Journal of
eISSN: 2373-633X


Research Article Volume 4 Issue 1
1BS Abdur Rahman University, India
2AU-KBC Research Centre, Anna University, India
3Purdue University, USA
Correspondence: Raji Sundararajan, Purdue University, 401, N Grant St, West Lafayette, IN 47907, USA
Received: November 26, 2015 | Published: January 18, 2016
Citation: Pachamuthu S, Jothi V, Ramachandran RP, et al. Influence of electrodes on electric field distribution for effective electrochemotherapy. J Cancer Prev Curr Res. 2016;4(1):21-25. DOI: 10.15406/jcpcr.2016.04.00107
Electroporation is the application of electrical pulses for enhanced drug delivery. When used for delivering chemo drugs, it is called electrochemotherapy (ECT). For inoperable and chemo- and radio-resistant tumors, we need an alternative technique and ECT is a viable option as evidenced by the treatment of thousands of patients, effectively. The efficiency of the ECT depends on the voltage (electric field) magnitude, pulse duration, number of pulses, the drug molecule to be delivered and the electrode geometry and size. It is of practical interest to study the effect of electrode material on the efficacy of the therapy. Towards this, in this research, we investigated the influence of electric field distribution due to different electrode materials. For this purpose, both platinum and surgical steel needle array electrodes were used. Surgical steel is the most commonly used material for electro chemotherapy applications. These needle electrodes are of both hexagonal and pentagonal configurations with a central electrode in each. ANSYS, the industry standard software that uses finite element method is used to study the electric field distribution, of both healthy tissue and tumor tissue using these two electrode configurations and the two different materials. Both unipolar and bipolar voltages were studied. The results indicate that the electric field distribution, both in magnitude and pattern is similar for both electrodes, for both configurations and materials, which is desired from the clinical aspect. The electric field intensities for the hexagonal and pentagonal needle electrodes were 1280V/cm and 1180V/cm respectively in the case of tumor tissue (correlating well with the desired level of 1200V/cm). They were 835V/cm and 843V/cm for these electrodes in the case of healthy tissues. The values were same in the case of bipotential voltages too.
Electrochemotherapy (ECT) is an evolving technique to treat various types of skin, chest wall breast cancer and basal cell carcinoma with minimal side effects.1 Electrochemotherapy was the only available alternative treatment for patients suffering from lung cancer who are unfit to undergo surgery.2 This procedure utilizes hydrophilic chemo drugs such as bleomycin and cisplatin which are aided by electroporation to create apoptosis. ECT has an overall response of 80-90% for un-resectable recurrent disease.3,4 Typically eight 1200V/cm, 100µs pulses are applied in the clinics. The various parameters which influence the process of electroporation are electric potential (field intensity), pulse width, number of pulses, types of chemo drug, and size and geometry of the tumor.5–7 In addition, the efficiency of electroporation also depends on the type, size and shape of electrodes. In practice, based on the method of contact, electrodes are classified as surface electrode, needle electrode and flexible laparoscopic electrode.8 Based on the geometry, the electrodes are classified as linear array and concentric electrodes. The electrodes play a vital role of connecting the tissue to the electrical pulses. Needle electrodes have better efficiency over surface electrodes for treating deep-seated tumors.7 But the surface electrodes provide uniform distribution over needle electrodes, since the point of contact for surface electrode is wider than needle electrode. Within needle electrodes, concentric type of electrodes provides better uniform distribution of electric field over linear array electrodes.9 For effective electroporation and to maximize its outcome in the tumor, design and positioning of the electrodes with respect to the tumor becomes a critical factor. Hence, the design of electrodes varies for each case. Electrode design using numerical methods enables the optimized design of electrodes for effective electroporation. Numerical modeling determines optimal parameters even for inhomogeneous tissues which could not be achieved through analytical calculation.9 The focus of this work is to determine the effect of material used as electrode apart from its configuration in electroporation. For this purpose, needle electrodes of both surgical steel and platinum were studied for both hexagonal and pentagonal configurations. Surgical steel is the material commonly used in the manufacturing of electrodes. Due to its distinct electrochemical properties, nobility and metallic characteristics; it is used in various medical applications from cranial joints to syringes.10–12 On the other hand, platinum can also be used as electrode material for its electro-chemical attributes, noble metal (inert) properties and physical properties. However, platinum usage results in the deposition of salts, viz., platinum (IV) chloride, hexachloroplatinate (IV) ammonium, hexahydroxyplatinate (IV) potassium, diaminedinitroplatinum (II), etc.13,14 These salts are reported to cause various side effects. Platinum salts can also induce bronchoconstriction, anaphylactic shock, elevated plasma histamine levels etc. even without any prior exposure.15 In addition, platinum is costly. It is of practical interest to study using simulation, the electric field distribution of these two materials.
In this study, two configurations of concentric type needle electrodes are analyzed. Honey comb structured hexagonal array concentric type needle electrode and pentagonal type needle electrode with central anode are analyzed due to the uniform distribution of electric field by these configurations.9,16,17 The above configurations have also been built and simulated for their electric field distribution. Figure 1 shows the two electrode geometries with central electrode, designed and built. Figure 1A shows the hexagonal electrode array and Figure 1B shows the pentagonal electrode array. These electrodes are modeled and simulated using industry standard software, ANSYS APDL version13.0, 2010, which uses finite element method to do the electric field computation. The electrode configuration with tumor, surrounded by healthy tissue and without tumor are modeled in ANSYS such that the distance between each electrode (d) is very much greater than the diameter (a) of the electrode (d>>a). In ANSYS, the various available types of simulation techniques available are electric, thermo-electric, fluid dynamics, structural, and so on. Electric was used in this research. Then the element property to be applied for the model has to be selected. In this study, 2D quad structure is selected. ANSYS needs the electrical properties, resistivity and relative permittivity of the various materials in the study, including the healthy tissue, the tumor tissue, and the electrode materials. The resistivity of the tumor is considered as 2.5Ω-m and permittivity as 52F/m. For healthy tissue, the resistivity is considered as 5 Ω-m and permittivity as 52F/m.17,18 The electrical properties of electrodes (both platinum and surgical steel) are provided in the Table 1.5,17

Figure 1 Electrode geometries of Hexagonal (A) and Pentagonal electrodes, both with central positive electrode.
S. no |
Material description |
Resistivity, Ω-m |
Relative permittivity |
1 |
Platinum electrode |
105x10-9 |
1 |
2 |
Surgical steel electrode |
740x10-9 |
14 |
3 |
Healthy tissue |
5 |
52 |
4 |
Tumor tissue |
2.5 |
52 |
Table 1 Electrical properties of materials studied
In addition, the geometry and dimensions of all these materials is also needed. The radius of each electrode was chosen as 0.5mm. The tumor size is 2.5mm. Table 2 gives the various geometry details. For study purpose, the distance between adjacent electrode of same potential (d) and the distance between electrodes of opposing potential (l) are considered to be equal (0.4cm). The electric field applied in the study is a single pulse of 1200V/cm with a pulse width of 100µs. Contour plot is preferred over other output methods since it can provide the uniformity of electric field distribution as well as region of effective electroporation graphically. Both unipolar and bipolar potentials were studied. In the case of unipolar, the central electrode was set at positive voltage (of V=+480V, to get a electric field of, E=V/d = 480/0.4=1200V/cm, for an electrode gap of 0.4cm). The outer electrodes were set to ground voltage (0V). For bipotential, the central electrode was set at +240V and the outer electrodes at -240V, so the total voltage is 480V (240-(-240) =480V). Figure 2 shows the models used for electric field simulation study. Figure 2A shows the central anode configuration of concentric type hexagonal array electrode, and Figure 2B shows the central anode configuration of concentric type pentagonal array electrode.
S. no |
Description |
Dimension |
1 |
Radius of each electrode |
0.05 cm |
2 |
Healthy tissue |
3 cm X 3cm |
3 |
Radius of the tumor |
0.25cm |
4 |
Distance between each pair of electrode (l) |
0.4cm |
5 |
Distance between cathode and anode (d) |
0.4cm |
Table 2 Dimensions of model components
The 2D contour plots of electric field distribution of platinum electrodes without tumor is shown below in Figure 3 and that of with tumor (surrounded by the healthy tissue) is shown in Figure 4. Figure 3A shows the electric field distribution in the healthy tissue without tumor, when a hexagonal concentric array with central positive electrode is used to apply pulses in the healthy tissue, and Figure 3B, with a pentagonal electrode. It is seen that the electric field did not spread beyond the ground potential electrodes surrounding the anode, in both cases. Thus these configurations provide good coverage and precision in locally targeting the required area. Figures 4A & 4B show the electric field distribution with the tumor. The tumor is considered as a homogeneous structure of circle for easy representation. In practice, the shape of the tumor will be inhomogeneous structure. Here, the maximum electric field is around the positive electrode, which in turn is placed exactly on the tumor. Thus the maximum electric field is rather on the tumor than on the healthy tissue. The electric field distribution of surgical steel electrodes with tumor for these configurations is shown in Figure 5. This matches exactly with the electric field distribution shown in Figure 4, for platinum electrodes. Tables 3 & 4 show a comparison of the max and average electric field intensities for the two electrode configurations and the two materials. There is close correlation between the values at both the healthy tissue and tumor area, indicating that the material does not affect the electric field value, which is good for treating the tumor with various electrode materials. Of course, it is possible that the reaction of the tissue and the drug molecules could be different in the clinical practice. However, as for as the electrochemotherapy is concerned, only the configuration of the electrode geometry matters, not the material.
A comparison of our results with the published results in the literature9 indicates close correlation in the pattern and magnitude of the electric field. Figure 6 shows results obtained by Corovic et al.9 for hexagonal electrode. There is very good similarity in the electric field distribution. There is good correlation of the magnitudes also at various distances (905.4, 928.7, 925.4, 876.9, 875.9V/cm, and so on). The magnitudes vary from 4% to 10% between our and these published values, indicating good correlation between our findings. One-on-one correlation is not possible as the data points are not furnished. Figure 7 & Figure 8 illustrate the comparisons of electric field intensities at various points/distances for hexagonal and pentagonal electrode configurations, respectively, for both platinum and surgical steel electrodes, with and without tumor. They compare the max value of the electric field from center of the tumor to the cathode. Table 5 shows the variation of the max electric field, assuming the value at 0 to be 100%. It reduces at locations 1, 2, and 3 and then increases. The variation is similar for both healthy and tumor tissues and also for both materials for the two electrode geometries. The variation is maximum at the interface of the electrode to tissue due to the noticeable difference in the resistivity and relative permittivity of the two materials. It tapers down in between and then again increases due to the significant difference between the material properties between the tissues and the electrode.

Figure 6 Electric field distribution of hexagonal electrode.9
In addition to unipolar potential, the electric field distribution using bipolar potential was also studied. For this purpose, the central electrode was kept at +240V and the outer electrodes at -240V, compared to +480V and 0V respectively, in the unipolar case. Figure 9 & Figure 10 show the electric field distributions of hexagonal and pentagonal platinum electrodes with bipolar potential for healthy and tumor tissues respectively. These bipotential distributions correlate very well with those using central positive electrode (and other electrodes at ground potential (0V). The average electric field magnitudes were 1230 and 1180V/cm respectively for hexagonal and pentagonal electrodes for both platinum and surgical steel electrodes. They match very well with the unipolar values of 1230 and 1180V/cm (Table 3). There is also good match for the maximum values of 2950V/cm for hexagonal and 2850V/cm for pentagonal electrodes. The results are same for surgical steel electrodes (data not shown).
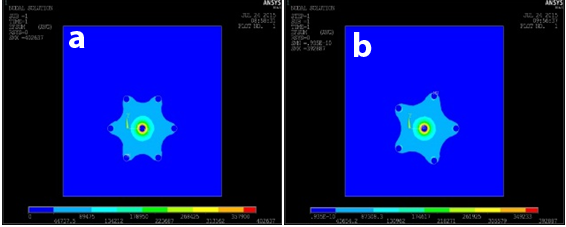
Figure 9 Electric field distribution using bipolar potential for healthy tissue using hexagonal (A) and pentagonal (B) Needle electrodes.
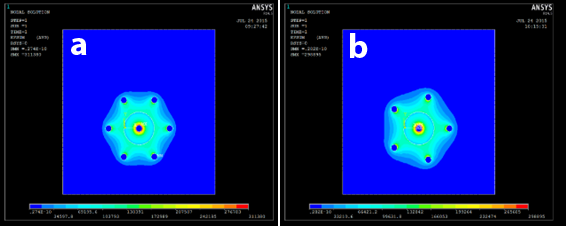
Figure 10 Electric field distribution using bipolar potential for tumor tissue using hexagonal (A) and pentagonal (B) Needle electrodes.
Electrode geometry |
At the healthy tissue |
At the tumor tissue |
||
Platinum |
Stainless steel |
Platinum |
Stainless steel |
|
Hexagonal |
835 |
835 |
1230 |
1230 |
Pentagonal |
843 |
843 |
1180 |
1180 |
Table 3 Average electric field intensity for hexagonal and pentagonal electrodes
Electrode geometry |
At the Healthy Tissue |
At the Tumor Tissue |
||
Platinum |
Stainless Steel |
Platinum |
Stainless Steel |
|
Hexagonal |
3780 |
3780 |
2950 |
2950 |
Pentagonal |
3640 |
3640 |
2830 |
2830 |
Table 4 Maximum electric field intensity for hexagonal and pentagonal electrodes
Location |
Hexagonal electrode |
Pentagonal electrode |
||
|
Healthy tissue% |
Tumor tissue% |
Healthy tissue% |
Tumor tissue% |
0 |
100.00 |
100.00 |
100.00 |
100.00 |
1 |
37.70 |
34.90 |
37.30 |
35.12 |
2 |
21.90 |
21.30 |
23.10 |
21.94 |
3 |
17.62 |
35.25 |
18.75 |
36.75 |
4 |
31.13 |
60.67 |
34.95 |
38.50 |
Table 5 Variation of mam magnetic field along the distance between the electrodes
We gratefully thank Mr. Abdul-Qadir AR Buhari, Chairman, Dr. VM Periasamy, Vice Chancellor and Dr. V. Murugesan, Registrar of BS Abdur Rahman University, Chennai, India for their support and funding to accomplish this work.
The authors declare that there is no conflict of interest.

©2016 Pachamuthu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.