Journal of
eISSN: 2373-633X


Case Report Volume 14 Issue 4
1Department of, Surgery, Om Surgical Center & Maternity Home, India
2Department of Obstetrics and Gynecology, Om Surgical Center & Maternity Home, India
Correspondence: Dr. Pankaj Srivastava, Laparoscopic, Thoracic, Thoracoscopic & VATS Surgeon, Om Surgical Center & Maternity Home, SA 17/3, P-4, Sri Krishna Nagar, Paharia, Ghazipur Road, Varanasi, UP, India, 221007, Tel +91-542-2586191
Received: August 08, 2023 | Published: August 22, 2023
Citation: Pankaj S, Shalini S. Trichilemmal cyst: a simple cyst having the potential of complications-revisited. J Cancer Prev Curr Res. 2023;14(4):83-85. DOI: 10.15406/jcpcr.2023.14.00526
We Present the case of a trichilemmal cyst of the scalp which is a common intradermal cyst having the minimal potential of the malignant transformation. Treatment of this cyst should be considered always by keeping in mind its transformation into an aggressive proliferating trichilemmal cyst and rarely into a malignancy. The purpose of the presentation is a review of the latest literature and awareness about the common ailment having malignant potential.
Keywords: trichilemmal cyst, pilar cyst, cyst, scalp, benign, proliferating cyst, intradermal, hair, follicle, excision
Trichilemmal cysts are common intradermal cysts derived from the hair follicle. This is also known as a pilar cyst. The trichilemmal cyst is originated from the outer hair root sheath and is filled with keratin. It is the second most common type of cutaneous cyst present mostly in the scalp region (~90%) and also in the scrotum and fingers.1 This is a type of simple cyst lined by the stratified squamous epithelium, filled with dense keratin which is eosinophilic in nature. The granular cell layer is absent in the epithelial lining. It may develop into Proliferating trichilemmal cyst, Merkel cell carcinoma, and other malignancies.
A 47-year-old non-smoker, non-alcoholic, non-vegetarian male presented with slowly growing painless swelling on the scalp over the frontoparietal junction of the skull for the last 8 years (Figure 1). The swelling was initially of peanut size but gradually attended to the size of a walnut. The margins of the lump were well-defined with sharp edges. The skin over the swelling was normal and the tumor was firm and mobile under the skin and not fixed to the base too. There was no punctum found over the lump. There was no history of penetrating or blunt trauma and any previous operation. The patient had no complaints except cosmetic concerns for which he needed an excision. A provisional diagnosis of an epidermal cyst was made.
All the vitals and blood parameters were normal. The excision of the tumor was planned under local infiltration anesthesia. The patient was put in the supine position and after proper painting and draping, the skin around the tumor was infiltrated with 0.5% lignocaine containing 1:10 000 norepinephrine solution at 3, 6, 9, and 12 O’clock positions to make surrounding skin anesthetized. 1mL anesthetic solution was also infiltrated under the bed of the tumor. The tumor was then enucleated in toto with the help of blunt and sharp dissection. Hemostasis is done. The wound was closed with a 4-0 polypropylene suture and dressed. Stitches were removed on the 8th postoperative day. The patient had no complaints in the postoperative period (Figure 2). One year follow-up is uneventful with no recurrence and an almost invisible surgical scar (Figure 3).
A gross examination of the tumor revealed a well-circumscribed firm, ovoid, tan-white soft tissue which measured 1.5 x 1.5 cm (Figure 4), and the cut section showed an irregular soft inner surface with no content (Figure 5). Histologic examination revealed Cyst lined by squamous epithelium with an absent granular layer with homogenous very dense pink keratin (Figures 6 & 7). The final diagnosis was in favor of a Trichilemmal cyst (Table 1).
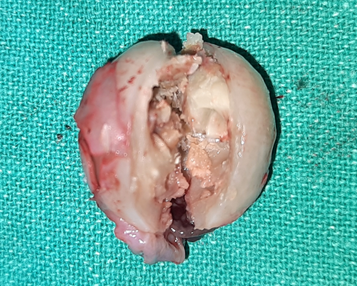
Figure 5 Cut-section of the trichilemmal cyst in toto after excision showing irregular soft inner surface with no content.

Figure 6 Microscopic examination revealed trichilemmal cyst lined by squamous epithelium with absent granular layer.

Figure 7 Microscopic examination revealed trichilemmal cyst lined by squamous epithelium with homogenous pink keratin (H&E Stain).
1. Dermoid cyst |
2. Epidermal inclusion cyst |
3. Lipomas |
4. Proliferating pilar tumor |
5. Malignant Proliferating pilar tumor |
6. Hibernomas |
7. Spindle cell liopmas |
8. Pilomatrixoma |
9. Steatocystoma multiplex |
10. Liposarcoma |
11. Acne keloidalis nuchae |
12. Neurofibromas |
13. Osteoma cutis |
Table 1 Differential diagnosis of fibroma of tendon sheath
Trichilemmal cysts or "Pilar" cysts are mostly involved in the scalp region and are derived from the external hair follicle root sheath. The hair follicle's external root sheath is repeated at the isthmus of the follicle in the cyst wall. These cysts are mostly asymptomatic, firm in touch, mobile, non-tender dermal, or subcutaneous nodule-like structures. Central punctum is absent. These are small in size until complicated. Genetically most cysts follow autosomal dominant inheritance but genetic inheritance is not yet clear. It is emphasized that Phospholipase C delta 1 (PLCD1) and monoallelic mutational mechanism are responsible for the cyst formation.2,3 Diagnosis is mainly clinical but on sonography, it is present as well-defined lesions which are hypoechoic in nature. The internal calcification with posterior enhancement in the soft tissues of the scalp or beneath the structure is suggestive of a Trichilemmal cyst.4 It is usually a benign tumor, but malignant transformation has been reported. Metastasis is rare with this even on malignant transformation. Proliferating trichilemmal cysts can develop from a benign trichilemmal cysts after trauma, irritation, or inflammation.5 Merkel cell carcinomas have been also reported in a complicated trichilemmal cyst.6 Intracystic squamous cell carcinoma (SCC), a very rare malignant transformation arising within a cutaneous cyst is also reported.7,8 Treatment included simple cyst excision with the cyst wall and its entire content in toto. Neoadjuvant radiotherapy is advised in medically unfit patients and where the tumor involves cosmetically important regions to shrink the tumor before definitive surgical resection in a subset of proliferating trichilemmal tumors.9 The local recurrence has been evaluated by the Ki67 immunostaining technique and is correlated with low recurrence potential.10
Trichilemmal cysts are the common intradermal cysts found in scalp region but should always be considered as a matter of concern because of its malignant potential to get converted into fatal malignant proliferating trichilemmal tumors and even squamous cell carcinoma. So in my opinion, excision of the cyst should always be considered as feasible.
None.
Authors declare that there is no conflict of interest.

©2023 Pankaj, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.