Journal of
eISSN: 2373-633X


Research Article Volume 5 Issue 6
1Department of Pathology, University of Hail, KSA
2Department of Histopathology and Cytology, University of Khartoum, Sudan
3Department of Medical Laboratory, University of Kordofan, Sudan
4Department of Histopathology and Cytology, Sudan University for Science and Technology, Sudan
5Department of Medical Lab Science, University of Hail, KSA
Correspondence: Hussain Gadelkarim Ahmed, Department of Pathology, College of Medicine, University of Hail, 2440, Kingdom of Saudi Arabia
Received: August 31, 2016 | Published: September 21, 2016
Citation: Ahmed HG, Beely MABI, El Aziz MSA, et al. Prevalence of high risk human papilloma viruses 16 and 18 (HR-HPV16&18) among Sudanese patients with esophageal cancer.J Cancer Prev Curr Res. 2016;5(6):355‒358 DOI: 10.15406/jcpcr.2016.05.00181
Objective: The aim of this study was to screen for the presence of High Risk Human Papilloma Viruses 16 and 18 (HR-HPV16&18) among Sudanese patients with esophageal cancer.
Methodology: The study was retrospectively examined 100 formalin fixed paraffin wax embedded tissue’s blocks for the presence of HR-HPV subtypes 16 and 18 by Immunohistochemical methods. All samples were previously obtained from Sudanese patients with esophageal cancer.
Results: Regarding IHC staining for HPV 16 and 18, positive findings were revealed in 13 (13%) and couldn't be disclosed in 88 (87%) of the study subjects, hence, none of the cases was identified with HPV18.
Conclusion: HR-HPV subtype 16 is strongly contributed to the etiology of esophageal carcinoma in Sudan. Urgent preventive strategies are highly recommended to reduce the burden of esophageal cancer in Sudan.
Keywords: esophageal cancer, Sudan, hpv16, hpv18
Esophageal cancer, usually involve esophageal squamous cell carcinoma (SCC) and esophageal adenocarcinoma (AC), is one of the most common malignant tumors in the world.1 Esophageal cancer is the sixth leading cause of cancer death in the world.2 Esophageal squamous-cell carcinoma and esophageal adenocarcinoma represent the core histological subtypes of esophagus cancer.3 Esophageal carcinoma represents a poor prognosis among gastrointestinal cancers. While esophageal squamous cell carcinoma predominates worldwide, Western nations have seen a marked rise in the incidence of esophageal adenocarcinoma that parallels the obesity epidemic. Efforts directed toward early detection have been difficult, assumed that dysplasia and early cancer is generally asymptomatic. However, significant developments have been made in the past 10 to 15years that permit for endoscopic management and often cure in early stage esophageal malignancy.4
Many factors have been incriminated to the etiology of esophageal cancer. The carcinogenesis of esophageal AC is initiated by the acid exposure of the esophageal mucosa from stomach5 whereas that of the esophageal SCC is linked to the chronic irritation of carcinogens mainly by the cigarette smoking,6 alcohol7 and hot beverage.8 A potential role of HPV in the rise of esophageal AC was proposed recently. Multiple meta-analyses support the outcome of a higher HPV detection rate in regions associated with high risk for esophageal SCC compared to low-risk areas.9 A meta-analysis showed that HPV16 and 18 can be detected in esophageal SCC. HPV16, but not HPV18, is significantly associated with the risk of esophageal SCC.10 Therefore, the objective of the present study was to screen for the presence of High Risk Human Papilloma Viruses 16 and 18 (HR-HPV16&18) among Sudanese patients with esophageal cancer.
The present study investigated 100Sudanese patients with esophageal cancers, 54were males and 45were females (male/female ratio, 1.20:1.00), aged between 12 and 98years with mean age of 60years old, were diagnosed as having esophageal carcinomas, were investigated for the presence of HR-HPV subtypes 16&18 using C1P5 (HPV16 E6/18 E6 Antibody) immunohistochemistry. Immunohistochemical positive results were further confirmed by Polymerase Chain Reaction (PCR). The diagnosis was based on clinical examination and histological features of the biopsy. Esophageal cancer diagnosis was confirmed base on Royal College of Pathologists criteria (Royal College of Pathologists, 2005). The esophageal cancer including 90/100 (90%) squamous cell carcinomas (SCCs) and 10/100 (10%) adenocarcinoma. The sample included full coverage of patients with esophageal lesions referred to Radiation and isotope Centre Khartoum with available sample quantity and data. Ethical consent was obtained from ethical committee of the Faculty Research Board and Hospital.
C1P5 immunohistochemistry (IHC) was performed on formalin-fixed paraffin embedded (FFPE) tissue sections using kits from (Dako Agilent Technologies Company). After antigen retrieval, sections were incubated with mouse monoclonal C1P5, and then En Vision_ System HRP anti-mouse, followed by diaminobenzidine (DAB) chromogen and counterstaining with hematoxylin. Cervical cancer sections known to be HPV-positive were used as a positive control, and omission of primary antibody was used as a negative control. All C1P5 IHC slides were semi quantitatively scored by two investigators for intensity of staining in the cell nucleus and cytoplasm. Intensity was scored as 0 (none), 1(weak), 2 (moderate), or 3 (strong), with 0 or 1 scores defined as negative and 2 or 3 defined as positive. C1P5 scoring was performed without knowledge of HPV infection status.
This study investigated 100 tissue samples which were obtained from Sudanese patients with esophageal carcinoma (90 patients were with squamous cell carcinoma and 10 were with adenocarcinoma). Of the 100 study subjects 54 were males and 45 were females their age ranging from 12 to 98 years old with a mean age of 60 years. The majority of the study populations were at the age range 66-75years constituting 26 patients followed by age ranges, both 56-65 and <45years representing 24 patients. Moreover, 16 patients were identified among age group 46-55years, hence only 10 patients were found among age group 76+years, as indicated in (Figure 1).
However, most of the patients were diagnosed as having Squamous cell carcinoma representing 90% followed by Adenocarcinoma representing 10%. Of the 90 patients with Squamous cell carcinoma, 52% were males and 48% were females. Of the 10 patients with Adenocarcinoma 73% were males and 27% were females.
Regarding IHC staining for HPV 16 and 18, positive findings were revealed in 13/100 (13%) and couldn't be disclosed in 87 (87%) of the study subjects, hence, none of the cases was identified with HPV18 (confirmed by PCR), as shown in Microphotograph 1 & 2. The risk associated with HPV 16 as etiological factor for esophageal cancer and the Odd Ratio (RO) and the 95% confidence interval was 31(1.81-528), P <0.017. Of the 54 males with esophageal cancer, 7/54 (12.9%) were identified with HPV16 infection and the remaining 47/54(87.1%) found without HPV16 infection. Of the 45 females with esophageal cancer, 6/45(13.3%) were found positive for HPV 16 immunostaining and the remaining 39/45(86.7 %) were found negative for HPV16.
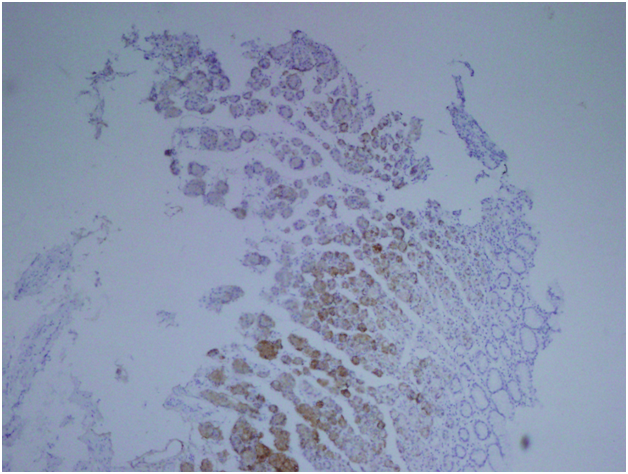
Microphotograph 1 Esophageal carcinoma showing positive HPV16 expression (Immunohistochemical staining using C1P5 antibody), En Vision_ System HRP. X100.
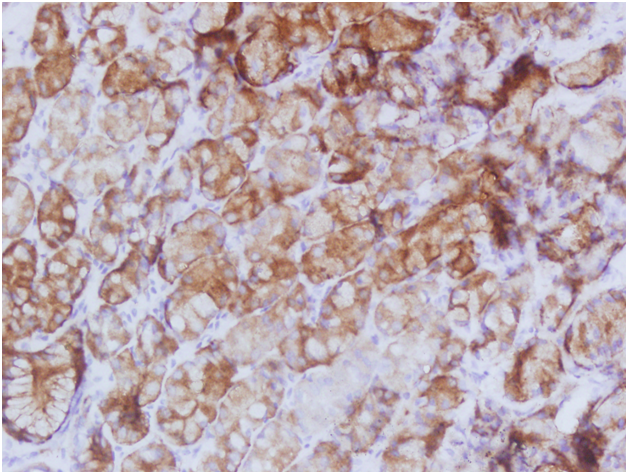
Microphotograph 2 Esophageal carcinoma showing positive HPV16 expression (Immunohistochemical staining using C1P5 antibody), En Vision_ System HRP. X400.
The association of HPV 16 risk with sex was OR (CI)=0.97(0.30-3.12), P<0.9.
According to cancer type, of the 90 cases of the Squamous cell carcinoma, 11/90 (12.2%) were found with positive HPV16 and the remaining 79/90 (87.8%) were negative. Of the 10 cases of the Adenocarcinoma, 3/10(30%) were found with positive HPV16 and the remaining 8/10 (70%) were negative, as indicated in Table 1. The association of HPV 16 risk with Adenocarcinoma was OR (CI) = 0.37(0.084-1.56), P<0.18, as indicated in (Table 1) & ( Figure 2).
Sex |
Positive |
Negative |
Total |
Males |
7 |
47 |
54 |
Females |
6 |
39 |
45 |
Total |
13 |
87 |
100 |
Cancer Type |
|||
Squamous |
11 |
79 |
90 |
Adenocarcinoma |
3 |
7 |
110 |
Total |
14 |
86 |
100 |
Table 1 Distribution of IHC results of HPV subtypes 16, 18 by sex and cancer type
Concerning IHC staining results of HPV subtypes 16, 18 with age distribution, the highest positive results were found in age group 66-75 years, representing 6(23%), followed by (<45& 56-65) and 46-55 constituting 3(12.5%) and 1(6.3%) respectively, where's; the groups with the highest negative results were <45 and 56-65 years, representing 21(23.6%) in each followed by 66-75,46-55 and 76+ constituting 20 (22.5%), 15 (16.8%) and 12(13.5%) in this order, as shown in (Table 2) & (Figure 3).
Age Group |
Positive |
Negative |
Total |
<45 years |
3 |
21 |
24 |
46-55 |
1 |
15 |
16 |
56-65 |
3 |
21 |
24 |
66-75 |
6 |
20 |
26 |
76+ |
0 |
10 |
12 |
Total |
13 |
87 |
100 |
Table 2 Distribution of IHC results of HPV subtypes 16, 18 by age
HR-HPVs particularly subtypes 16 and 18 have been linked to the etiology of several cancers including esophageal cancer. However, there is a lack of data regarding the relationship between HPV infection and esophageal carcinoma in the Sudan. Thus the present study is an attempt to explore the role of HPV in the etiology of esophageal cancer and to stimulate further research in this area.
The present study found a prevalence of 13% of HR-HPV16 infection among Sudanese patients with esophageal cancer.HPV related esophageal SCC detection rates are greatly variable across different countries. Geographic location likely accounts for a majority of the variation in HPV prevalence, with high-incidence regions including Asia reporting significantly higher HPV related esophageal SCC infection rates compared with low-incidence regions such as Europe, North America, and Oceania.11 Studies have shown that Asia is high-risk region.12–14 In a meta-analysis study, an overall HPV prevalence of 30.6% was calculated, but a region-specific infection rate of 10.1% for Canada and the United States.12 There was evidence of an increased risk of esophageal SCC in patients with HPV infection odds ratio (OR) 2·69, 95% confidence interval (CI) 2·05-3·54. The prevalence of HPV in esophageal SCC was found to be 24·8%. There was an increased risk associated with HPV-16 infection (OR 2·35, 95% CI 1·73-3·19). Subgroup analyses showed geographical variance, with Asia (OR 2·94, 95% CI 2·16-4·00), and particularly China (OR 2·85, 95% CI 2·05-3·96) being high-risk areas.14
However, we didn’t found any literature regarding the relationship between esophageal carcinoma and HPV reported from Sudan. In study to determine the frequency and genotype of human papillomavirus (HPV) infections in head and neck squamous cell carcinomas (HNSCCs),6 of the 150 (4%) HNSCCs were HPV positive. HPV16 was the most prevalent type, with single infections present in 3/6 (50%) cases, whereas HPV18 and HPV33 were detected in 2/6 (33%) and 1/6 (17%), respectively. HPV infections were detected in 3 (50%) cases of oral cavity and 3 (50%) cases of pharynx.15
In the current study the detected cases of HPV infections were infected with HPV16 when further confirmed with molecular tests. Such findings were reported in several studies. In a study investigated 8990 esophageal squamous cell carcinoma (SCC) patients and 174 esophageal adenocarcinomas patients, the prevalence of HPV in esophageal SCC was 22.2%, HPV16 was the most frequently observed subtype with a summarized prevalence of 11.4% . With respect to esophageal adenocarcinoma, HPV prevalence was 35.0% (95% CI, 13.2-65.7%) and HPV-16 prevalence was 11.4%. Significant association was observed between HPV infection and esophageal SCC with a summarized odds ratio of 3.32 (95% CI, 2.26-4.87). According to HPV16, the strength of the association was found to be 3.52 (95% CI, 2.04-6.07).16 Though HPV18 was not detected in the present study but studies have reported low prevalence rates in the highly infected regions.17
Although the prevalence of esophageal cancer was higher among males, but the prevalence rates of HPV16 were relatively similar for both sex. However, we didn’t come across study showing significant variation in the prevalence of HPV infections in regard to the sex. When calculating the prevalence rate from the same number of sex, it appears greater among females due to the low number of females in regard to the total number of the study population. In the present study we observed variable frequencies among different age ranges, but the HPV infection was more frequent among elder population. The limitations in this study include; it’s retrospective setting and the strict detection of only two HR-HPV subtypes. This in addition to the missing of some demographical data. But still it has a value in directing further studies in this context.
HR-HPV subtype 16 is strongly contributed to the etiology of esophageal carcinoma in Sudan. Urgent preventive strategies are highly recommended to reduce the burden of esophageal cancer in Sudan.
None.
Authors declare that there is no conflict of interest.

©2016 Ahmed, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.