Journal of
eISSN: 2373-633X


Mini Review Volume 13 Issue 3
Department of Genetics, Nirnayan Healthcare Pvt Ltd, India
Correspondence: Ajanta Halder, Department of Genetics, Nirnayan Healthcare Pvt Ltd, Sukanta Pally, Kaikhali, Kolkata, West Bengal 700136, India, Tel +91-9830196735
Received: May 11, 2022 | Published: June 1, 2022
Citation: Banerjee B, Halder A. Lifestyle and environmental factors-a critical correlation of breast cancer. J Cancer Prev Curr Res. 2022;13(3):79-81. DOI: 10.15406/jcpcr.2022.13.00492
In India, most common form of cancer in women is breast cancer. Every year more than 1,00,000 new breast cancer patients are diagnosed in India. Though it is completely treatable if detected in early stage, the rate of cure in India is less due to lack of awareness, lack of access to health care facilities, ignorance of symptoms and socio-cultural attitudes. There are several environmental factors associated with BC. Research has shown that the risk factor of BC is higher to the women who work at night as light exposure at night suppresses the melatonin secretion and gives rise to cancer. Exposure to Xenoestrogen (present in plastic containers, pesticides etc.), Parabens (present in preservatives and cosmetics), alkylphenols, phytoestrogen are really harmful and can cause BC. Besides, consumption of excessive alcohol, obesity, use of Hormone Replacement Therapy and late onset of menopause are equally responsible for breast cancer.
Keywords: Breast Cancer, BPA, xenoestrogen, paraben, alkylophenol, melatonin, dichlorophenyltrichloroethane
Breast cancer is one of the most common cancers in women. Worldwide more than 1million new breast cancer patients are diagnosed annually.1 There are various factors that can cause breast cancer, like genetic factors, radiation, hormonal abnormalities, lifestyle disorder, hormone replacement therapies, environmental factors etc. Breast tissue formation starts before birth and continues to mature during puberty, pregnancy and menopause. Researchers found that there are various environmental factors like chemicals, diet, lifestyle etc. can alter gene expressions, which results the formation of carcinoma during the development stages of breast tissues. The scope of the review is focused upon the compilation of data of various researches and studies for breast cancer awareness.
Xenoestrogen
The word “Xeno” refers to “Foreign”, thus Xenoestrogen is foreign estrogen. It is also known as “Environmental Hormones” or Endocrine Disrupting Compound (EDC).2 It is one of the most hazardous chemicals that is responsible for Estrogen imbalance within the body, not because of its action because it is present almost everywhere or in everything that we use regularly. Previously it was thought that Xenoestrogen can only act through nuclear hormone receptor3 but studies found that it can also exert the action through neurotransmitter receptors. Researchers also demonstrated the alteration of acetyl cholinesterase.4 Xenoestrogen is also found to alter HOX gene expression.5 In an experiment6 found that if rodents are exposed to Bisphenol A, molecular changes in their breast tissues occur which also causes alteration of estrogen sensitivity, mammary ductal hyperplasia and finally carcinoma.6
Sources
Plastic is one of the major sources of Xenoestrogen. Bisphenol A (BPA) is a chemical plasticizer which has xenoestrogenic properties.2 BPA directly enters within our body though diet as it is used in plastic bottles, beverage boxes, lining of juice cans etc.
Another well-known source of Xenoestrogen is Pesticide. The most hazardous pesticide is DDT. Though it is banned in most of the countries but it can persist within the soil for centuries. Not only within the soil, it is present within the cereals, vegetables and even in water. In a study performed in Spain (1999-2009) it was found that 81% breast cancer patients belonged to high pesticide contaminated areas.7 The pesticides that enter our body through diet can be stored within the fat tissues, which are also found in the breast.
Only 1% pesticides fall on the pests in the fields and remaining affects the crops. It is found that nowadays almost all vegetables, fruits and even water is contaminated by Xenoestrogen.8
Some other chemicals that act as Xenoestrogen are shown in Table 1:2
Chemicals |
Uses |
Alkylophenol |
Used to manufacture many other chemicals |
Atrazine |
Commonly used weedicide |
Butylated hydroxyanisole (BHA) |
Used for preservation of foods |
Dieldrin |
Insecticide (banned in many countries) |
DEHP |
Used in PVC manufacturing |
Endosulphun |
Insecticide (banned in many countries, not banned in India yet) |
Heptachlor |
Insecticide (restricted, not in India) |
4-methylbenzydene camphor |
Used in Sunscreen lotions |
Pentachlorophenol |
Used as biocide and wood preservative |
Phenosulfothiazine |
Used to manufacture red dye |
Propyl gallate |
It is an antioxidant, used to prevent fats and oils from oxidation |
Phytoestrogen
Phytoestrogens are natural substances that are found in plan or plant derived foods.9 Phytogens have potential anticancerous activity but some are also responsible for estrogen imbalance in the body. The main three classes are isoflavones, coumestans and lignans.10 Among the three classes isoflavone has received huge concern due to its estrogenic potential. It is mainly found in Soy beans and flax seeds. Isoflavones bind to estrogen receptors, preferably to the estrogen beta receptor.11 They trigger only poor response and at the same time they block the binding of natural estrogens. There is structural similarity to the potent synthetic antiestrogen, Tamoxifen, a drug that is efficient in breast cancer treatment and prevention.12
The effect of phytoestrogens on breast cancer is still in debate. Some studies established that consumption of soy beans can cause decrease in serum 17-beta estradiol,13 decrease in plasma FSH and LH14 in premenopausal women. Although Martini et al. did not find any hormonal imbalance due to soy consumption in 36 premenopausal women (Figure 1).10

Figure 1 Xenoestrogen and Phytogen, when present in blood, bind to Estrogen receptorand causes unregulated cell division, which enhance the risk of breast cancer.
Light exposure
These days most of the women work in rotating shifts, which affects their circadian rhythm. Working and light exposure at night results reduced level of Melatonin, which is a darkness responsive hormone and results sleep deprivation. Melatonin is primarily secreted by pineal gland, other organs like skin,15 eyes,16 GI tract,17 lymphocytes,17 and bone marrow.18 Epidemiological studies have accounted associational testimony that night shift work and exposure to light at night are risk factors for breast cancer.19
Reduced melatonin levels and elevated estrogen secretion have been documented in nurses who developed breast cancer and who had long employment history of rotating night shifts.20 On the other hand, a reduced risk of breast cancer was reported in blind women. In a case control study, women with bilateral blindness had almost half the risk of breast cancer as compared to the control group (Figure 2).21
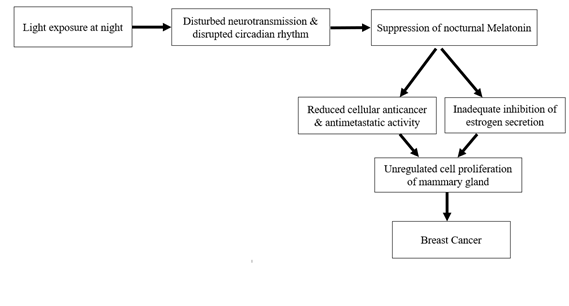
Figure 2 Prolonged light exposure during night can lead to suppression of Melatonin and increased estrogen secretion which increases the risk of Breast Cancer.
Cosmetics
In our day-to-day life we use various kinds of cosmetics, most of which contain hazardous chemicals like paraben, ethylene oxide, phthalates etc. Paraben is widely used as preservative in shampoo, soaps, antiperspirants, fragrances etc. It can be present in various compounds, like ethylparaben, methylparaben, n-butylparaben, isoparaben etc., all of these components are equally harmful. Janjua et al.,22 found that paraben can easily penetrate our skin and long term use of these products leads to accumulation of paraben within the body.
Experimental studies have established the mechanism of action of parabens and their effect on the occurrence of breast cancer. A number of studies have reported that parabens act mainly by an in-vivo mechanism mediated by the estrogen receptor.23 Parabens have been identified as weak estrogens because of their low-binding affinity to the estrogen receptor, but they can give the same magnitude of response on the growth of human breast cancer cells in-vitro as 17β-estradiol when adequate concentrations are present.24
Ethylene oxide is widely used in shampoo, fragrances, detergents, thickeners etc. It was one of the main ingredients in various cosmetics until International Agency for Research for Cancer (IARC) identified this as carcinogenic agent.25 Phthalates have potential estrogenic cell response. It is found in wide various products like cleaning products, nail polish, hair spray, soft plastic containers etc. Some studies found elevated level of phthalates within the urine sample of breast cancer patients.26 The major pathway of exposure to phthalates is the oral route, though inhalation and dermal absorption may play a significant role in exposure.27
Alcohol consumption
The practice of alcohol consumption, especially among women has increased with developing economy. A number of epidemiological studies suggested the correlation of alcohol consumption and breast cancer and the evidences show various mechanism of this association. Alcohol elevates hormone levels, particularly estrone sulfate and dehydroepiandrosterone (DHEAS), and this is one of the mechanisms of causing breast cancer.28 A study among 51 post-menopausal women suggests, women who were not on Hormone therapy, when consumed 15g and 30g alcohol per day for 8 weeks they had increased concentration of estrone sulfate (7.5% and 10.7% respectively). DHEAS level also increased by 5.1% and 7.5% respectively.29
Alcohol metabolism, predominantly occurs in liver, is known to cause tissue damage due to the production of acetaldehyde.30 Acetaldehyde is a toxic element which may lead to DNA modification resulting cancer. In addition, alcohol metabolism has significant role in formation of tumor and metastasis via increasing estrogen level.30
Hormone replacement therapy
Hormone replace therapy (HRT) relieves the symptoms of post menopause and also prevents osteoporosis. Though HRT is beneficial, it has been reported to cause breast cancer in various studies. In 1993, Zumoff31 did a detailed review where he mentioned 69 epidemiological reports concerned about the correlation of HRT and breast cancer. As per his report, 27 studies showed slight increase, 32 studies showed no differences, while 10 studies showed slight decrease in the risk of breast cancer. Women who have received prolonged hormone therapy have denser breast tissue32 and the tumor is hard to detect via mammography. Thus, they have poor prognosis. Though there are lots of data, there is also conflict regarding this hypothesis. Researchers are going on to find more association.33
Chemicals with various estrogenic activities are being used every day. It seems impossible to avoid their exposure and nowadays women need to work without calculating time and maintaining healthy lifestyle. Though, following some measures can go long way in ensuring protection like not using electronic devices during bed time, avoiding chemical-based cosmetics products, reducing the use of chemical pesticides in agricultural field, washing raw fruits and vegetables to reduce the amount of pesticides, switching to organic food, reducing the use of plastic container, specially while heating the food in microwave, avoiding nonstick and Teflon cookware, minimizing the consumption of food from tin can, ventilating the house frequently etc. The study also suggests reduced alcohol consumption and avoiding HRT can also lower the risk of breast cancer. Moreover, a healthy lifestyle with balance diet, a healthy mental state, physical activities are more effective to abate the risk of breast cancer. However, further studies are needed to explore the effects better.
I am grateful to Nirnayan Healthcare for providing required infrastructure and academic resource for this study.

©2022 Banerjee, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.