Journal of
eISSN: 2373-633X


Research Article Volume 14 Issue 3
1High Private School of Engineering and Applied Technologies IHE-ESPITA, Tunisia
2Research Unit: Molecular Biology of Leukaemia and Lymphoma, Department of Biochemistry, Medicine Faculty of Sousse, Tunisia
3Unit of Medical Biology Laboratories, Ministry of Public Health, Tunisia
Correspondence: André Tshimanga Ndaye, Higher Private School of Engineering and Applied Techniques (IHE-Espita), 4000, Sousse, Tunisia
Received: June 30, 2023 | Published: July 18, 2023
Citation: Ndaye AT, Knani SA, Moussa HD, et al. Performing first application (REST API) for adaptive palliative care facility in Alzheimer’s disease. J Cancer Prev Curr Res. 2023;14(3):70-72. DOI: 10.15406/jcpcr.2023.14.00523
Alzheimer’s disease is considered as the third major cause of disability after cardio-cerebro vascular diseases and cancers. Patients with this neuropathology must be followed-up on the first day of the diagnosis as well as during the development of the pathology so as to avoid a rapid degradation of their health and ensure better outcomes. We use Representational State Transfer Application Programming Interface (REST API) to closely follow up patients diagnosed with Alzheimer’s disease. We integrate the FMRIB Software Library (FSL) in this application in order to facilitate neuroimaging analysis and interpretation. Alzheimer’s disease involves several medical stakeholders. Through this application, we coordinate between the various healthcare activities to provide a better follow-up for patients. For the first time, we have created REST API for Alzheimer's follow-up to overcome the overall difficulties related neuroimaging diagnosis, medical records managing, and clinical coordination between evolved healthcare givers. Through this REST API, we targeted the most critical points which represented an obstacle for an efficient follow-up of Alzheimer’s patients.
Keywords: neurodegenerative disorder, Alzheimer’s disease, palliative care, neuroimaging, REST API
According to the latest statistics provided by the World Health Organization (WHO), the Alzheimer’s Disease (AD) is one of the most common neurodegenerative disorders in the world. There are approximately 46.8 million Alzheimer patients across the world. According to estimates, this number will increase to reach 114 million patients by 2050.1 AD is seen as the third major cause of disability after cardiovascular and cerebrovascular diseases as well as cancers. As a result, this will have serious social impacts and increase economic burden on international public healthcare systems.2
The etiology of the AD remains not well defined as many factors are involved. Until now, there has not been any efficient treatments. Most of them are preventive or symptomatic. They help improve patients’life quality and delay their total disability, which could lead to death. For this reason, early diagnosis is highly recommended. The diagnosis of neurodegenerative diseases is multi-parametric which includes clinical tests. The goal is to identify the AD from other forms of dementia. Despite the various clinical diagnoses, the neuroimaging remains the most promising approach. The neuroimaging diagnosis is an expanding area of research used to detect the AD.3 The prominent advances made in this field allowed a better characterization even an anticipation of diagnosis in patients with high-risk or presenting some genetic predisposition to develop this neuropathology.
The absence of efficient treatments highlights the importance of identifying new reliable neuroimaging biomarkers for an early diagnosis even before symptoms are displayed.4 A variety of neuroimaging approaches may be very useful for anticipated diagnosis such as Positron Emission Tomography scan or PET scan,5 Computed Tomography Scan (CTS)6 and Magnetic Resonance Imaging (MRI).7 The MRI is still the most common approach used for AD diagnosis in routine investigations.8 Extracting clinical data from MRI neuroimaging represents on itself a big challenge.
Providing medical care to Alzheimer’s patients constitutes another challenge for the healthcare professionals. Patients should be provided a close medical follow-up immediately after the first day of the diagnosis as well as during the development of this neuropathology. The goal is to avoid the exacerbation of their overall health and ensure better outcomes.
The clinical follow-up generates several multidisciplinary medical records. As a chronic disease, the AD requires the involvement of various healthcare stakeholders including neurologists, physiotherapists, radiologists, psychologists, neuroimaging technicians and medical biologists working in laboratories. This medical follow-up will generate medical data, which are crucial for health monitoring. These extensive medical records have to be saved and provided to the above-mentioned caregivers throughout the development of the disease. It is worth mentioning that this is not an easy process at all considering the large number of medical records as well as the number of stakeholders involved.
Throughout this study, we are aiming to create a Representational State Transfer Application Programming Interface (Rest Api) so as to ensure a better follow-up of patients diagnosed with AD.
The Rest Api is a style of software architecture defining a set of constraints that we adopt to create web services. These web services allow requesting systems to manipulate web resources via their text representations through a set of uniform, predefined stateless operations. The Rest Api have been developed and adopted in several domains, particularly in the medical field. They have advantages to be easy to design and much easier to integrate them into mobile devices.
In our project, the REST Api was created with the aim to overcome difficulties related to the AD monitoring. It stands as a powerful tool: First, it conducts an MRI neuroimaging investigation using FSL Software Library access that we integrate in our Rest APi. Secondly, it manages the neuroimaging data and medical records generated while monitoring AD patients. Thirdly, it provides a better adaptive palliative care services. Finally, it ensures close coordination between healthcare professionals by providing data access to all records regarding AD patients during follow up and the disease development.
Rest Api: A Representational State Transfer Application Programming Interface (REST Api) is a method using the hypertext transfer protocol (HTTP), to execute specific actions.
It provides a set of protocols and services accessible by programs. The Representational State Transfer (REST) offer access through resources, illustrates resources by representations, exchanges self-descriptive messages and uses links to connect resources. The Rest API architecture intended to transfer a representation of server data between Healthcare providers/ Patients and server in back end integrations.9,10 The architecture Network are presented in Figure 1,2.
REST Apis are all following the same process allowing a direct integration of the research database into the software applications. In our case we develop, a Rest Api to manage clinical follow up of patients diagnosed with AD and achieve medical care coordination. It also provides efficient MRI neuroimaging analysis and save all generated medical records.
FSL Brain: The FMRIB Software Library (FSL) is a comprehensive library of analysis tools for functional, structural and diffusion MRI brain imaging data.11
We adopted and integrated this software into our Rest API because it contains several powerful tools allowing the extraction of significant and relevant informative datafrom MRI records. This leads to a better characterization of dementia, especially in AD. Among these tools, we find:
MRI records: Records from Patients diagnosed with AD were obtained from OASIS (Open Access Series of Imaging Studies) database (http://www.oasis-brains.org/). This open access database contains axial brain MRI images of 416 people aged between 18 and 96.100 of them had moderate mild dementia AD based on a clinical CDR (Clinical Dementia Rating) diagnosis. These MRI records served to test the FSL brain tool that we integrated into the Rest API.
The evolution of technology has led to the emergence of new concepts such as Rest Api that made great strides in several areas mainly medical field. The evolution of microservices was to expose its functionality through HTTP-based REST services. These microservices are an architectural and organizational approach allowing to development software, in which the software consists of small independent services that communicate via well-defined APIs. In this monolithic architecture, all components merge into a single module (Figure 1, 2).
Through our investigation, we performed a Rest Api for a better follow-up of AD patients by targeting the major critical points including neuroimaging investigation and records managing. The home interface of the developed web application is composed of a menu allowing the administrator (main doctor) and associated doctors, nurse, medical secretary’s access to the different functionalities according to their specific tasks to manage (Figure 3).
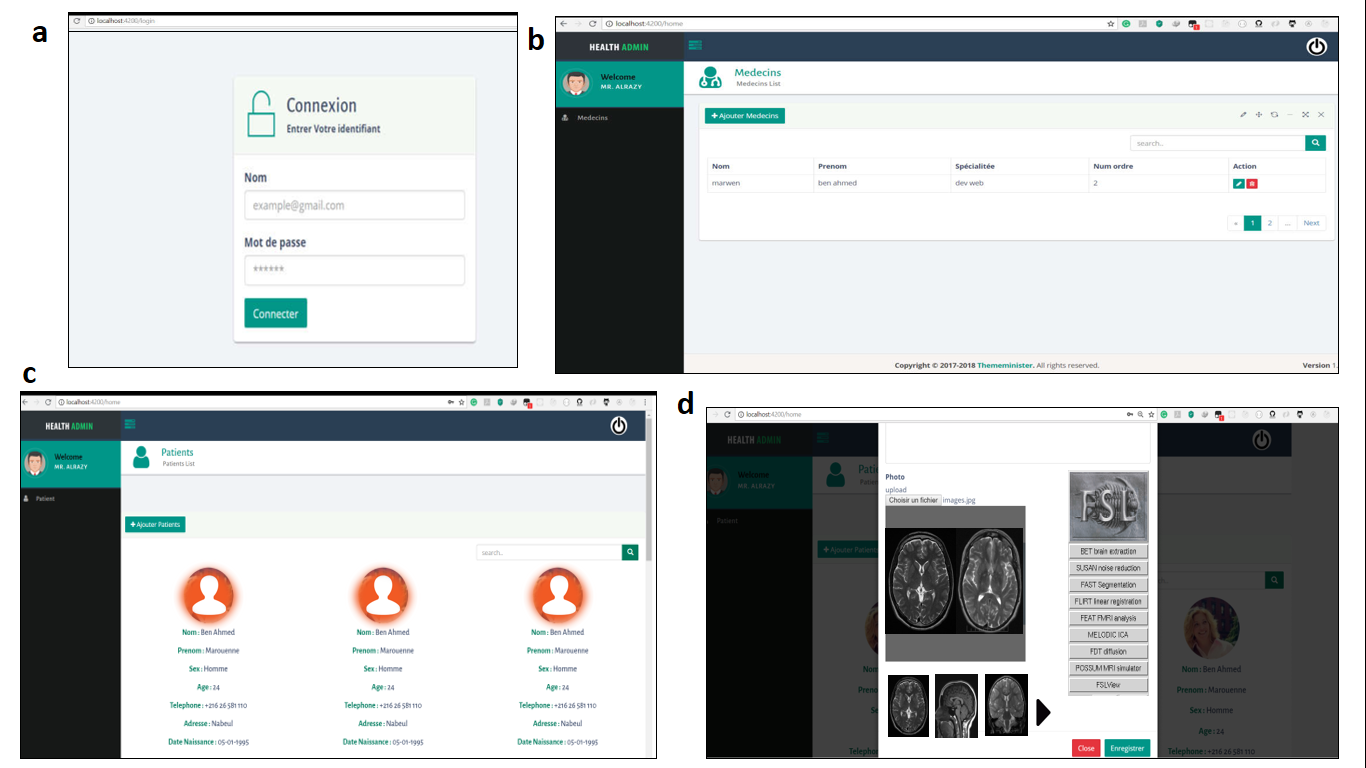
Figure 3 API Rest interface: a, administrator session access; b, associated doctors’ sessions; c, patients sessions; d, MRI imaging storage and analysis trough FSL brain tool.
In fact, our system must establish the following features according to established architecture Network (Figure 1-2). The main features consist in the identification and registration of administrator who is the main doctor following the Alzheimer patients. The management of involved doctors or healthcare providers by the administrator: it consists in the addition/suppression, the consultation, the sending of emails and any type of authorization, also tracking patients’ appointments. Moreover, sending and receiving automatic confirmation emails between the administrator and the healthcare providers and intervening doctors. The numerical MRI analysis data generated during patient’s follow-up should be download and registered on PACS or RIS format.
This Rest Api provides full access to FSL brain library and associated tools for functional, structural and diffusion MRI brain imaging data analysis as well generates reports and interpretation of neuroimaging records by the main or associated doctors. For that our application allows the categorization of co-doctors involved for AD patient diagnosis and follow-up: neurologist, radiologist, psychologist, and geriatrist. The generated medical reports will be recorded and accessible by the administrator and all involved doctors and health care providers. The request for advice between co-doctors and access to all records and medical reports of patients and the possibility to call the doctor in case of emergency has been envisaged.
Over the past years, technological advances have greatly increased the range of data types especially in health care through standards open software or Rest APIs. The REST API is very easy to adopt using HTTP requests from simple command tools such as cURL or a web browser especially with the huge numerical progress nowadays.15 Many challenges need to be considered, such as effective early diagnosis and follow-up of AD patients to palliate the symptoms during the disease progression. Through these simple programmatic methods REST Api, we aim to overcome all these difficulties.
First, by performing neuroimaging analysis by integrating a complete FSL tools (BET, FAST, FIRST...) that allow a better functional and structural interpretation and provide valuable clinical data extraction. These clinical data allow better evaluation of disease progression and improve prognostic evaluation. Secondly, this application coordinates the medical healthcare provider’s acts. The follow-up of AD involves several medical disciplines such as neurology, radiology, general medicine, geriatrics.
In our REST Api (Figure 3), we suppose the neurologist as a major administrator. The administrator will suspect neurodegenerative symptoms after conducting neurological tests. Thus, the neurologist can add other clinicians as secondary administrators to confine the diagnosis, especially the radiologist making an MRI neuroimaging investigation. The major administrator can even involve other doctors when needed such as a family doctor, geriatrician and physiotherapist for the follow-up during the disease progression.
This REST Api, allows the communication between all intervening healthcare providers and access to all clinical data, records and medical statements. Through this network managed by our application, we seek to facilitate communication of important medical information to carry out an efficient follow-up of AD. We proceed continuous updates for our performed REST Api based on feedback from users, in order to make sure the efficiency of patients follow-up and provide more functions for neuroimaging analysis.
The use of simple programmatic methods in chronic illnesses such as Alzheimer's disease can be a prominent alternative to provide more efficient healthcare services. Through this project, we have adopted for the first time the use of Representational State Transfer Application Programming Interface in the service of neurodegenerative disease.These findings present a new tool providing better health care services not only in neurodegenerative diseases but also in all chronic pathologies, which involve adaptive follow-up. The expansion need of medical APIs in our modern life can be a perspective to African engineer to perform valuable service through Rest Api development.
The Private Higher School of Engineering and Applied Technologies IHE-ESPITA has supported this work. We would like to extend our thanks to the IT-GATE institution for its contribution and Mr. Helmi Ben Aziza for the English revision.
We declare no competing interests.

©2023 Ndaye, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.