Journal of
eISSN: 2373-633X


Case Report Volume 13 Issue 6
Centro de Radioterapia Deán Funes, Argentina
Correspondence: Ariel Matías Gómez Palacios, Centro de Radioterapia Deán Funes, Córdoba, Argentina
Received: December 17, 2022 | Published: December 30, 2022
Citation: Palacios AMG, Gilardi J, Raies A, et al. Vaginal neuroendocrine carcinoma: regarding a clinical case. J Cancer Prev Curr Res. 2022;13(6):158-159. DOI: 10.15406/jcpcr.2022.13.00507
Primary small-cell neuroendocrine carcinoma of the vagina is a rare tumor with aggressive clinical behavior and poor prognosis despite the current multimodal therapeutic options.1 The mean age at diagnosis is 59 years, and women typically present with postmenopausal bleeding. Characteristically, this malignancy results in lymphovascular space invasion, and the clinical course is marked by early hematogenous widespread dissemination and early demise.2 Less than 30 cases have been reported in the literature3,4 and its most common location in the vagina is the upper third and posterior face of it.5
This is a 77-year-old female patient, with no personal pathological history, diagnosed with FIGO Stage I vaginal carcinoma who came to our clinic at the Centro de Radioterapia Dean Funes to assess radiant treatment. She presented with fetid serohematic genital discharge of several months of evolution, which is why she consults the gynecology service.
Among the relevant gynecologic and obstetric history are: eight pregnancies (6 natural births, 1 caesarean section and 1 spontaneous abortion) and one sexual partner. She denies any previous sexually transmitted disease. She did not perform annual gynecological screening.
On gynecological physical examination: an exophytic, friable and bleeding lesion of 3 cm is observed and palpated, which compromises the posterior face of the vagina, in its middle-upper third; respecting the rest of the organ and the cervix. On rectal examination, the ampulla is empty, without lesions; the parametria are free.
A transvaginal pelvic ultrasound was performed in which no ovarian or uterine lesions were found. And an excisional biopsy was performed.
The anatomopathological study showed: small cell neuroendocrine carcinoma. Immunohistochemistry: CK7 positive, synaptophysin positive, focal positive chromogranin, p40 negative, p16 positive and Ki67 90%.
A.Histopathology where several fragments are observed, some of which show the presence of a stratified squamous epithelium that shows ulceration, with the presence of a neoplasm made up of small cells with intense, basophilic chromatin, and in the lamina propria. Scarce cytoplasm that is arranged in sheets or trabeculae, identifying an eosinophilic material between the nests, acellular. Immunomarking was performed, which was positive for CK7, Synaptophysin and focally for Chromogranin, confirming the neuroendocrine lineage. p16 was positive, p40 was negative. Ki67 proliferation factor is 95%.
A chest-abdominal-pelvic CT was indicated, in which hypervascular blastomatous thickening of the vaginal walls was evidenced as pathological. A pelvic MRI was performed, showing a vegetating lesion in the vaginal lumen, with a sessile appearance, between 8 and 12 hours, solid, generally homogeneous, with greater peripheral contrast enhancement, showing diffusion restriction, 28mm by 21mm by 25mm, suspicious in appearance, of apparent vaginal origin, found in its middle third, without contact with the cervical area. It does not extend beyond the walls of the organ, finding the surrounding perivaginal fatty tissues respected, like the rest of the perineal organs (Figure 1). Uterus and bladder without suspicious lesions. In the right ovary, a complete cyst was observed without signs of malignancy. No pelvic lymph nodes were found.
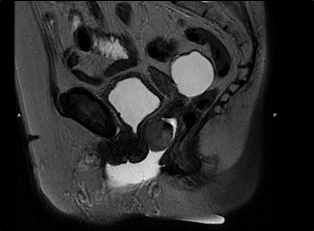
Figure 1 MRI (Sagittal T2 Image) shows a solid, vegetating, blastomatous formation, originating from the right anterolateral margin of the vaginal middle third, measuring 50 mm by 42 mm by 19 mm, with a blastomatous appearance.
It was staged as FIGO stage I vaginal carcinoma. It was evaluated by an interdisciplinary committee (pathologists, gynecologists, clinical oncologists, and radiation oncologists) and was defined as concomitant treatment with chemotherapy based on cisplatin/etoposide and external radiotherapy to the pelvic area (50 Gy in 25 fractions). Subsequently, under local anesthesia Vaginal HDR 3D brachytherapy was performed (Total dose of 18 Gy in 3 fractions of 6 Gy, 25 mm cylinders) (Figure 2).
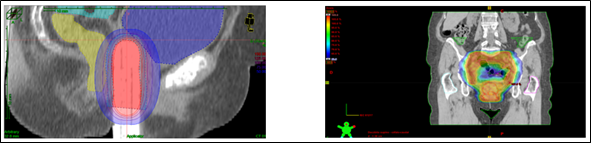
Figure 2 On the left, the vaginal applicator is shown with the HDR brachytherapy dose distribution. On the right, dose distribution for external radiotherapy (treated with VMAT).
Patient finished radiant treatment with G2 vulvar radiodermatitis and G1 urethritis. They resolve with topical treatment and oral analgesics (paracetamol).
The most common location of neuroendocrine carcinoma in the vagina is the upper third and posterior face of the vagina,5 as occurred with our patient. The definitive diagnosis of small cell neuroendocrine carcinoma is made by anatomopathological and immunohistochemical study.
Complete clinical evaluation is essential to establish the origin of the tumor and rule out metastasis, with the lung being the most frequent site of primary small cell carcinoma. It is also important to note that the FIGO staging of vaginal carcinoma should be clinical and not surgical.6 In our clinical case, the patient underwent an exhaustive physical examination and was studied with different complementary methods (CT thoraco-abdomino-pelvic, pelvic MRI, gynecological ultrasound) to exclude direct extension and primary carcinoma in other tissues, since the Small cell carcinoma of the vagina is histologically similar to small cell carcinoma of the lungs, which is why it was classified as stage I primary vaginal carcinoma.
No consensus has been reached on the optimal treatment, since this pathology is very rare and current therapies have given poor results. Surgical resection or radiotherapy or both may provide increased local control, and chemotherapy is frequently employed as part of the therapeutic regimen.6 Despite a multimodal approach and using multidisciplinary guidance, prognosis is poor since distant metastasis is the likely outcome.
Eighty-five percent of patients die within one year of diagnosis,7,8 and survival after diagnosis of recurrent disease is short, typically only 7 months.9 Our patient’s course was consistent with the literature when she developed recurrence 7 months after her initial visit. Typically, PFS in recurrent gynecologic small-cell neuroendocrine carcinoma of the cervix in treated patients is 7-8 months.10 She died one year after the initial visit.
None.
The authors declare that they have no conflicts of interest.

©2022 Palacios, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.