Journal of
eISSN: 2373-633X


Case Report Volume 14 Issue 5
1Assistant Surgeon of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
2Surgical Resident of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
3Associate Professor of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
4Professor, Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
Correspondence: Ulises Parada, Assistant Surgeon of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Montevideo, Uruguay, Tel 099313877
Received: September 12, 2023 | Published: October 5, 2023
Citation: Parada U, Fernández L, Ramirez L, et al. Zenker’s diverticulum: clinical case and surgical technique. J Cancer Prev Curr Res. 2023;14(5):103-107. DOI: 10.15406/jcpcr.2023.14.00530
Zenker's diverticulum is a protrusion of the esophageal pharyngeal mucosa and submucosa through a weak area of the posterior pharyngeal wall called Killiam's triangle. It is located between the inferior constrictor muscle and the cricopharyngeus muscle. It is considered a false diverticulum since its walls lack a muscular layer. The treatment accepts two different access routes: transoral endoscopic access in which there are publications in our environment and open surgery consisting of myotomy of the upper esophageal sphincter and diverticulectomy or diverticulopexy. The importance of this clinical case is to show that despite the advent of other less invasive techniques, surgery continues to maintain its place in the therapeutic arsenal for Zenker's diverticulum, providing safety and relief of symptoms. The aim of this article is to describe the surgical technique for the treatment of Zenker's diverticulum based on a clinical case. Performing surgery following the technical details described in the clinical case would reduce the most frequent complications such as recurrent laryngeal nerve injury, bleeding, anastomotic leakage and esophageal stricture. Although surgery is more invasive and requires a longer hospital stay, it remains a valid and safe technique for the management of Zenker diverticulum.
Keywords: Zenker's diverticulum, surgical technique, endoscopy
Zenker's diverticulum (ZD) is a protrusion of the pharyngoesophageal mucosa and submucosa through a weak area of the posterior pharyngeal wall called Killiam's triangle.1 This is located between the inferior constrictor muscle and the cricopharyngeus muscle. It is considered a false diverticulum since its walls lack a muscular layer (Figure 1).2
It was described for the first time in 1767 by Ludlow3 during an autopsy, but owes its name to Friedrich Albert von Zenker, who a little more than a century later described it in greater detail, adding his own series.4 Among the most frequent symptoms are dysphagia, halitosis, noisy swallowing and regurgitations.5 The most accepted hypothesis is the asynchrony between the contraction of the walls and the relaxation of the upper esophageal sphincter being by definition a diverticulum by pulsation and acquired.6,7 This hypothesis is supported by a loss of elasticity of the upper esophageal sphincter in which the muscle is replaced by fibroadipose tissue and which are more frequent in elderly patients where there could be some degree of deterioration of neuromuscular coordination.8
It is the most common esophageal diverticulum, although the frequency is low between 0.01 and 0.11 % of the population. Most of them occur in men and over 60 years of age, however it is difficult to determine the real incidence, because a number of patients are not diagnosed.9
The diagnosis is made by performing a barium transit that allows to see the diverticulum, its size and topography. It is important to evaluate the three swallowing times 1) oropharyngeal 2) pharyngeal esophageal 3) esophageal. The barium clearance, elimination times, and the cricopharyngeal cleavage approximately in the 6th cervical vertebra, which is necessary to know for the interpretation of clinical pictures, will be observed (Figure 2). Upper endoscopy is not strictly necessary for the diagnosis, however it could be complementary, assessing the presence of structural changes in the mucosa as well as differential diagnoses.10 Esophageal manometry and video fluoroscopy provide data regarding pathogenesis.11

Figure 2 Barium transit. Gastric esophagus barium study. Zenker's diverticulum is observed in the posterior pharyngeal esophageal face marked with black arrow.
The treatment of DZ accepts two different access routes: transoral endoscopic access in which there are publications in our environment12 and open surgery consisting of myotomy of the upper esophageal sphincter and diverticulectomy or diverticulopexy. The aim of the article is to describe the surgical technique of DZ treatment based on a clinical case.
Male patient, 74 years old, hypertensive with no other history. He consults for dysphagia for solids, halitosis, regurgitation and noisy swallowing of approximately 3 to 4 years of evolution. He is evaluated with high endoscopy and barium transit.
The endoscopy highlights immediately above the upper esophageal sphincter, a drop in a blind pouch, which appears to be a wide cervical esophageal diverticulum. Mucosa without alterations. Given the endoscopic findings, it was decided to request an esophageal transit. From the pharyngeal esophageal transit, a 53mm posterior diverticulum compatible with Zenker's diverticulum is highlighted. It fills quickly and is very slow to evacuate. The rest of the esophageal and pharyngeal esophageal passage of usual caliber without evidence of other alterations. It was discussed in the athenaeum and surgery was decided because it was a diverticulum larger than 50 mm. Diverticulectomy and myotomy of the cricopharyngeal muscle. During hospitalization, the patient reported controlled pain, without dysphagia, barium esophageal transit was performed without leakage or esophageal narrowing. Patient was discharged after 7 days tolerating oral route with wounds in good condition and without dysphagia. In postoperative controls 2-3 months after surgery, patient is tolerating oral route (liquid and solids) without difficulties, denies dysphagia, halitosis and regurgitation. Pathological anatomy of the diverticulum microscopy: esophageal mucosa with erosion, acanthosis, spongiosis and intraepithelial lymphocytic and polymorphonuclear infiltrate. Submucosa: edematous with congestive vessels and diffuse lymphoplasmacytic infiltrate. No evidence of malignancy.
The treatment of DZ is currently not standardized. Basically, there are two types of approach: surgical and endoscopic, each with its advantages and disadvantages. Endoscopic treatment offers the advantages of minimally invasive procedures, less pain, avoidance of skin incision and dissection of deep cervical planes, shorter procedure time and shorter hospital stay. These factors added to the fact that most of the patients with DZ are older than 60 years old9 some with underlying pathologies make this type of technique gaining followers.
Different technical particularities are described in the literature that are beyond the scope of this article, but beyond this, a therapeutic efficacy of around 91% is achieved for symptom relief, concluding that it is an effective and safe technique.13,14 The most feared complications are perforation, bleeding and persistence of symptoms, in which case the procedure may even be repeated.12 One of the aspects to take into account when choosing therapeutic options is diverticular size. Diverticulum size greater than 50 mm has been linked as a risk factor for endoscopic therapeutic failure.15 It is in these patients with large diverticula where the surgical option acquires greater value. Especially young patients and without associated comorbidities. We must also take into account that the endoscopic procedure is not always available in all centers and with incoming personnel.
Surgical treatment consists of cricopharyngeal myotomy and diverticulectomy or diverticulopexy. Surgical results have been satisfactory with a remission of symptoms of more than 90% and a recurrence rate of 5%. Post-operative morbidity is not negligible, with recurrent laryngeal nerve palsy (3.2%), salivary fistula (1.8%) and wound infection (3%).16,17 Ultimately, the choice of one procedure or another must be individualized, taking into account the size of the diverticulum, the patient's comorbidities, the experience of the team involved, as well as the possibility of human and material resources. In cases where surgical treatment is chosen, it is essential to take into account technical details in order to achieve a systematized, quality and safe procedure. The following is a description of the surgical procedure used in the clinical case presented.
Regarding the surgical technique used, the following is described:
Diverticulectomy and cricopharyngeal myotomy. This is not intended to be a "new surgical technique" but to detail the most relevant aspects of the procedure considered by the author group to alleviate symptomatology and reduce the incidence of complications.
Materials to be used
Patient preparation
Once the patient undergoes oro-tracheal intubation, the tube is fixed with an elastic net to avoid extubation during surgery. A siliconized support is placed at cephalic level to fix the head and neck in the form of a screw that allows a correct support, position and prevents movements during the course of surgery (Figure 3). The patient is placed in dorsal decubitus position with neck extension and is lateralized to the right exposing the left lateral region (Figure 4).

Figure 3 Silicone skull support. It keeps the position of the head and neck fixed, it is of great importance to avoid movements that may cause cervical spine injuries and extubation. Black arrow marks the device.
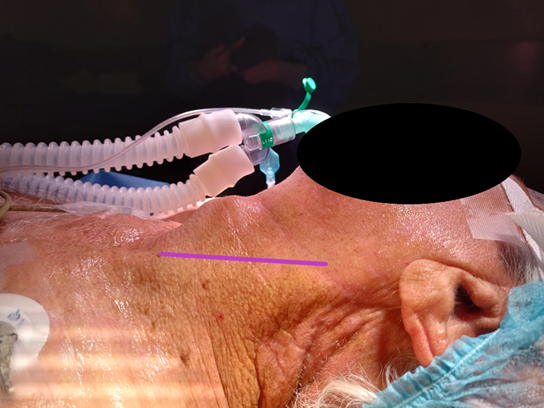
Figure 4 Exposure of the lateral neck region. The purple line marks the site of the pre sternocleidomastoid incision. Note the extension of the neck and its rotation to the right side exposing the left lateral cervical region.
The surgical drapes are placed in a triangular shape at the level of the base of the neck and in a flat shape covering the head leaving the whole neck region exposed. The authors do not wrap the head with capellin-shaped drapes since they do not visualize benefits and also hinder the esophageal calibration maneuver described in the surgical technique.
The surgery is started by making a pre sternocleidomastoid incision (ECM) on the left side because there is a slight displacement of the esophageal pharyngeal sector towards this side with respect to the airway. It extends from the hyoid bone up to a couple of cm before reaching the sternal recess (Figure 4). For the separation of the covering planes we use 2 Adson's auto-static separators (Figure 5). This allows in addition to a correct exposure to leave the hands of the assistants free for drying, traction and separation.
Once the skin and platysma are sectioned, we proceed to the identification of the anterior border of the sternocleidomastoid muscle, at this level, we proceed to the superficial cervical aponeurosis. This plane allows a bloodless surgery, without the need of dissection of the vascular-nerve bundle of the neck, leaving it laterally to the dissection plane.
In the middle cervical aponeurosis is the omohiodeus muscle, the author group reclines it without sectioning it (Figure 5). The opening of the aponeurosis allows us by means of blunt dissection and through an alveolar plane to palpate the cervical spine, the esophagus is identified immediately above it.
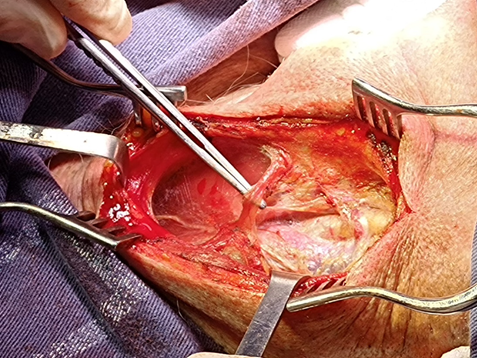
Figure 5 Left pre-sternocleidomastoid incision. Autostatic and loaded separator of the omohyodeus muscle is visualized on a dissecting forceps. Note the width of the incision and the exposure obtained from the sternocleidomastoid region.
Once the esophagus has been identified, in order to achieve a correct exposure of the esophagus, we separate it into 2 complexes: one medial, the thyroid and the trachea, and the other lateral, formed by the ECM and the vascular-nervous bundle of the neck. This maneuver allows access to the retropharyngeal esophageal sector and visualization of the diverticulum. Most of the time, ligation of the thyroid pedicle is not necessary. Traction maneuvers should be gentle to avoid bleeding of the gland and its pedicles as well as injury to the recurrent laryngeal nerve. If a correct and comfortable exposure is not achieved, the inferior thyroid pedicle can be ligated without major consequences.
Once the diverticular pouch is identified, it is dissected and released by means of a blunt and gentle maneuver until the neck of the pouch is identified on the posterior pharyngeal esophageal surface. Technically, traction with Allis or dissecting forceps is useful (Figure 6).

Figure 6 Identification and dissection of the diverticular sac. The figure shows the diverticulum tracted from the dissecting forceps. The esophagus is accessed through an alveolar plane medial to the vasculonervous bundle. The cervical spine is used to identify the esophagus which is immediately in front of it. The diverticulum must be dissected with blunt maneuvers up to the esophagus (diverticular neck).
Upon reaching the neck, we can clearly identify the cricopharyngeal muscle in the lower sector, which is loaded with American forceps, taking care not to injure the mucosa and submucosa and sectioning it with ligasure or electric scalpel (Figure 7).

Figure 7 Loading of the cricopharyngeal muscle with American forceps. Once the diverticulum is completely dissected, the cricopharyngeal muscle is loaded, taking care not to injure the mucosa or sub mucosa. It is sectioned with vascular sealants.
To calibrate the esophageal lumen we use a 32 Fr chest tube. It is convenient that the placement of the probe is performed by a surgeon in continuous dialogue and coordination of the maneuver with the team that is participating in the surgery. The passage is checked visually and palpatorily a couple of centimeters distal to the neck of the diverticulum.
This passage of the 32 Fr tube allows to calibrate the esophagus avoiding the narrowing of the lumen, assuring a good passage of the alimentary bolus. Once calibrated, we are able to perform the diverticular section. The authors prefer the use of mechanical suture with triple row of hooks, violet or gold charge. The non-opening of the mucosa avoids contact of the esophageal lumen with the surrounding tissue, thus avoiding contamination (Figure 8 and 9).

Figure 8 Dissection of diverticulum up to the neck after esophageal calibration. Section with gold-loaded mechanical suture. Calibration of the esophageal lumen with a thick probe is a very important point of the surgery since it avoids narrowing the lumen and therefore postoperative dysphagia.

Figure 9 Diverticulum resection. This type of gold or violet load is preferred since it presents triple row of agrafes giving greater security to the procedure. The resection specimen is sent for definitive anatomopathological study.
Reinforcement stitches are made covering suture with absorbable monofilament thread polydioxanone 4-0 using the inferior fibers of the inferior constrictor of the pharynx (Figure 10). At this moment we remove the chest tube and we place a nasogastric tube also under mink up to the gastric chamber which is used as a feeding route in the postoperative period. We leave a glove sheet or suction drainage at cervical level, which is removed after the 3rd day. We perform a barium transit prior to the reestablishment of the oral route in order to evaluate the passage and rule out leakage.
With the advent of other less invasive therapeutic options such as endoscopy and due to the low frequency of this pathology, training in the surgical technique has decreased. Although surgery is more invasive and requires a longer hospital stay, it continues to be a valid and safe technique for the management of Zenker diverticulum. Performing surgery following the technical details described in the clinical case would reduce the most frequent complications such as recurrent laryngeal nerve injury, bleeding, anastomotic leakage and esophageal stricture.
None.
Authors declare that there is no conflict of interest.

©2023 Parada, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.