Journal of
eISSN: 2373-633X


Case Report Volume 14 Issue 5
1Assistant Surgeon of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
2Residente Cirugía General, Hospital de Clínicas Universidad de la República, Uruguay
3Anatomia Patologica, Hospital de Clínicas Universidad de la República, Uruguay
4Professor, Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
Correspondence: Ulises Parada, Assistant Surgeon of the Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Montevideo, Uruguay, Tel 099313877
Received: September 21, 2023 | Published: October 6, 2023
Citation: Parada U, Viana S, Ramírez L, et al. Tall cell papillary thyroid micro carcinoma: case report and review of the subject. J Cancer Prev Curr Res. 2023;14(5):109-111. DOI: 10.15406/jcpcr.2023.14.00531
The WHO defines papillary micro thyroid carcinoma as a papillary thyroid carcinoma with a maximum diameter not exceeding 10 mm. Discussion: There are anatomo-pathologic variants such as the tall cell variant with a more aggressive course and unfavorable prognosis, which will have repercussions on therapeutic decisions. Although lobectomy plus isthmectomy is accepted as a surgical treatment for micro carcinoma, is it sufficient when it presents with a tall cell subtype? We will present a clinical case of a patient with papillary micro carcinoma of tall cell variant. Conclusion: Tall cell variant papillary micro carcinoma presents structural, phenotypic and genotypic characteristics that imply a different management than its classic variant, even though it is a micro carcinoma.
Papillary micro thyroid carcinoma (MCP) is defined by the WHO as a papillary thyroid carcinoma with a maximum diameter of less than 10 mm.1 Despite having an indolent course in most cases, a small number of patients with MCP spread outside the thyroid gland to the lymph nodes and, more rarely, hematogenously. Therefore, it is important to determine which characteristics of MCP are more aggressive and what type of treatment is indicated for a particular case.
There are anatomo-pathological variants such as the tall cell variant with a more aggressive course and unfavorable prognosis, which will have an impact on therapeutic decisions.2 The tall cell variant is defined by the presence of at least 30% of tall cells in the cellular universe of the tumor. Characteristically they are at least 2 to 3 times taller than wide and have an eosinophilic cytoplasm, the nucleus is large, irregular in outline and oriented to the basement membrane.2,3 This histological subtype is considered by the ATA (American Thyroid Association) to have a higher risk of recurrence, metastasis and more importantly a lower response to iodine.4 The therapeutic options for MCP cover a wide spectrum of possibilities ranging from active surveillance (AS) to surgery (lobectomy, total thyroidectomy, nodal emptying). Although lobectomy plus isthmectomy is accepted as a surgical treatment for MCP, is it sufficient when presented with tall cell subtype? We will present a clinical case of a patient with papillary micro carcinoma of tall cell variant (MCP CA).
Female patient, 25 years old. No history of cervical irradiation, nor family history of thyroid cancer. Currently the patient is undergoing studies for gender reassignment. She refers unspecific discomfort in the neck for which cervical ultrasound is requested by the treating physician. With the result she was referred to the surgery polyclinic. The ultrasound showed a thyroid of normal size with a thyroid nodule (TN) of 6 mm in the left lobe. It does not establish more characteristics about the TN, without adenopathies. The patient is explained the indolent nature of most of these TN, however the patient insists on fine needle aspiration puncture (FNA). The acting team agrees to perform the puncture, cytology reports MCP without further specifications. Therapeutic possibilities were explained to the patient, VA was proposed, to which the patient refused and opted for surgery. Left lobectomy plus isthmectomy by Kocher incision was performed. The patient had a postoperative period without dysphonia and without hypocalcemia. The high cell MCP, a negative lymph node, an intrathyroid parathyroid is highlighted (Figure 1 - 3).
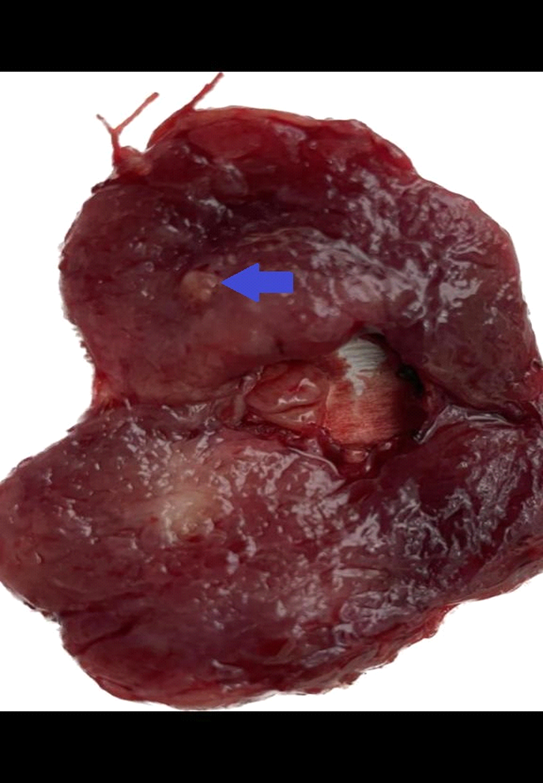
Figure 1 Resection and opening of the left thyroid lobe for identification of the thyroid micronodule. Arrow points to the micronodule 5-6 mm.
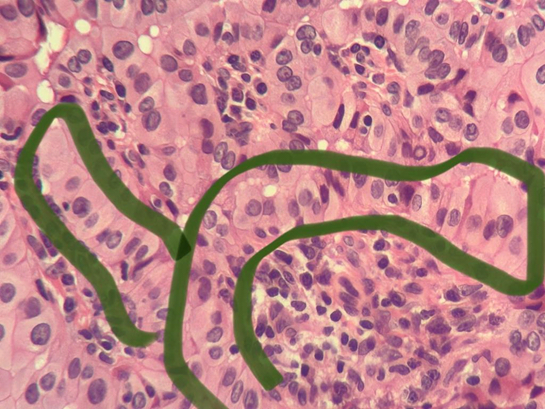
Figure 2 The pattern of tall cells is visualized framed in green. When they acquire an ordered pattern it is easier to visualize them. A cell height to width ratio of 3:1 is observed.
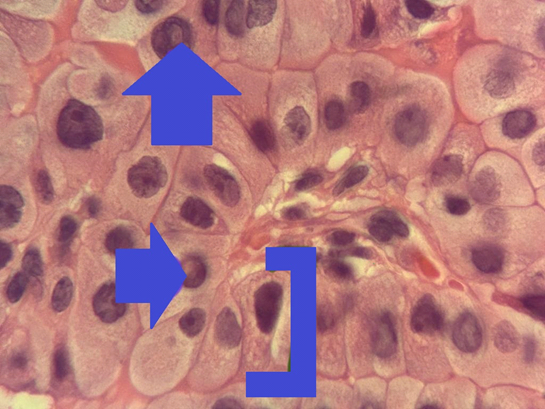
Figure 3 Atypical follicular cells are visualized. Blue arrows point to pseudo inclusions. Blue bracket frames a tall cell (clearly taller than wide). Abundant eosinophilic cytoplasm can also be seen.
Due to the anatomo-pathologic finding with a high cell pattern, it was decided to discuss in a multidisciplinary committee and the case was taken to the Endocrine Surgery Unit (UCE) of the Hospital de Clínicas. It was decided to complete the glandular resection.
Surgery was performed 3 months after the first intervention and the procedure was performed without incident. There were no postoperative complications. The patient was discharged 48 hours after surgery.
The incidence of High Cell Papillary Thyroid Carcinoma (HTC-PTC) is variable according to the literature with figures ranging from 1.3% to 13% of all PTC.5 Papillary thyroid carcinoma (PTC) according to its anatomo-pathologic variant is grouped according to its risk of aggressiveness and prognosis. The most aggressive and with the worst prognosis are those with tall cells, followed by the classic variant and then the follicular variant.6 This implies that clinical management depends on the specific variant.
CPT-CA is a poor prognostic factor independent of other factors such as age, size and extra-thyroidal extension.7 This type of lesion is more prone to extra-thyroidal extension, lymph node metastasis and to present as advanced stage disease.8 The diagnosis of this MCP CA subtype is obtained in most cases after the anatomo-pathologic study of the resection specimen. The size of the nodule and the limitations of FNA make pre-surgical diagnosis very difficult. The tall cell variant presents distinctive characteristics in its molecular basis that confer it a particular course with greater morbidity and mortality than its classic counterpart. The BRAFV600E mutation is the most common of the CPT9 is more frequent in CA CPT reaching figures close to 80% in some series.8,10 Also the RET/PTC rearrangements are also more frequent in these variants, reaching up to 36% of the cases.11
Mutations at the BRAF, TERT, RET/PTC level are more frequent in the high cell variants and are strongly associated with a more aggressive evolution and unfavorable prognosis.5,12 Such mutations are proposed as an early event in thyroid carcinogenesis that could be present even in micro carcinomas. This is important because molecular genetic studies can contribute greatly to therapeutic decisions.
The benefit of surgical treatment in early stages of MCP CA lies in improving the results by lowering the incidence of recurrence and metastasis.13,14 It should also be taken into account that this variant presents greater resistance to radioiodine treatment than the conventional variant. In a comparative study between MCP classic variant and MCP-CA, it was seen that the latter had 30% more extra-thyroidal evasion, slightly more lymphatic dissemination and BRAF mutated in 93% with respect to 77% in its classic variant. In short, the literature suggests that this type of high cell lesion is more aggressive and therefore treatment should be different from other MCPs. For this reason it is suggested that patients with CA CPT should undergo total thyroidectomy even when they present in MCP.15,16
CA CPTs present structural, phenotypic and genotypic characteristics that imply a different management from their classical variant, even if they are MCP. Although studies on the aggressiveness of MCP CA are scarce and retrospective, the greater tendency to loco regional invasion and recurrence and its lower response to radioiodine compared to its classic variant are factors that the surgeon must take into account when planning the extent of surgery.
None.
Authors declare that there is no conflict of interest.

©2023 Parada, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.