a 28 year old woman with a suspected abscess of Nuck that was shown to be a cyst of Bartholin by histopathological examination. Furthermore, we reviewed the literature on this subject.
The canal of Nuck was first described in 1691 by Anton Nuck, a Dutch anatomist.2 During the embryological development the gubernaculum is responsible for the descent of the ovary from high in the abdomen to the inguinal canal. Eventually the gubernaculum attaches to the labium major. Inferior and superior remnants of the gubernaculum develop respectively into ligament teres uteri, also called the round ligament and ligamentum ovary iproprium (Figure 1).
As the teres ligament evaginates out of the abdominal cavity into the inguinal canal it is covered by parietal peritoneum. This structure of peritoneum in the inguinal canal is called the canal of Nuck. The canal of Nuck also holds the ilio-inguinal nerve and the genital branch of the genitor femoral nerve.
In most cases, the canal of Nuck obliterates before birth. The cause of this obliteration is unknown, but some studies show that the calcitonin-gene related peptide (CGRP), that is being released from the genitofemoral nerve, plays a role.3 However, in some cases there is incomplete obliteration or even no obliteration at all. This can cause cases a non-communicating cyst or even a communicating hernia in guinalis. The fluid inside the cyst of this canal of Nuck is a result of disbalance between production and absorption of fluid produced by the parietal peritoneum.4
A cyst of Nuck is a rare entity. The incidence is not exactly known but literature estimates an incidence of 1% in young girls.5 However, this might be an underestimation, since the cyst might be misdiagnosed.
A 25 year old null gravid with no medical history presented with a painful vulvar swelling superior lateral of the right major labium of approximate four centimetres in diameter. The swelling fluctuated and was red. This swelling was present since one month, however the intense pain was present since three days. There was no history of fever. On examination an in durated, red frontal part of the labium with swelling of the tissue between the top of the labium and the inguinal canal was seen. No enlarged inguinal lymph nodes were palpable. The Valsalva manoeuvre was negative, further gynaecologic examination was impossible due to intense pain. Ultra sonography showed a fluid filled cyst of five centimetres in diameter in the upper part of the labium up to the inguinal canal, without positive Doppler flow.
The initial differential diagnosis consisted of an infected cyst of Bartholin, an infected cyst of Nuck, an infected lipoma, leiomyoma or a sarcoma. Since Bartholin glands are located slightly posterior and to the left and right of the opening of the vagina, an infected cyst of Nuck was our working diagnosis. Marsupialisation of the complete cyst wall was performed under general anaesthesia. The cyst wall was located in the upper part of the labium and ended in the direction of the right inguinal canal. Afterwards a redon-drain was placed and the wound was closed. Post-operative there were no complications except for pain. This was treated with tramadol, ibuprofen and pantoprazol. One day postoperatively, the patient was discharged. The drain remained for two days. On follow up after one week, the wound was closed and healing properly. Microbiological investigation of the pus showed no chlamydia, Neisseria gonorrhoea, mycoplasma genitalium or trichomonas vaginalis. Histological examination revealed fragments of a cystic lesion adjacent to normal Barholin’s gland acini. The cyst wall was partially lined by a stratified squamous, transitional and columnar epithelium. There was a moderately to heavy active inflammatory component causing erosion and abscess formation (Figure 2).

Figure 2A. Heavily inflamed cyst wall with columnar, transitional and stratified squamous epithelium. (HE, 10x magnification).
B. Erosive part of the cystic wall. (HE, 10x magnification)
C. Active inflammation with abscess formation. (HE, 20x magnification)
D. Lobules of Bartholin’s gland acini adjacent to the cyst. (HE, 2,5x magnification)
Literature search
A pubmed search was performed with mesh term: “nuck” untill June 2016. A total number of 72studies are mentioned in literature. Forty-six cases are on a hydrocele of Nuck/infected cyst of Nuck.5,9–51 Thirteen cases on endometriosis in a cyst of Nuck.52–61 One case of an ectopic pregnancy62 as well as six cases on herniation of Nucks’ duct are described.63–68 Furthermore, one case of angiofibroblastoma69 and one case of angiomyofriboma,70 two cases of adenocarcinoma71,72 and two cases of haematocole of Nucks’ duct73,74 are described. All articles were analysed for complaints at presentation, whether histopathological investigation was done and which radiological investigation was done (Table 1). This information was available in 32 of the studies. In only Fifty-six percent (18 studies) histopathological investigation was performed.
|
Sarkar S et al.8 |
Complaint: Tender right in guino-labial swelling |
|
Histopathology: Yes |
|
|
Imaging modality: surgical exploration |
|
|
Patnam V et al.9 |
Complaint: Swelling was non-tender, cystic and irreducible. No cough impulse. |
|
Histopathology: No |
|
|
Imaging modality: CECT, MRI |
|
|
Heer J et al.11 |
Complaint: painless “boil” to the right groin, |
|
Histopathology: No |
|
|
Imaging modality: CT |
|
|
Kono R et al.12 |
Complaint: Swelling in the right inguinal region |
|
Histopathology: YES |
|
|
Imaging modality: MRI |
|
|
Mazzeo C et al.54 |
Complaint: Unknown |
|
Histopathology: No |
|
|
Imaging modality: MRI |
|
|
Husaric E et al.13 |
Complaint: Left sided groin swelling |
|
Histopathology: No |
|
|
Imaging modality: surgical exploration |
|
|
Hensgens RL et al.14 |
Complaint: Painful swelling in right groin |
|
Histopathology: No |
|
|
Imaging modality: surgical exploration |
|
|
Matsumoto T et al.22 |
Complaint: Painless and reducible swelling in left groin |
|
Histopathology: Yes |
|
|
Imaging modality: US and MRI |
|
|
Uno Y et al.55 |
Complaint: Lump in right inguinal region |
|
Histopathology: Yes |
|
|
Imaging modality: MRI |
|
|
Qureshi NJ et al.15 |
Complaint: Pain and swelling in left inguinal region |
|
Histopathology: Yes |
|
|
Imaging modality: US |
|
|
Noguchi D et al.67 |
Complaint: Painful swelling in right groin |
|
Histopathology: Yes |
|
|
Imaging modality: US, MRI |
|
|
Mandhan P et al.17 |
Complaint: Tender swelling in guino-labial swelling left |
|
Histopathology: Yes |
|
|
Imaging modality: US, MRI |
|
|
Jagdale R et al.16 |
Complaint: Painful swelling in right groin |
|
Histopathology: Yes |
|
|
Imaging modality: US |
|
|
Choi YM et al.19 |
Complaint: Inguinal groin with (case 1) and without (case 2) tenderness |
|
Histopathology: Case 1: No, Case 2: Yes |
|
|
Imaging modality: US and MRI |
|
|
Manjunatha Y et al.24 |
Complaint: Palpable mass in right inguinal region with occasionally pain |
|
Histopathology: Yes |
|
|
Imaging modality: MRI and US |
|
|
Bagul A et al.56 |
Complaint: Swelling in right groin with mild discomfort |
|
Histopathology: Yes |
|
|
Imaging modality: surgical examination |
|
|
Ozel A et al.25 |
Complaint: Inguinal groin right |
|
Histopathology: Yes |
|
|
Imaging modality: MRI |
|
|
Hernández Monge A et al.75 |
Complaint: Unknown |
|
Histopathology: Yes |
|
|
Imaging modality: Unknown |
|
|
Bhattacharjee PK et al.27 |
Complaint: Painless left groin swelling |
|
Histopathology: No |
|
|
Imaging modality: ultrasound |
|
|
Cervini P et al.59 |
Complaint: Mass overlying right pubis |
|
Histopathology: Yes |
|
|
Imaging modality: Ultra sonography |
|
|
Ameh EA et al.29 |
Complaint: Right groin swelling |
|
Histopathology: No |
|
|
Imaging modality: surgery |
|
|
Huang CS et al.30 |
Complaint: Asymptomatic palpable movable mass |
|
Histopathology: No |
|
|
Imaging modality: Ultra sonography |
|
|
Turpin F et al.61 |
Complaint: Unknown |
|
Histopathology: No |
|
|
Imaging modality: US and MRI |
|
|
Hernández-Monge A et al.75 |
Complaint: Unknown |
|
Histopathology: Yes |
|
|
Imaging modality: Unknown |
|
|
Laskin WB et al.74 |
Complaint: Painless mass Vulvar Region (15 cases) |
|
Histopathology: Yes |
|
|
Imaging modality: Unknown |
|
|
Josefsson ML et al.69 |
Complaint: Pelvic pain |
|
Histopathology: No |
|
|
Imaging modality: Ultra sonography |
|
|
Caviezel A et al.38 |
Complaint: Unknown |
|
Histopathology: Yes |
|
|
Imaging modality: MRI and Ultra sonography |
|
|
Wang CJ et al.63 |
Complaint: Tender mass in left groin |
|
Histopathology: No |
|
|
Imaging modality: Ultra sonography |
|
|
Jedrzejewski G et al.71 |
Complaint: Palpable movable mass in right inguinal region |
|
Histopathology: No |
|
|
Imaging modality: Ultra sonography |
|
|
Khanna PC et al.39 |
Complaint: Right inguinal pain and discomfort |
|
Histopathology: No |
|
|
Imaging modality: Ultra sonography |
|
|
De Meulder F et al.40 |
Complaint: Bulge in right groin |
|
Histopathology: Yes |
|
|
Imaging modality: Ultra sonography |
|
|
Miklos JR et al.44 |
Complaint: Painful vulvar mass |
|
Histopathology: No |
|
|
|
Imaging modality: Ultra sonography |
Table 1 Results of the literature review with data on complaints at presentation, whether histopathological evaluation was performed and what imaging modality was used
In the differentiation of causes of a vulvar swelling, imaging is of importance. In this case ultra sonography was used. This technique is seen as the golden standard for assessing swellings in the vulvar area6. This technique is simple, non-invasive and radiation free. Figure 3 shows examples from different patients from our population of MRI and ultrasound images from a cyst of Nuck and Bartholin. However, in this case the vulvar swelling was mistakenly taken for a cyst of Nuck, because of the anatomical location and the relation with the inguinal canal. It was only by histopathological examination that a cyst of Bartholin was diagnosed. We therefore urge histopathological examination of all removed vulvar swellings, because a cyst of Nuck might be even more rare, since most case reports in our literature search did not mention the results of the histopathological examination.
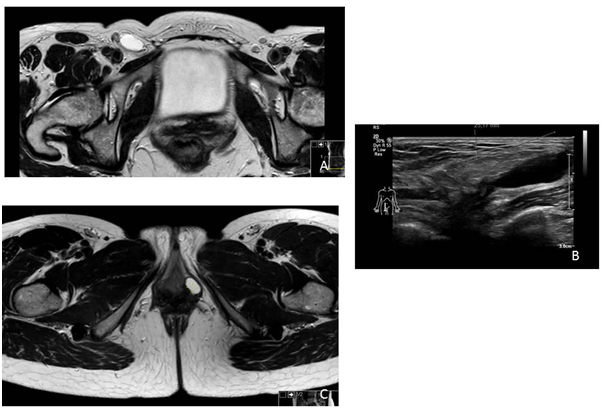
Figure 3
In all cases it is important to exclude vascularisation of the cyst, which can easily be done by ultra sonography. This can be a sign of a true inguinal hernia or a malignancy.7 Most prevalent malignancies in the vulvar area that have a similar presentation as a cyst of Bartholin or Nuck are liposarcoma, leiomyosarcoma, fibro sarcoma and undifferentiated sarcoma.6 An inguinal hernia is characterized by an hypo-echo genic mass usually containing intestines, omentum or other structures.
Ultra sonography has a place in the differential diagnosis of a vulvar swelling. However, as shown in the case report histopathological examination is always warranted when assessing cysts in the vulvar area.
None.
The authors declare there is no conflict of interests.
None.

©2016 Benali, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.