Journal of
eISSN: 2373-6410


Research Article Volume 5 Issue 1
Neurosurgery Department, Assiut University Hospital, Assiut, Egypt
Correspondence: Hassan Mohammed, Neurosurgery Department, Assiut University Hospital, Assiut, Egypt
Received: December 19, 2015 | Published: July 11, 2016
Citation: Mohammed H, Elsatar ABA, Ragab M, Alghriany A (2016) Evaluation of Late Onset Congenital Aqueductal Stenosis Hydrocephalus. J Neurol Stroke 5(1): 00163. DOI: 10.15406/jnsk.2016.05.00163
Early onset hydrocephalus due to congenital aqueductal stenosis is well known and fully studied. However, late onset one is not so. The present study is a trial to give spotlight on the late onset type which may be clinically confusing with other syndromes leading sometimes to mismanagement.
Our study included 25 patients with late onset congenital aqueductal stenosis hydrocephalus. They verified into 18 males (72%) and 7 females (28%). Their ages ranged from 5 years to 64 years. They presented with headache in 19 cases (76%), visual disturbance in 11 cases (44%), gait disturbance in 8 cases (32%) and disturbed level of consciousness in 4 cases (16%). Ventriculoperitoneal shunts were done for all cases with improvement in 20 cases (80%), no improvement in 3 cases (12%) and deterioration in 2 cases (8%). Post-shunt complications occurred in 9 cases (32%) and include 6 cases with subdural hematoma (24%), 2 cases with infection (8%) and one case with shunt obstruction (4%)
Late onset aqueductal stenosis hydrocephalus is not uncommon cause of hydrocephalus in our locality. Proper diagnosis and management of such patients depended on the well manifest clinical data confirmed with the neuroimaging studies became easy.
Keywords:Ventriculoperitoneal shunt, Aqueductal stenosis
Aqueductal stenosis is responsible for 20% of cases of hydrocephalus. Its incidence ranges from 0.5 to 1.0 in 1,000 births, with a recurrence risk in siblings of 1.0% to 4.5%. The onset of symptoms is usually insidious and can occur at any time from birth to adulthood. Associated malformations in neighboring structures are common The presence of these malformations helps to explain the intellectual, cognitive, and motor handicaps even after the hydrocephalus is compensated by shunting. Aqueductal obstruction constitutes three percent of adult hydrocephalus.1
According to the histopathological classification of Russell,1 non-tumoral aqueduct stenosis can be subdivided into four types: Stenosis, Forking, Septum formation and Gliosis. Congenital aqueductal stenosis can present later in adult age due to compensation of CSF flow dynamics during childhood and normalization of clinical symptoms are more important in evaluating the benefits of treatment than in the decrease in ventricular size.
Hydrocephalus secondary to aqueductal stenosis may present at any age. Clinical course may vary, according to the patient’s age and the anatomical deformation of the ventricular system. Imaging with CT and MRI will show dilated third and lateral ventricles with marked upward bowing of corpus callosum. Treatment of hydrocephalus secondary to aqueductal stenosis can be achieved with implantation of extracranial shunt, such as ventriculo-peritoneal (VP) or ventriculoatrial shunts, or by the means of neuroendoscopy (ETV).1
The most common shunt coplications include: infection, obstruction and overdrainage Prognosis of patients with aqueductal stenosis does not depend only on promptness and efficacy of surgical treatment. Better outcome is observed in post-natal than congenital hydrocephalus.1
This study evaluates hydrocephalus due to late onset congenital aqueductal stenosis regarding preoperative patients' characteristics (demographic data and clinical presentations), operative management, and postoperative patients' characteristics (complications and outcome).
This study included 25 patients with late onset congenital Sylvius aqueductal stenosis admitted to the neurosurgery department in Assiut University Hospital from march 2012 till march 2013. In this study, the patients were subjected to the following inclusion and exclusion criteria
A-Inclusion criteria:
B-Exclusion criteria:
All patients included in this study were subjected to the following:
Our study included 25 patients with late onset congenital aqueductal stenosis hydrocephalus.
In Table 1, patients were divided into 3 age groups. The highest incidence of late onset aqueductal stenosis was in the age group between (41-60) (44%) followed by the age group between (5-20) (36%), while the age group which showed least figures was the age group between (21-40) (20%).
Age group |
Male No.(%) |
Female No.(%) |
P value |
Age group 5-20 years |
5 (55.6%) |
4 (44.4%) |
0.15 |
Age group 25-40 years |
4 (80%) |
1 (20%) |
|
Age group 40-64 years |
9 (81.8%) |
2 (18.2%) |
|
Total |
18 (72%) |
7 (28%) |
Table 1 Relation between sex and age groups
Table 1, also showed sex predilection, where the highest incidence was in males in general (72%) while the females were just (28%). Females showed a significant peak in the age group between 5-20 years (44.4%) whereas the males were dominant in all the age groups especially the age group between 41-60 years (81.8 %) (Figure 1).
Table 2, shows the demographic distribution as 64% of the patient were from Assiut city itself, whereas only 36% of the patient were from other cities, also shows that majority of cases were married (64%) while only (36%) were singles. Regarding occupation, there was a significant percent of the patient who don't work (72%) while only (28%) were working (p=0.03) (Figure 2).
Demographic data |
No.(%) |
Residence |
|
Assiut |
16 ( 64 %) |
Outside Assiut |
9 (36%) |
Marital status |
|
Single |
9 (36%) |
Married |
16 (64%) |
Occupation |
|
Working |
7 (28%) |
Not working |
18 (72%) |
Table 2 Numbers and percent of cases in relation to demographic data
Table 3 shows significant longer duration of illness among the age group (21-40) in comparison to the duration of the other age groups.
Duration (months) Mean±SD |
Range |
|
Total group (years) 5-60 |
50.2±62.8 |
1-270 |
Age group 5-20 |
56±88.2 |
7-270 |
Age group 21-40 |
60.8±86.8 |
2-210 |
Age group 41-60 |
50.8±6.9 |
3-120 |
P value |
0.04 |
Table 3 Clinical and biochemical variables of individuals with overweight-obesity
SD: Standard Deviation; BMI: Body Mass Index; WC: Waist Circumference; AC: Abdominal Circumference; HC: Hip Circumference; RER: Respiratory Exchange Ratio; HR: Hear Rate.
Table 4 showed that the headache as a presenting manifestation has the highest incidence (76%) followed by visual manifestation (44%) whereas the urinary incontinence showed the least incidence (4%) (Figure 3).
Total No. (%) |
Male |
Female |
|
Headache |
19(76%) |
12(63.2%) |
7(36.8%) |
Visual manifestation |
11(44%) |
6(54.6%) |
5(45.5%) |
Disturbed Conscious level |
4(16%) |
4(100%) |
0(0%) |
Gait disturbance |
8(32%) |
6(75%) |
2(25%) |
Urinary Incontinence |
1(4%) |
1(100%) |
0(0%) |
Fits |
2(8%) |
2(100%) |
0(0%) |
Vomiting |
3(12%) |
1(33.3%) |
2(66.7) |
Table 4 Clinical manifestation of the studied patients. N.B: Most of the patients had more than one clinical presentation
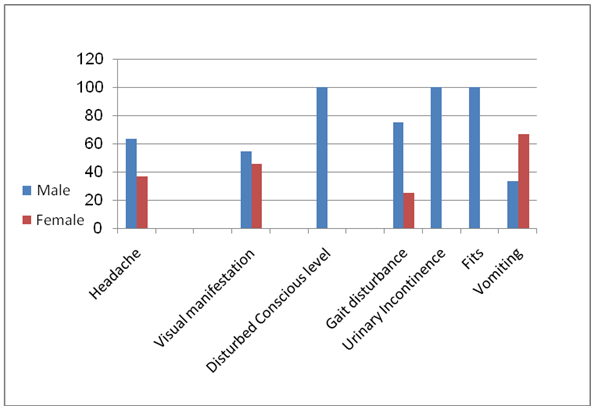
Figure 3 Clinical manifestation of the studied patients. N.B: Most of the patients had more than one clinical presentation.
Table 5 showed that there is relationship between affection of fundus and late onset congenital aqueductal stenosis (Figure 4).
Total No. of cases |
No. of cases with Normal fundus |
No. of cases with Blurred disc margins |
No. of cases with Papillodema |
25 |
6 |
5 |
14 |
Table 5 Relation between late onset congenital aqueductal stenosis and fundus examination
Table 6 showed the marked improvement of the cases after application of the shunt in 80% whereas only 12% of the cases didn't improve, and just 8 % showed deterioration (Figure 5).
Total No. of the cases of late onset congenital aqueductal stenosis |
No. of Cases improved after V-P shunt and (%) |
No. of Cases didn't improved after V-P shunt and (%) |
No. of Cases deteriorated and (%) |
25 |
20(80%) |
3(12%) |
2(8%) |
Table 6 Outcome of the patients after V-P shunt insertion
Table 7 showed that only 36 % of the cases showed postoperative complications.
No. of cases passed without any complications after shunt insertion and their percent (%) |
No. of cases developed complication after shunt insertion and their percent (%) |
Total No. of cases treated with V-P shunt |
||
Shunt obstuction |
Shunt Infection |
Subdural hamaetoma |
||
16(64%) |
1(4%) |
2(8%) |
6(24%) |
25 |
Table 7 Schedule showing the incidence of the complications after shunt operation
Case 1
A fifty eight years old male patient presented with urinary incontinence, ataxia, and headache of 4 month duration. Fundus examination showed blurred disc margins. The CT scan showed dilatation of lateral and 3rd ventricles. A ventriculoperitoneal shunt was inserted, but the patient didn't improve and moreover became comatosed. The CT scan was done and showed bilateral chronic subdural haematomas which were surgically evacuated via 4 burr holes with upgrading of shunt device and the patient afterward improved (Figure 6 & 7).
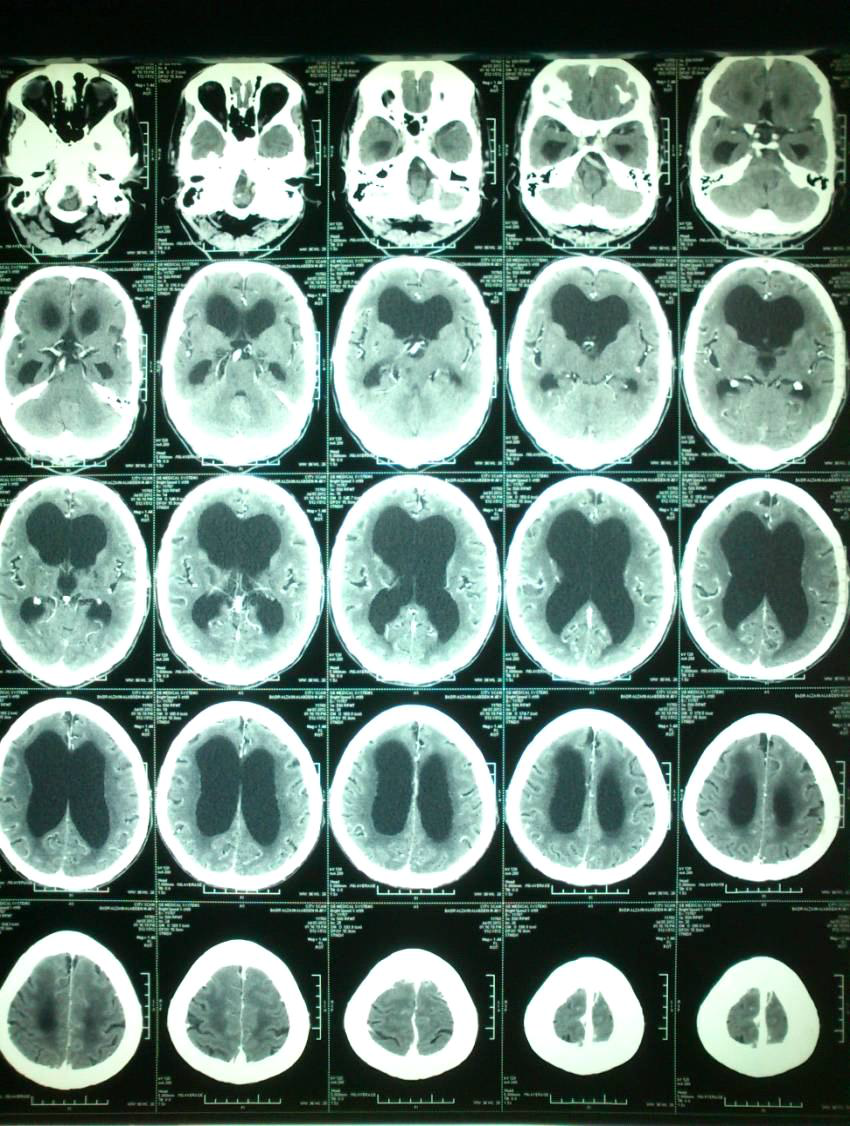
Figure 6 Preoperative CT showing late onset congenital aqueductal stenosis where there are dilatation of the lateral and 3rd ventricles while the 4th ventricle is normal.
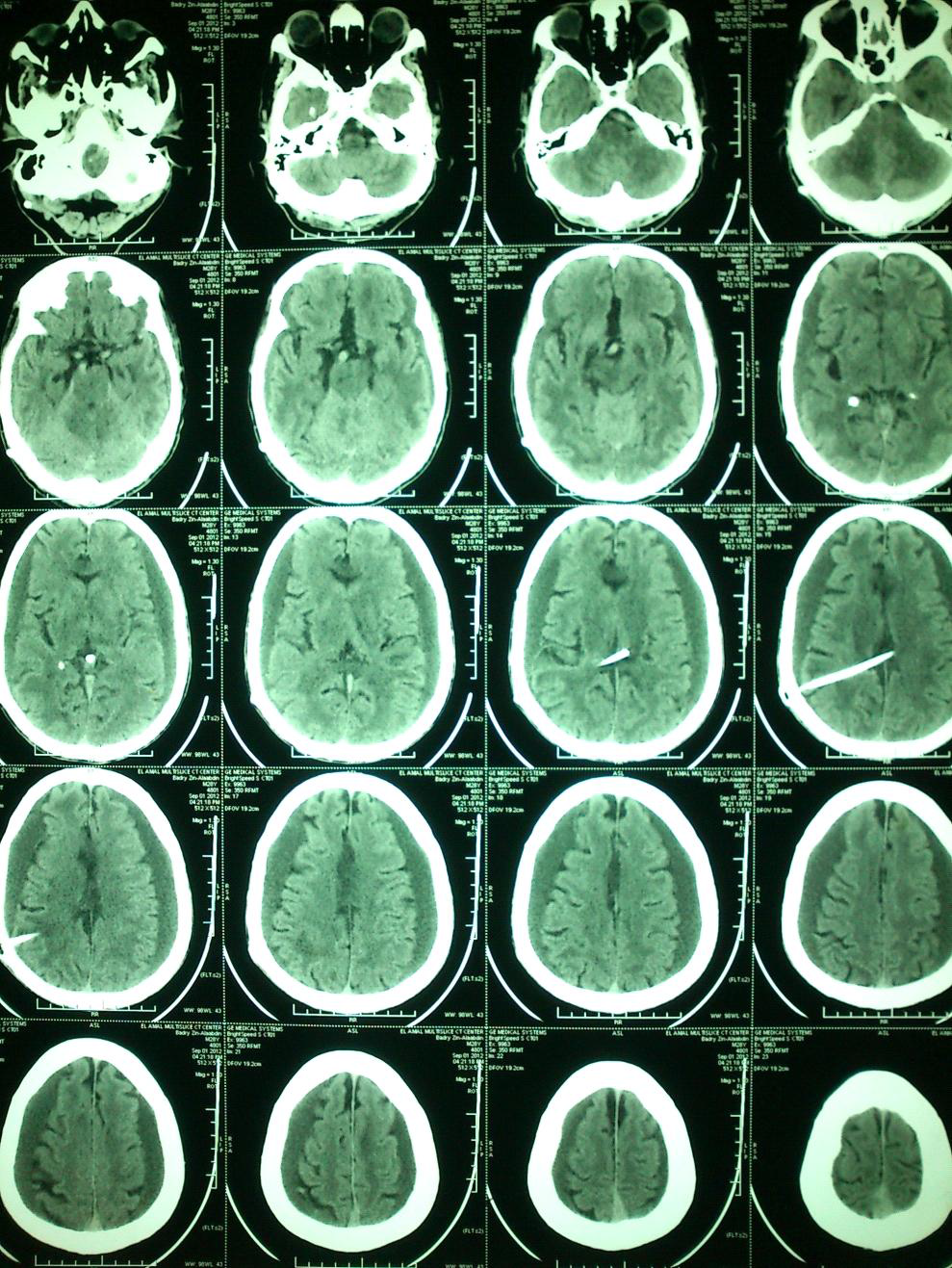
Figure 7 Postoperative CT showing development of bilateral subdural haematoma after shunt insertion as a result of overdriange Case No. 1.
Case 2
Female patient, 16 years old presented with headache and decreased intellectual performance. MRI revealed dilated 3rd and lateral ventricles. Ventriculoperitoneal shunt was done with no postoperative improvement. The patient presented one month later by the disturbed level of consciousness, left sided hemiparesis and urine incontinence. CT brain showed development of bilateral subdural hematoma and patient improved after evacuation of the hematoma and shunt upgrading (Figure 8-10).
Aqueductal obstruction constitutes 3% of adult hydrocephalus.2 Aqueductal Stenosis is usually a malformation occurring as a sporadic developmental anomaly. There are 4 main types of aqueductal obstruction.
Despite its' congenital origin, the alterations of the CSF dynamics can remain compensated and undiagnosed for several years.2 Clinical features in the compensated stage include episodes of headache and nausea, that are more severe in the morning because CSF is drained less in the recumbent position and is relieved by sitting up. There may be an even development of cognitive function with changes in behavior.
The patient may also present with an endocrine disorder due to the distraction of the hypothalamus and pituitary stalk by a grossly dilated third ventricle. The patient may also present with failure of upward gaze and accommodation due to pressure on the tectal plate.
In the late acute decompensated stage, the patient may present with vomiting, drowsiness and episodes of graying out of vision due to increased intracranial pressure. The patient may also have a spastic weakness of lower limbs with gait disturbance due to stretching of pyramidal tract around dilated third ventricle.
On physical examination, head circumference may be normal or only slightly increased. Imaging with CT and MRI will show dilated 3rd and lateral ventricles with a marked upward bowing of corpus callosum. The normal aqueductal CSF flow void in MRI cine phase contrast won't be seen, indicating obstruction to CSF flow through the aqueduct.5
Intersitial edema around the dilated ventricles will not be seen in the compensated stage of obstruction. MRI offers better morphological definition of the ventricles and shows some causal lesion like web.
MRI with cine phase CSF velocity study has improved diagnosis of this type of hydrocephalus by illustrating the aqueductal stenosis.5
The treatment option in the compensated stage is with drugs like acetazolamide and frusemide to limit the evolution of hydrocephalus by decreasing fluid secretion by choroid plexus.6,7
In late decompensated stage, the treatment option is surgical. In cases of shunt procedures CSF flow velocity imaging by MRI can show the patency of the shunt.
The present study included 25 patients with late onset congenital sylvius aqueductal stenosis admitted and managed at the neurosurgery department in Assiut university hospital from March 2010 till march 2011. In these patients, the cause of the hydrocephalus was the late onset aqueductal stenosis.
In the present study, we divided the age group into 3 subgroups and found that the highest incidence of late aqueductal stenosis was in the age group between 41-64years (44%) followed by the group between 5-20 years (36%), while the age group which showed least figures was the age group between 21-40 years (20%).
When we compared the sex predilection in this study, we found that the higher incidence occurs in males in general (72%) while the females were just (28%). The females showed a significant rise in the age group between 5-20 years with a percent of (44.4%) whereas the males were dominant in all the age groups, especially the age group between 41-64 years with a percent of (81.8%).
The demographic distribution showed that there was a significant percent of the patients who don't work (72%) while only (28%) were working (p=0.03). In the present study, headache as a presenting manifestation has the highest incidence (76%) followed by visual manifestation (44%), whereas the urinary incontinence showed the least incidence (4%).
Other studies showed that headache occurs in approximately 50% of adult patients.8 It has been suggested to be caused by raised intracranial pressure because of impaired flow within the ventricular system and may be associated with other unspecific signs of elevated intracranial pressure, such as transient visual scotomas, diplopia, tinnitus and papilloedema.9
The present study showed the marked improvement of the cases after application of the shunt 80%, whereas only 12% of the cases didn't improve, and just 8% showed deterioration. The present study showed that only 36% of the cases showed postoperative complications (4% of the cases showed shunt obstruction and 8% showed shunt infection, and 24% showed post shunting subdural haematoma).
Other study10 showed that mechanical obstruction had occurred in 14% of cases.This may occur at either or both ends, but usually due to obstruction of ventricular catheter by entrapped choroid plexus tissue, intraventricular debris or gliosis around the catheter tip. This incidence is highest in early postoperative period and decreases with time. We had proximal obstruction in six of the seven cases. Distal obstruction is due to accumulation of debris in the slit valve. The dead space beneath the slit valve favors this accumulation. Debris is composed of acellular fibrin clumps surrounded by a large number of macrophages, lymphocytes and fibroblasts. We had one patient with peritoneal end blockage by tissue debris.
The second most common complication of these procedures is infection. This occurs in 5 to 10% of the cases and is usually the result of prior infection of CSF or infection introduced during surgery. Ventriculitis, meningitis and local wound infection are the most common clinical manifestations. The infection rate in that study is 12%. Infection is generally due to organisms of low virulence, most commonly Staphylococcus epidermidis.11 Staphylococcus aureus, Gram negative bacilli and mixed pathogens are the next most common agents encountered. The organism cultured in our series was predominantly the Staphylococcus species.
The most common complication was post shunting subdural haematoma. This occurred in 6 patients (24%). This possibly happened due to rapid drainage of the CSF with ventricular collapse, so we recommend intraoperative measuring of intraventricular pressure to select proper shunt pressure, otherwise we recommend to insert a high pressure valve.
Our study included 25 patients with late onset congenital aqueductal stenosis. The highest incidence of late onset aqueductal stenosis was in the age group range between 41-60 years (44%) followed by the age group between 5-20 (36%). Late onset hydrocephalus were more frequent among males (72%) than females (28%). Headache as a presenting manifestation has the highest incidence (76%) followed by the visual manifestation (44%) whereas the urinary incontinence showed the least incidence (4%).
Marked improvement of the cases after application of the shunt 80%, whereas only 12% of the cases didn't improve, and just 8% showed deterioration. Complication of the operation were recorded in 36% of the cases (4% of the cases showed shunt obstruction, 8% showed shunt infection, and 24% showed post shunting subdural haematoma). The most common complication was post shunting subdural haematoma. This possibly happened due to rapid drainage of the CSF with ventricular collapse. Infection was the second most common complication of these procedures it may be related to prior infection of CSF or infection introduced during surgery. Ventriculitis, meningitis and local wound infection are the most common clinical manifestations.
Late onset aqueductal stenosis, congenital hydrocephalus is not uncommon cause of the hydrocephalus in our locality. Detection and management of such patients with the well manifest clinical data confirmed with the neuroimaging studies became easy. We recommend detailed multicentric studies to overcome our restricted number of cases which were studied in short time (one year).
None.
None.

©2016 Mohammed, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.