Journal of
eISSN: 2373-633X


Case Report Volume 10 Issue 6
1Department of Radiology, Webimagem, Brazil
2Department of Biomedicine, Universidade Paulista, Brazil
Correspondence: Márcio Luís Duarte, Department of Radiology, WEBIMAGEM, Avenida Marquês de São Vicente 446, São Paulo, Brazil
Received: December 09, 2019 | Published: December 16, 2019
Citation: Costa MGSV, Ito MH, Silva MO, et al. Splenic hamartoma–a rare finding. J Cancer Prev Curr Res. 2019;10(6):174-175. DOI: 10.15406/jcpcr.2019.10.00412
Splenic tumors are relative. Epidemiologically, splenic hamartoma can similarly affect both genders, regardless of age. Most patients are asymptomatic but there are some cases with hematological symptoms - anemia, thrombocytopenia, and infections, as well as clinical symptoms caused by the tumor mass. The objective of this work is to describe a case of splenic hamartoma highlighting its imaging findings.
Keywords: hamartoma, splenic diseases, magnetic resonance imaging
MRI, magnetic resonance imaging; CT Scan, computed tomography scan
The spleen is the largest lymphatic organ in the body, being of mesodermal origin.1 Splenic functions include immune surveillance, red blood cell degradation, and splenic contraction to increase blood volume during bleeding.1 The spleen is divided into two compartments – the red and white pulps separated by the marginal zone.1 The white pulp is composed of centrally located T and B lymphocytes, while the red pulp is composed of rich plexuses of tortuous venous sinuses.1
Splenic tumors are relatively rare and include malignancies such as lymphomas, angiosarcomas, plasmacytomas, primary malignant fibrous histiocytomas, and metastatic disease.1–4 The most common benign splenic lesions include:5
Splenic hamartoma was first described in 1961 by Rokitansky.3–7 Epidemiologically, splenic hamartoma can affect both sexes similarly, regardless of age, predominantly in older adults.5 About 20% of hamartoma occurs in children.8 They are usually diagnosed after splenectomies or autopsies.8 In this case report, we describe a case of splenic hamartoma diagnosed by magnetic resonance imaging.
A 47-year-old man with abdominal pain for one year. Refers to diffuse abdominal pain in abdominal palpation, mainly in the left flank. Denies trauma, allergies, and surgeries. Normal blood count and white blood count. CT scan demonstrated splenic nodule of nonspecific aspect. MRI demonstrated solid nodular formation within the splenic body, with lobulated contours, well-defined boundaries, with slight low-signal compared to the rest of the spleen in T1-weighted sequence and slightly high signal in T2-weighted sequence - with small cystic foci and enhancement soon after contrast infusion, compatible with hamartoma (Figures 1–3).
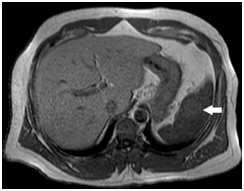
Figure 1 MRI axial section in the T1 sequence reveals an oval lesion in the spleen with a slight high signal relative to the rest of the parenchyma (white arrow).
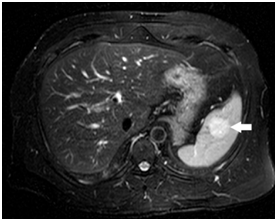
Figure 2 MRI axial section in the T2-weighted image reveals an oval-shaped spleen lesion with a high signal relative to the rest of the parenchyma (white arrow).
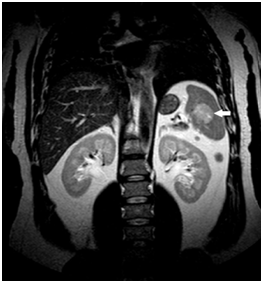
Figure 3 MRI coronal in the T2-weighted image reveals an oval lesion in the spleen with a high signal relative to the rest of the parenchyma (white arrow).
Since then, the patient has been in medical follow-up performing imaging exams annually, in which there have been no changes in size or appearance.
Pathologically, splenic hamartoma is characterized by a tumor-like proliferation of normal spleen tissues.5 Hamartoma exhibits expansive growth and compresses surrounding splenic tissue without a true capsule, and two major histological types are described: white pulp and red pulp.9 Most lesions are a mixture of both subtypes, either solitary or multiple lesions.9
Most patients are asymptomatic,10 but there are some cases with hematological symptoms - anemia, thrombocytopenia, and infections, in addition to the clinical symptoms caused by tumor mass.3 Only 15% of patients have symptoms, most commonly abdominal pain, splenomegaly, cytopenia, and accidental spontaneous rupture.9
Preoperative diagnosis using a combination of multi-modality imaging exams may be possible.4 Accurate preoperative diagnosis helps to avoid unnecessary surgery or biopsy and ultimately decrease the patient's overall morbidity.10
Ultrasonography reveals splenic hamartoma as well-defined, homogeneous solid masses with variable echogenicity relative to the normal splenic parenchyma, but other masses may be heterogeneous with cystic changes or, in rare cases, have a gross calcification secondary to ischemia or hemorrhage.9 Doppler shows increased blood flow.9 Color Doppler ultrasonography and ultrasonography with microbubble contrast, such as Levovist, are helpful.11 Contrast ultrasonography reveals a remarkable enhancement after Levovist injection.11
CT Scan reveals that splenic hamartoma is isodense or hypodense masses with prolonged enhancement following intravenous administration of contrast material.2 Also, image fusion between positron emission tomography (PET) using 18F-fluoro-2-deoxy D-glucose (FDG) with CT becomes an important tool in evaluating patients with a malignant disease or suspected lymphoma to evaluate other malignancies.2
The main differential diagnosis is a hemangioma, and MRI is the most appropriate technique to differentiate them.2,4,12 Most lesions are isointense in T1-weighted images and heterogeneously hyperintense in T2-weighted images.12 In dynamic contrast sequences, it is typical to see low and heterogeneous enhancement in immediate post-contrast images.12 These are the key features of the differentiation between hamartoma and hemangiomas.12 In delayed post-contrast imaging, the hamartoma is relatively uniformly and intensely reinforced and may reveal areas with poor central vascularization.12 Recently, less invasive treatments such as laparoscopy-assisted surgery have been developed.2
Not applicable.
The authors declare that there is no conflict of interests regarding the publication of this paper.
The written informed consent of the patient was obtained, for the publication of her case.

©2019 Costa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.