Journal of
eISSN: 2373-633X


Research Article Volume 4 Issue 6
1Division of Medical Oncology, Aga Khan University Hospital Nairobi, Kenya
2Department of Radiology, Aga Khan University Hospital Nairobi, Kenya
3Department of Pathology, Aga Khan University Hospital Nairobi, Kenya
Correspondence: Asim Jamal Shaikh, Assistant Professor, Division of Medical Oncology, The Aga Khan University Hospital Nairobi, 30270, Kenya
Received: December 04, 2015 | Published: May 12, 2016
Citation: Shaikh AJ, Sikosana MLN, Nguku S, et al. Malignant pervascular epitheloid cell tumor (PEComa), presenting as a large intra-abdominal mass in a young woman: a case report and review of literature. J Cancer Prev Curr Res. 2016;4(6):181-183. DOI: 10.15406/jcpcr.2016.04.00142
Introduction: Perivascular epithelioid cell tumors (PEComa) are rare mesenchymal tumors of variable biologic behavior. Information on epidemiology, risks, treatment and prognosis is extremely limited.
Case presentation: We are presenting case of a 20 years old girl, who presented with huge retroperitoneal PEComa, deemed un-resectable due to encasement of the major vessels and extreme friability. Treatment response was poor to Adriamycin based chemotherapy. She however responded to mTOR signaling pathway blocking therapy for a short time before gross progression and massive pleural effusion.
Conclusion: Malignant PEComas are very rare mesenchymal tumor; there is a need of better understanding of pathophysiological and molecular pathways of this rare but potentially fatal malignancy in order to define the best possible treatments.
Keywords: PEComa, mTOR, rare cancer
PEComa, perivascular epithelioid cell tumors; mTOR, mammalian target of rapamycin; CD, cluster designation; CEA, carcino embryonic antigen; AE, anti pankeratin; EMA, epithelial membrane antigen; HMB, human melanoma black; CT, computerized tomography; TSC, tuberous sclerosis complex
PEComas (Perivascular epithelioid cell tumors) are extremely rare mesenchymal tumors composed of distinctive, perivascular epitheloid cells, first described in 1992 by Bonetti et al.1 The term PEComa was introduced by Zamboni et al.2 a few years later.2 There are a few cases of PEComas that have been described so far and treatment modalities are controversial. We present a case of a young lady with a huge intra-abdominal PEComa. We discuss various treatment approaches and response patterns. A review of literature on treatment modalities of PEComa is also presented.
A 20 year old female was referred from a primary care physician with one year history of increasing palpable abdominal mass associated with progressively worsening left flank pain. She reported no other symptoms during this period, except significant anorexia. There was no family history of malignancy ant there were no features suggestive of tuberous sclerosis. On Examination She had a palpable non tender mass arising from umbilical region extending to Pelvis up to the left flank. The mass was firm, immobile and non-tender. A complete blood count revealed a normocytic normochromic mild anemia. The liver function tests were normal and She had normal electrolytes, urea and serum Creatininie levels as well. A CT-Scan abdomen revealed multiple avidly enhancing masses in the retro peritoneum and left kidney. The mass measured 15cm in greatest dimension and appeared to be primarily arising from the retro peritoneum and left kidney (Figure 1a). There were associated necrotic para-aortic nodes. A tumor thrombus was present in the left renal artery (Figure 1b). Rest of the abdominal and pelvic organs was normal.
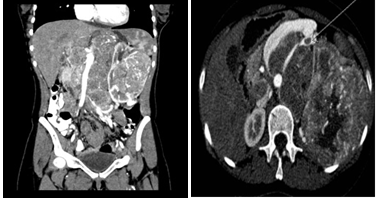
Figure 1 a) Abdominal CT image, Coronal reformat showing left renal mass and retroperitoneal masses. b) Axial CT image showing left renal artery thrombus.
CT scan of Chest was negative for metastasis. Attempts to get biopsy from this mass failed as repeat attempts revealed necrotic tissue only. She subsequently underwent an attempt at laparoscopic debulking, however, Intra operatively she was found to have a grossly extensive and extremely friable tumor lying very close and encasing major abdominal vessels, the mass was pushing the mesentery and colon anteriorly. The upper part of the tumor was adherent to the retroperitoneal muscles. A debulking was therefore not possible, however core biopsies from two sites were taken and the sample was sent to histopathology for assessment.
The histology sections showed tissue sample in which malignant cells whose architecture was completely effaced and replaced by sheets of epithelioid cells with abundant clear cytoplasm and moderately pleomorphic nuclei. The tumor cells showed prominent nucleoli and were distributed around a dense network of blood vessels. The Cells showed scant mitotic activity and there was no necrosis. The tumor cells where Negative for inhibin, CD10, CEA, AE1,AE3, Vimentin, EMA , S100, CD45 and CD99 and positive for HMB45.The features were finally reported to be consistent with a perivascular epitheloid cell tumor (PEComa) (Figure 2a & 2b).
The clinical and Histology findings were discussed in multidisciplinary tumour board and a decision was made to attempt downsizing by giving chemotherapy, based on the lines of sarcoma. She was therefore started on Anthracycline based chemotherapy (Adriamycin, ifosfomide and methotrexate). She showed extremely poor tolerance to chemotherapy and the tumour size was seen to increase soon after the first cycle with worsening of symptoms. mToR inhibitors have shown good clinical activity and solid molecular basis to have efficacy in this rare tumor.3,4
She was subsequently therefore switched to mToR (mammalian target of Rapamycin) inhibitor Evrolimus.5 She showed a good clinical response with improvement in appetite, reduction in pain and requirement of analgesia, better performance status and feeling of general wellbeing. A repeat CT scan after 4 months of treatment revealed that the mass showed reduction in size and there were prominent necrotic appearing areas. The patient remained stable and responding for seven months after being put on mToR inhibitors. On one of the further follow ups she complained of breathlessness and exertional fatigue. She had clinical signs of pleural effusion, which was confirmed on chest radiograph. She was initially managed conservatively but she continued to show clinical worsening requiring a chest tube drainage followed by Pleruodesis. A repeat CT-scan (Figure 3) revealed gross progression of the primary tumor.
In view of extensive tumor progression, a poor performance status and failure to available lines of therapy, after thorough counseling of the patient herself and the family, active treatment was withdrawn and she was offered best supportive care. She subsequently succumbed to the disease three weeks later.
PEComas are mesenchymal neoplasms composed of morphologically and immunohistochemically distinct perivascular epitheloid cells. They belong to a family of related neoplasms that include Lymphagiomyomatosis, Angiomyolipoma, and Clear cell ‘sugar’ tumours of the lung. These tumors have previously been described as an “Abnormal myoblast”.1 The cells show focal association with blood vessels and express smooth muscle and melanocyte markers.6 These rare group of tumours have a female preponderance.7They have been described in multiple anatomical sites including the liver, mesentery, pancreas, uterus heart, Kidney and lung and prostate gland.8 Review of the of the literature suggests that the patient presented has had perhaps the largest size of PEComa reported so far and is easily to be confused with other rather common soft tissue sarcomas in this age group.9 The biological behaviour of these tumours has been described to vary significantly more variable has been the treatment response. Their clinical behaviour has been described to range from what would be close to benign to a very high grade sarcoma with relentless course in some instances.10 Folpe et al.11 have suggested criteria for malignancy and aggressiveness, including a size of >8.0cm, mitotic count of >1 per 50 high power fields (HPFs) and necrosis, with 3 categories namely benign, uncertain malignant potential and malignant based on the presence of none, 1 or ≥2 of these three criteria, respectively.11
PEComas are strongly associated with Angiomyolipoma and lymphangiomyomatosis, which are associated the tuberous sclerosis complex. There is sparse data on the cytogenetic and molecular genetics of sporadic PEComas, and the little data available is inconsistent. The evidence for the use of mTOR inhibitors stemmed from data showing increased markers of mTOC1 suggestive of loss of TSC1 or TSC2.12 Good therapeutic response to mTOR inhibitors has been reported by Gennatas et al.5 offers a reasonable rationale for the initiation of this therapy.5 Our Patient also demonstrated a reasonable degree of radiological response with mTOR inhibitor Evrolimus 10mg / day, our patient showed striking improvement in symptoms such as pain control, and improvement in appetite. The response was albeit short-lived, and lasted for only about seven months.
Optimal treatment for PEComa has not been established. Curative or debulking surgery appears to be the mainstay of treatment in the situations when the primary and metastasis are resectable. The role of neo/adjuvant therapy is not established and is reported with inconsistent responses.13,14 Large locally advanced or metastatic disease usually has a poor prognosis.
Early identification of a rare malignancy like PEComa is of utmost importance for appropriate management. These tumours can behave variably and sometimes very aggressively. Better molecular understanding would define effective medical treatment for this rare tumour, for which there are no current standards of care.
None.
The authors declare there is no conflict of interests.
None.

©2016 Shaikh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.