Journal of
eISSN: 2373-633X


Case Report Volume 8 Issue 2
Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, Qatar
Correspondence: Sushila B Ladumor, Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, P.O. Box 3050, Doha, Qatar, Tel 97466430597
Received: April 22, 2017 | Published: July 17, 2017
Citation: Ladumor SB, Darweesh A. Renal sinus cyst. J Cancer Prev Curr Res. 2017;8(2):237-239. DOI: 10.15406/jcpcr.2017.08.00272
Renal sinus cysts are benign. Cysts involving the renal pelvis are classified as Para pelvic or peri pelvic cyst (renal sinus cyst) according to their site of origin.
Para pelvic cyst: originate from the adjacent parenchyma and protrude into the renal sinus. Histologically, they are lined with a single epithelial layer. These are simple renal cysts that extends into the renal sinus from the adjacent renal parenchyma. They are usually single or few and resemble simple renal cortical cyst in morphology.
Pera pelvic cyst: originate within the sinus itself and have a lymphatic origin. A para pelvic cyst sometimes may cause compression of the pelvicalyceal system resulting into hydro nephrosis.
Renal sinus cysts are many times diagnosed as hydro nephrosis by renal ultrasound as sometimes is it very difficult to differentiate between renal sinus cysts and hydro nephrosis. (As in this case patient presented with left loin pain).
It is very important to keep in mind that renal sinus cyst as differential diagnosis of hydro nephrosis and asking patient about his/her previous history or any previous exam. CT urography or intravenous urography very well differentiate and demonstrate a normal or narrowed/stretched/displaced (but not dilated) collecting system.
NECT, non-enhanced computerized tomography; CECT, contrast enhanced computerized tomography; USG, ultra-sonography
49yr old male patient with left loin pain. Patient referred for Renal Ultrasound for evaluation of urinary stone and obstruction. Renal Ultrasound reveals: Left mild hydro nephrosis. Renal pelvic was not demonstrated. No stone. No hydro ureter (Figure 1). Non-contrast CT recommended after as Ultrasound reveal left hydro nephrosis and failed demonstrating stone.
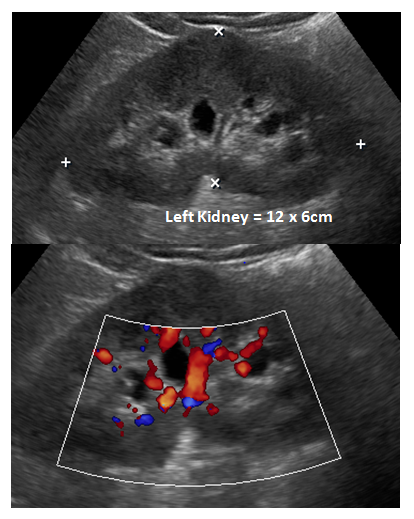
Figure 1 Renal ultrasound recommended ruling out urinary stone. Ultrasound demonstrates left mild hydro nephrosis. Renal pelvic was not demonstrated. No stone. No hydro ureter.
Non-contrast CT
Again appears as left mild hydro nephrosis without stone and hydro ureter. CT urogram performed and reveals no hydro nephrosis. No stone in kidneys, ureters and urinary bladder. Re-demonstration of cystic structures from left renal pelvis extending alongside of non-dilated pelvi calyceal system. Incidentally noted mesenteric root fat stranding with multiple lymph nodes, representing mesenteric panniculitis.1–3
Parapelvic cysts
These are simple renal cysts that plunge into the renal sinus from the adjacent renal parenchyma. They are usually single or few and resemble simple renal cortical cyst in morphology. A parapelvic cyst at times may cause compression of the pelvicalyceal system resulting into hydronephrosis.
Peripelvic cysts
These are frequently bilateral. They appear as water attenuation cysts closely abutting the pelvis and infundibula; rarely cause functional renal derangement by compression. When followed up they remain unchanged in size. They may be confused with hydronephrosis on NECT and USG, but on CECT the differentiation is obvious.
Differential diagnosis
Renal sinus cysts can mimic hydronephrosis but CT/ IVP studies will demonstrate a normal or narrowed/stretched/displaced (but not dilated) collecting system. Renal sinus cysts (sometimes referred to as peripelvic cysts) are asymptomatic cysts that arise from the lymphatics of the renal hilum. Peripelvic renal cysts defined as cysts which are situated in the renal hilus, intimately related with the renal pelvis and calyces. It can be simple or multiloculated and single or multiple. Peripelvic cyst are not buried within renal parenchyma and not appearing as mass in polar region or as exophytic on renal surface like simple renal parenchymal cyst. Usually they compress and displace the renal pelvis and vascular pedicle. If they are large, they may protrude from the renal hilum.
Their appearance is often difficult to distinguish from hydronephrosis in Ultrasound and non-contrast CT. However, the distinction is readily apparent on contrast-enhanced excretory phase CT images, where the high-attenuation contrast agent–filled collecting system can easily be distinguished from fluid-attenuation renal sinus cysts. Peripelvic cysts which are large enough to cause symptoms or be detectable radiographs are rare and have rarely reported in the urological or radiological literature (Figure 2).

Figure 2 Axial Images: CT urogram was advised to exclude stone. CT urogram shows no hydro nephrosis. No stone in kidneys, ureters and urinary bladder. Re-demonstration of cystic structures from left renal pelvis extending alongside of calyceal system. Incidentally noted mesenteric root fat stranding with multiple lymph nodes, representing mesenteric panniculitis.
Mesenteric panniculitis
Mesenteric panniculitis is a rare disorder characterized by a chronic nonspecific inflammation involving the adipose tissue of the bowel mesentery. The cause of the disease is unclear. Autoimmune response to unknown sources and ischemia of the mesentery has been proposed as pathogenic mechanisms. Whether mesenteric panniculitis occurs independently or in association with other disorders is not yet clear. The disease has been related to a variety of conditions such as vasculitis, granulomatous disease, rheumatic disease, malignancies, and pancreatitis.
The condition mostly in middle or late adulthood with a slight male predominance. When symptomatic, patients may present with a palpable abdominal mass and systemic manifestation, including abdominal pain, pyrexia, weight loss, and bowel disturbance of variable duration. Symptoms may be progressive, intermittent, or absent. Laboratory findings, including elevation in erythrocyte sedimentation rate and anaemia, are absent or nonspecific. Complete resection of the mass is usually impossible and is generally considered to be of not curable or beneficial. In most cases the mesenteric panniculitis is incidentally identified during a CT examination for an unrelated condition as in this study (Figure 3 & 4).
The disease was usually asymptomatic and frequently associated with abdominal or distal malignancy. CT features, including the envelopment of the superior mesenteric vessels by a well-delineated fatty mass, the displacement of adjacent bowel loops, well-defined soft-tissue nodules less than 5 mm, a fatty halo, and a hyper attenuated stripe, may enable
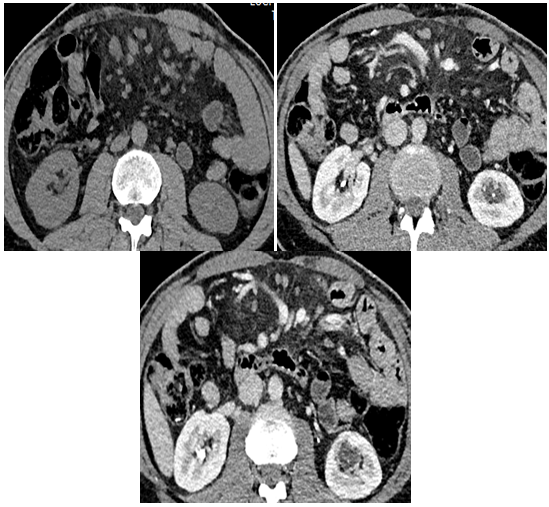
Figure 3Axial Images: CT urogram was advised to exclude stone. CT urogram shows no hydro nephrosis. No stone in kidneys, ureters and urinary bladder. Re-demonstration of cystic structures from left renal pelvis extending alongside of non-dilated calyceal system. Incidentally noted mesenteric root fat stranding with multiple lymph nodes, representing mesenteric panniculitis. Non-contrast study for comparison.
None.
Authors declare that they have no conflict of interest.
None.

©2017 Ladumor, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.