Journal of
eISSN: 2373-633X


Research Article Volume 15 Issue 5
1DDS, PhD student, Clinical Research Division, Instituto Nacional de Câncer, Brazil
2DDS, Dentistry section, Instituto Nacional de Câncer, Brazil
3PhD, Clinical Research Division, Instituto Nacional de Câncer, Brazil
Correspondence: Lísia Daltro Borges Alves, DDS, PhD student, Clinical Research Division, Instituto Nacional de Câncer, Rio de Janeiro, Brazil
Received: October 09, 2024 | Published: October 24, 2024
Citation: Alves LDB, Menezes ACS, Lage LFS, et al. Epidemiological profile of oral and maxillofacial prosthesis rehabilitated patients in the Brazilian National Cancer Institute: a cross-sectional study.J Cancer Prev Curr Res. 2024;15(5):109-116. DOI: 10.15406/jcpcr.2024.15.00561
Introduction: Maxillofacial prostheses represent a rehabilitative option for patients who underwent head and neck tumor resection.
Objective: To describe the epidemiological profile of maxillofacial prostheses rehabilitated patients in an oncology reference center, from 2015 to 2020.
Materials and methods: This is a retrospective, descriptive, observational study, based on secondary data. The maxillofacial prostheses were identified through the prosthesis laboratory records. The socio-demographic, clinical, and maxillofacial prosthesis data were collected from medical records and were descriptively analyzed according to the prosthesis types.
Results: A total of 202 patients and 282 maxillofacial prostheses were identified. Obturator prostheses (37%) were the most frequent, and 2019 was the year with the largest production (54%). Males (55%), with 45 years, and incomplete primary education (32%) prevailed. Most tumors were carcinomas (43%), in the palate (40%), with 15.5 months of evolution, at stage III (25%) Surgery and surgery associated with radiotherapy were the most commonly used therapeutic modalities (40% each). At the last visit, most patients had complete remission of the disease (67%). Maxillofacial prostheses were mostly in acrylic resin (92%), with 9.5 months of use, and hygiene was considered satisfactory (87%). Most patients reported good adaptation (82%), satisfaction (76%), satisfactory hygiene (87%), and no adverse events (83%) or difficulties (69%) associated with its use.
Conclusion: These data highlight the importance of oral and maxillofacial prostheses as an effective and accessible tool in the rehabilitation process and reinforce the need for a multidisciplinary team to work in oncology, with the dentist as an essential player in this context.
Keywords: maxillofacial prosthesis, patient care team, integrative oncology, cancer care facilities, rehabilitation.
In Brazil, cancer is a public health issue and one of the main causes of death. Its prevention and early diagnosis directly impact the success of treatment and a favorable prognosis for the patient.1 Considering the different oncological therapeutic modalities, surgery is usually the treatment of choice for most solid tumors; however, when performed in head and neck patients, it can imply major mutilations. These resections can be partial or total, involving one or both sides of the face, and include the maxilla, mandible, orbit floor, eyeball, nasal cavity, and auricular cavity, among other structures.2 In this sense, surgical or prosthetic rehabilitation are essential pillars in the patient's readaptation process,3–6 Being an extremely complex process, that should preferably involve a multidisciplinary team.4,7,8 In cases where surgical rehabilitation is not viable, the reconstruction of lost structures in the maxillofacial region can be achieved by maxillofacial prostheses (MFP), a highly relevant instrument.2–8 Its prime objective is to restore aesthetics and protect the damaged area, a crucial aspect in the patient's self-esteem reestablishment.4,7–10 These prostheses must be manufactured after the healing of the surgical area and can be for intraoral or extraoral use.2 Regarding intraoral prostheses, surgical plates, obturator prostheses, and modified lower prostheses stand out. The first two are used in those patients with loss of the maxillary complex structure and, consequently, buccosinusal communication, with the first being installed during the surgical time and the second, in a later period.11,12 The modified lower ones are those used by the mandible, tongue, and floor-of-the-mouth surgical patients, in which adaptations vary according to the new anatomy of the region after treatment.13 The extraoral prostheses are named after the rehabilitated region: ocular, oculo-palpebral, facial, nasal, or auricular.6
Guarded each MFP type proprieties, they are responsible for reducing the need for nasoenteral probe reinsertion, minimizing functional limitations (chewing, swallowing, phonation, breathing, and sucking), disability, depression, infection processes and contribute to the patient's familiar and social environment reintegration by restoring aesthetics, self-esteem, and related psychological factors.2,6,14,15 It is a complex procedure, involving a multidisciplinary team4,7,8 including the dentist. Currently, there are few MFP-specialized professionals, and consequently, scarce production and data regarding these prostheses. Thus, this study aimed to describe the epidemiological profile of MFP rehabilitated individuals in the Dentistry section of a Brazilian oncology reference center, from August 2015 to August 2020; as well as analyze the related characteristics to the manufacturing materials and the use of MFP.
This is a retrospective, descriptive observational study based on secondary data from physical and electronic records. The present study was approved by the responsible Ethics Committee for Research on Human Beings (nº 4.307.161, CAAE: 38012120.5.0000.5274). Individuals with histopathological diagnoses of benign or malignant tumors treated and rehabilitated with oral and maxillofacial prostheses in the Dentistry section of Instituto Nacional de Câncer (INCA), Rio de Janeiro, from August 2015 to August 2020 were included. Were considered as MFP auricular, facial, nasal, obturator, ocular, oculo-palpebraloculo-palpebraloculo-palpebraloculo-palpebral, or modified lower prostheses, and surgical plates. Individuals who started but did not complete the confection of MFP were not included in this study. Initially, the prosthesis laboratory records were reviewed, and the number of rehabilitated individuals, MFP per individual, type of MFP, and year of manufacture were identified. Based on this data, physical and electronic medical records were evaluated, and the data of interest were collected in a specific and standardized form.
The analysis of medical records collected the following data on sociodemographic variables: gender, age at diagnosis, schooling, and family history of neoplasms; regarding clinical variables, the collected variables were location, time of evolution to the date of diagnosis, clinical staging, histological type, treatment of choice and survival status at the last visit at the institution. Regarding the MFP, the data collected referred to the material, time of use, adaptation and patient satisfaction, hygiene situation, adverse events associated with the use, and difficulties reported during the use. The collected data were tabulated and descriptively analyzed using the SPSS statistical program (Statistical Package for the Social Sciences), version 17.0. Analyzes were performed according to the MFP types. For the sociodemographic and clinical variables, when more than one MFP was made for the same patient, only one record was considered; for patients with more than 1 different MFP type, 1 record was considered for each type of MFP. For MFP characteristics analysis, all registers were considered, regardless of the amount of MFP per patient. The results referring to the qualitative variables were described through tables of frequencies, with their respective percentages; for the quantitative variables, descriptive measures were adopted, such as mean and standard deviation.
The present study identified 202 MFP rehabilitated patients in this period. For 65 of them, more than one MFP was confectioned and so, for sociodemographic and clinical variables analysis, 235 records were considered; for the MFP variables, 282 were considered, as described in Supplementary (Table 1). The most manufactured MFP was the obturators (37%), followed by ocular (32%). There was no register of ear prostheses confection (0%). Regarding the period, 2019 was the year with the highest confection of most MFP types, except for the facial, with the highest frequency in 2020 (67%), and the modified lower prostheses, with the same frequency in 2017 and 2019 (50% in each year) (Table 1). Figure 1 illustrates some of the MFP made in the Dentistry section of Instituto Nacional de Câncer.
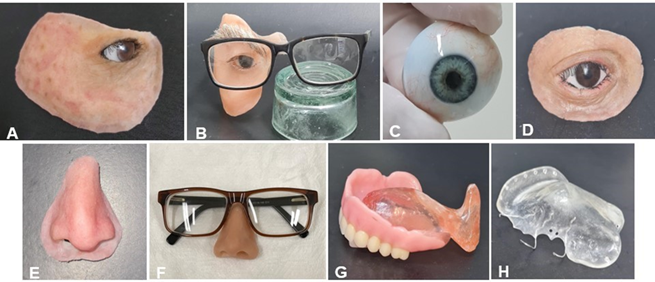
Figure 1 INCA dentistry sector MFPs, from august 2015 to august 2020. A- Silicone facial prosthesis, B- Acrylic resin facial prosthesis, fixed to glasses, C- Eye prosthesis, D- Oculo-palpebral prosthesis, E- Silicone nasal prosthesis, F- Acrylic resin nasal prosthesis, fixed to glasses, G- Obturator prosthesis, E- Surgical plate.
|
Variable |
MFP type |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Facial |
Nasal |
Obturator |
Ocular |
Oculo-palpebral |
Surgical plate |
Modified lower |
Total |
||||||||
|
Year (n= 282) |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
2015 |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
2016 |
0 |
0% |
1 |
9% |
12 |
12% |
3 |
3% |
0 |
0% |
3 |
6% |
0 |
0% |
19 |
7% |
|
2017 |
1 |
11% |
1 |
9% |
6 |
6% |
5 |
6% |
0 |
0% |
4 |
8% |
1 |
50% |
18 |
6% |
|
2018 |
0 |
0% |
2 |
18% |
12 |
12% |
11 |
12% |
1 |
6% |
13 |
27% |
0 |
0% |
39 |
14% |
|
2019 |
2 |
22% |
6 |
55% |
55 |
53% |
50 |
56% |
12 |
67% |
26 |
53% |
1 |
50% |
152 |
54% |
|
2020 |
6 |
67% |
1 |
9% |
18 |
17% |
20 |
22% |
5 |
28% |
3 |
6% |
0 |
0% |
53 |
19% |
|
Total |
9 |
100% |
11 |
100% |
104 |
100% |
89 |
100% |
18 |
100% |
49 |
100% |
2 |
100% |
282 |
100% |
Table 1 MFP confection by type and year, in the dentistry section of a Brazilian oncology reference center, from august 2015 to august 2020 (n=282)
Male patients prevailed in rehabilitation with facial (57%), obturator (52%), ocular (58%), oculo-palpebraloculo-palpebraloculo-palpebraloculo-palpebral (67%), and modified lower (100%) prostheses. Except for the ocular ones, all prosthesis types were for individuals diagnosed over 45 years. Incomplete elementary school was most frequent for nasal prostheses (43%), obturators (39%), and surgical plates (41%). Incomplete elementary, incomplete high school, and complete elementary levels were more frequent in facial, oculo-palpebral, and modified lower prostheses; (33%, 31%, and 50%), respectively. The ocular ones showed a prevalence of illiterate individuals (60%) (Table 2).
|
Variable |
MFP type |
Total |
||||||||||||||
|
Facial |
Nasal |
Obturator |
Ocular |
Oculo-palpebral |
Surgical plate |
Modified lower |
||||||||||
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
Sex (n=235) |
||||||||||||||||
|
Female |
3 |
43% |
4 |
50% |
41 |
48% |
30 |
42% |
5 |
33% |
23 |
51% |
0 |
0% |
106 |
45% |
|
Male |
4 |
57% |
4 |
50% |
45 |
52% |
42 |
58% |
10 |
67% |
22 |
49% |
2 |
100% |
129 |
55% |
|
Age at diagnosis (n=234)a |
||||||||||||||||
|
Mean (standard deviation) |
46.0 (±14.3) |
67.0 (±17.9) |
52.9 (±17.7) |
25.5 (±28.0) |
49,4 (±21.7) |
50.0 (±14.9) |
62.0 (±4.2) |
45.0 (±25.1) |
||||||||
|
0-10 years |
0 |
0% |
0 |
0% |
2 |
2% |
39 |
55% |
1 |
7% |
0 |
0% |
0 |
0% |
42 |
18% |
|
11-20 years |
0 |
0% |
0 |
0% |
5 |
6% |
1 |
1% |
1 |
7% |
1 |
2% |
0 |
0% |
8 |
3% |
|
21-30 years |
2 |
29% |
1 |
13% |
5 |
6% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
9 |
4% |
|
31-40 years |
0 |
0% |
0 |
0% |
5 |
6% |
4 |
6% |
2 |
13% |
3 |
7% |
0 |
0% |
14 |
6% |
|
41-50 years |
1 |
14% |
0 |
0% |
13 |
15% |
7 |
10% |
4 |
27% |
6 |
13% |
0 |
0% |
31 |
13% |
|
51-60 years |
4 |
57% |
0 |
0% |
22 |
26% |
11 |
15% |
1 |
7% |
10 |
22% |
1 |
50% |
49 |
21% |
|
61-70 years |
0 |
0% |
3 |
38% |
24 |
28% |
8 |
11% |
4 |
27% |
14 |
31% |
1 |
50% |
54 |
23% |
|
71-80 years |
0 |
0% |
3 |
38% |
8 |
9% |
1 |
1% |
1 |
7% |
8 |
18% |
0 |
0% |
21 |
9% |
|
81-90 years |
0 |
0% |
1 |
13% |
2 |
2% |
0 |
0% |
1 |
7% |
2 |
4% |
0 |
0% |
6 |
3% |
|
Schooling (n=207)b |
||||||||||||||||
|
Illiterate |
0 |
0% |
1 |
14% |
6 |
8% |
40 |
60% |
0 |
0% |
2 |
5% |
0 |
0% |
49 |
24% |
|
Complete elementary |
1 |
17% |
2 |
29% |
13 |
17% |
5 |
7% |
4 |
31% |
7 |
19% |
1 |
50% |
33 |
16% |
|
Incomplete elementary |
2 |
33% |
3 |
43% |
29 |
39% |
13 |
19% |
4 |
31% |
15 |
41% |
1 |
50% |
67 |
32% |
|
Complete high school |
1 |
17% |
0 |
0% |
14 |
19% |
6 |
9% |
3 |
23% |
7 |
19% |
0 |
0% |
31 |
15% |
|
Incomplete high school |
2 |
33% |
0 |
0% |
6 |
8% |
1 |
1% |
1 |
8% |
0 |
0% |
0 |
0% |
10 |
5% |
|
Complete higher education |
0 |
0% |
1 |
14% |
6 |
8% |
2 |
3% |
1 |
8% |
6 |
16% |
0 |
0% |
16 |
8% |
|
Incomplete higher education |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Family history of neoplasm (n=216)c |
||||||||||||||||
|
Absent |
5 |
83% |
2 |
40% |
47 |
59% |
38 |
56% |
10 |
67% |
20 |
49% |
1 |
100% |
123 |
57% |
|
Present |
1 |
17% |
3 |
60% |
33 |
41% |
30 |
44% |
5 |
33% |
21 |
51% |
0 |
0% |
93 |
43% |
Table 2 MFP rehabilitated individuals' socio demographic characteristics in the dentistry section of a Brazilian oncology reference center, from august 2015 to august 2020 (n= 235)
a= 1 missing data; b= 28 missing data; c= 19 missing data.
Regarding location, the tumoral location was compatible with the MFP type. At diagnostics, tumors had an average of 15.5 months of evolution; facial, oculo-palpebral, and nasal prostheses users had 30 months or more of tumoral evolution before diagnosis. Except for ocular prostheses, with retinoblastoma as the most common histological type (53%), all other MFP types were more frequent in carcinoma rehabilitation. Considering clinical staging, most facial, obturator, ocular prostheses, and surgical plates were for advanced-stage tumors (III and IV), 75%, 64%, 60%, and 64% respectively. Except for modified ocular prostheses and lower modified dentures, the treatment was usually combined therapy, with surgery associated with radiotherapy as the most frequent combination. Regarding survival status, obturator, ocular, oculo-palpebral, surgical, and modified lower prostheses rehabilitated individuals had complete remission at the last consultation, 68%, 83%, 77%, 50%, and 100%, respectively (Table 3).
|
Variable |
MFP type |
Total |
||||||||||||||
|
Facial |
Nasal |
Obturator |
Ocular |
Oculo-palpebral |
Surgical plate |
Modified lower |
||||||||||
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
Tumor location (n=235) |
||||||||||||||||
|
Mouth floor |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
50% |
1 |
0% |
|
Side of the tongue |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
50% |
1 |
0% |
|
Nasal cavity |
0 |
0% |
0 |
0% |
4 |
5% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
4 |
2% |
|
Nasal fossa |
1 |
14% |
1 |
13% |
2 |
2% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
5 |
2% |
|
Eyeball |
0 |
0% |
0 |
0% |
0 |
0% |
70 |
97% |
12 |
80% |
0 |
0% |
0 |
0% |
82 |
35% |
|
Eyeball and eyelid |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
7% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Upper lip |
1 |
14% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
1% |
|
Mandible |
1 |
14% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Nose |
0 |
0% |
7 |
88% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
8 |
3% |
|
Palate |
0 |
0% |
0 |
0% |
61 |
71% |
0 |
0% |
0 |
0% |
34 |
76% |
0 |
0% |
95 |
40% |
|
Eyelid |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
2 |
13% |
0 |
0% |
0 |
0% |
3 |
1% |
|
Parotid |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Upper ridge |
0 |
0% |
0 |
0% |
12 |
14% |
0 |
0% |
0 |
0% |
7 |
16% |
0 |
0% |
19 |
8% |
|
Maxillary sinus |
2 |
29% |
0 |
0% |
3 |
3% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
6 |
3% |
|
Sinuses |
2 |
29% |
0 |
0% |
2 |
2% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
4 |
2% |
|
Retromolar trigone |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
2 |
1% |
|
Tumor’s evolution time until diagnostic (n=206)a |
||||||||||||||||
|
Mean (standard deviation) |
34.5 (±57.1) |
30.0 (±22.7) |
17.9 (±23.8) |
10.7 (±19.0) |
32.0 (±36.3) |
14.3 (±17.7) |
10.0 (±0.0) |
15.5 (±23.7) |
||||||||
|
Tumor’s histological type (n=235) |
||||||||||||||||
|
Adenocarcinoma* |
1 |
14% |
0 |
0% |
16 |
19% |
0 |
0% |
0 |
0% |
7 |
16% |
0 |
0% |
24 |
10% |
|
Coronal adenoma |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Pleomorphic adenoma |
0 |
0% |
0 |
0% |
2 |
2% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
3 |
1% |
|
Ameloblastoma |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
1 |
0% |
|
Cystic adenoid carcinoma |
0 |
0% |
0 |
0% |
11 |
13% |
0 |
0% |
1 |
7% |
5 |
11% |
0 |
0% |
17 |
7% |
|
Carcinoma** |
5 |
71% |
8 |
100% |
47 |
55% |
3 |
4% |
8 |
53% |
29 |
64% |
2 |
100% |
102 |
43% |
|
Peripheral giant cell granuloma |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Hemangioma |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
3% |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
1% |
|
Lymphangioma |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Lymphoma |
0 |
0% |
0 |
0% |
4 |
5% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
4 |
2% |
|
Liposarcoma |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
7% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Melanocytoma |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Melanoma |
0 |
0% |
0 |
0% |
0 |
0% |
25 |
35% |
2 |
13% |
0 |
0% |
0 |
0% |
27 |
11% |
|
Nasoangio fibroma |
0 |
0% |
0 |
0% |
2 |
2% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
1% |
|
Conjunctival intraepithelial neoplasia |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
7% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Neurofibroma |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Chondroblastic osteosarcoma |
1 |
14% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
3 |
1% |
|
Retinoblastoma |
0 |
0% |
0 |
0% |
0 |
0% |
38 |
53% |
1 |
7% |
0 |
0% |
0 |
0% |
39 |
17% |
|
Synoviossarcoma |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
2 |
1% |
|
Solitary fibrotic tumor |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
7% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Primitive neuroectodermal tumor (PNET) |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Clinical staging (n=102)b |
||||||||||||||||
|
I |
1 |
25% |
1 |
25% |
6 |
12% |
1 |
20% |
0 |
0% |
6 |
18% |
0 |
0% |
15 |
15% |
|
II |
0 |
0% |
1 |
25% |
12 |
24% |
1 |
20% |
3 |
60% |
5 |
15% |
1 |
100% |
23 |
23% |
|
IIA |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
3% |
0 |
0% |
1 |
1% |
|
III |
1 |
25% |
1 |
25% |
12 |
24% |
1 |
20% |
2 |
40% |
9 |
27% |
0 |
0% |
26 |
25% |
|
IIIB |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
20% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
|
IV |
2 |
50% |
1 |
25% |
20 |
40% |
1 |
2% |
0 |
0% |
12 |
36% |
0 |
0% |
36 |
35% |
|
Treatment (n=235) |
||||||||||||||||
|
Surgery |
1 |
14% |
2 |
25% |
26 |
30% |
42 |
58% |
5 |
33% |
18 |
40% |
1 |
50% |
95 |
40% |
|
Surgery + Embolization |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Surgery + Chemotherapy |
0 |
0% |
0 |
0% |
0 |
0% |
16 |
22% |
1 |
7% |
0 |
0% |
0 |
0% |
17 |
7% |
|
Surgery + Chemotherapy + Radiotherapy |
0 |
0% |
0 |
0% |
5 |
6% |
5 |
7% |
0 |
0% |
5 |
11% |
0 |
0% |
15 |
6% |
|
Surgery + Radiotherapy |
6 |
86% |
6 |
75% |
45 |
52% |
9 |
13% |
9 |
60% |
19 |
42% |
1 |
50% |
95 |
40% |
|
Chemotherapy |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Chemotherapy + Radiotherapy |
0 |
0% |
0 |
0% |
6 |
7% |
0 |
0% |
0 |
0% |
2 |
4% |
0 |
0% |
8 |
3% |
|
Radiotherapy |
0 |
0% |
0 |
0% |
2 |
2% |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
3 |
1% |
|
Survival status (n=209)c |
||||||||||||||||
|
Complete remission |
0 |
0% |
1 |
20% |
54 |
68% |
52 |
83% |
10 |
77% |
21 |
50% |
2 |
100% |
140 |
67% |
|
Partial remission |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Stable disease |
2 |
40% |
0 |
0% |
5 |
6% |
7 |
11% |
0 |
0% |
1 |
2% |
0 |
0% |
15 |
7% |
|
Disease in progression |
2 |
40% |
4 |
80% |
5 |
6% |
1 |
2% |
1 |
8% |
6 |
14% |
0 |
0% |
19 |
9% |
|
Out of therapeutic possibility |
0 |
0% |
0 |
0% |
1 |
1% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
0% |
|
Death |
1 |
20% |
0 |
0% |
13 |
16% |
3 |
5% |
2 |
15% |
14 |
33% |
0 |
0% |
33 |
16% |
Table 3 MFP rehabilitated individuals' clinical characteristics in the dentistry section of a Brazilian oncology reference center, from august 2015 to august 2020 (n= 235).
a= 29 missing data; b= 133 missing data; c= 26 missing data.
* Adenocarcinoma denomination included: 2 adenocarcinomas, 1 low-grade adenocarcinoma, 2 basal cell adenocarcinomas, and 19 low-grade pleomorphic adenocarcinomas.
** Carcinoma denomination included: 9 basal cell carcinoma, 1 acinar cell carcinoma, 2 clear cell carcinoma, 69 squamous cell carcinoma, 5 epithelial myoepithelial carcinomas, 1 lymphoepithelioma carcinoma, 1 clear cell variant myoepithelial carcinoma, 10 mucoepidermoid carcinomas, 3 sebaceous carcinomas, and 1 unspecified carcinoma.
Specifically, regarding the MFP characteristics, 100% of the obturator, ocular prostheses, surgical plates, and modified lower dentures, and 55% of the nasal prostheses were manufactured in acrylic resin, while for the facial and oculo-palpebral prostheses, the use of silicone predominated (56% and 67% respectively). On average, MFP was used for 9.5 months, with adaptation and satisfaction and without reported adverse events (Table 4). Specifically for facial, nasal, and oculo-palpebral prostheses, which could be made from different materials, the average usage was 7.45 months for those made of acrylic resin and 6 months for the ones of silicone. The MFP hygiene situation was mostly satisfactory for all types of prostheses. Regarding the MFP-associated use difficulties, most individuals rehabilitated with obturator, ocular, oculo-palpebral prostheses, and surgical plates did not report any (73%, 69%, 80%, and 87% respectively); 75% of those with facial and 50% of those with nasal prostheses reported marginal adapting/bonding difficulties; and 100% of the modified lower prostheses users mentioned other kinds of difficulties, highlighting obstacles in retaining the device (Table 5).
|
Variable |
MFP type |
Total |
||||||||||||||
|
Facial |
Nasal |
Obturator |
Ocular |
Oculo-palpebral |
Surgical plate |
Modified lower |
||||||||||
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
MFP fabrication material (n=282) |
||||||||||||||||
|
Acrylic resin |
4 |
44% |
6 |
55% |
104 |
100% |
89 |
100% |
6 |
33% |
49 |
100% |
2 |
100% |
260 |
92% |
|
Silicon |
5 |
56% |
5 |
45% |
0 |
0% |
0 |
0% |
12 |
67% |
0 |
0% |
0 |
0% |
22 |
8% |
|
MFP usage time (n=216)a |
||||||||||||||||
|
Mean (standard deviation) |
8.3 (±9.1) |
6.3 (±7.7) |
12.1 (±9.9) |
10.4 (±9.1) |
5.1 (±6.5) |
3.6 (±3.5) |
12.0. (±0.0) |
9.5 (±9.1) |
||||||||
|
Patient’s MFP adaption? (n=206)b |
||||||||||||||||
|
No |
4 |
44% |
3 |
33% |
18 |
23% |
8 |
12% |
3 |
27% |
1 |
3% |
1 |
50% |
38 |
18% |
|
Yes |
5 |
56% |
6 |
67% |
60 |
77% |
60 |
88% |
8 |
73% |
28 |
97% |
1 |
50% |
168 |
82% |
|
Patient’s MFP satisfaction? (n=194)c |
||||||||||||||||
|
No |
3 |
33% |
3 |
33% |
22 |
30% |
13 |
20% |
2 |
18% |
2 |
8% |
1 |
100% |
46 |
24% |
|
Yes |
6 |
67% |
6 |
67% |
52 |
70% |
52 |
80% |
9 |
82% |
23 |
92% |
0 |
0% |
148 |
76% |
|
MFP hygiene situation (n=94)d |
||||||||||||||||
|
Unsatisfactory |
0 |
0% |
1 |
20% |
5 |
14% |
3 |
12% |
1 |
33% |
2 |
13% |
0 |
0% |
12 |
13% |
|
Satisfactory |
8 |
100% |
4 |
80% |
30 |
86% |
23 |
88% |
2 |
67% |
14 |
88% |
1 |
100% |
82 |
87% |
|
MFP use associated adverse events (n=122)e |
||||||||||||||||
|
Allergy to glue, silicone or remover |
1 |
25% |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
29% |
0 |
0% |
0 |
0% |
3 |
2% |
|
None |
3 |
75% |
7 |
100% |
32 |
76% |
42 |
95% |
4 |
57% |
13 |
76% |
0 |
0% |
101 |
83% |
|
Patient broke the prosthesis |
0 |
0% |
0 |
0% |
1 |
2% |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
1% |
|
Radio dermatitis prevented the MFP use |
0 |
0% |
0 |
0% |
0 |
0% |
0 |
0% |
1 |
14% |
0 |
0% |
0 |
0% |
1 |
1% |
|
Trauma and pain |
0 |
0% |
0 |
0% |
9 |
21% |
2 |
5% |
0 |
0% |
4 |
24% |
1 |
2% |
16 |
13% |
|
MFP use associated difficulties (n=101)f |
||||||||||||||||
|
Adapting/gluing the margins |
3 |
75% |
2 |
50% |
1 |
3% |
2 |
6% |
0 |
0% |
1 |
7% |
0 |
0% |
9 |
9% |
|
Hygiene control |
0 |
0% |
1 |
25% |
0 |
0% |
1 |
3% |
0 |
0% |
0 |
0% |
0 |
0% |
2 |
2% |
|
None |
1 |
25% |
1 |
25% |
29 |
73% |
22 |
69% |
4 |
80% |
13 |
87% |
0 |
0% |
70 |
69% |
|
Others |
0 |
0% |
0 |
0% |
10 |
25% |
7 |
22% |
1 |
20% |
1 |
7% |
1 |
100% |
20 |
20% |
Table 4 Characteristics of the dentistry section of a Brazilian oncology reference center confectioned MFP, from august 2015 to august 2020 (n= 282)
a= 66 missing data; b=76 missing data; c= 88 missing data; d= 188 missing data; e= 160 missing data; f= 181 missing data.
|
|
Number of patients included in the study |
Number of records included in the socio demographic and clinical variables analysis |
Number of records included in the MFP variables analysis |
|
One MFP |
137 |
137 |
137 |
|
Two MFP of the same type |
26 |
26 |
52 |
|
Two MFP of different types |
26 |
52 |
52 |
|
Three MFP of the same type |
4 |
4 |
12 |
|
Three MFP, with at least two different types |
7 |
14 |
21 |
|
Four MFP of the same type |
2 |
2 |
8 |
|
Total |
202 |
235 |
282 |
Table 5 Distribution and number of patients included in the study, records included in the socio demographic and clinical variables analysis, and records included in the MFP variable analyses
According to this study's results, it was possible to observe an increase in prostheses manufacturing between the years 2015 to 2019, followed by a reduction in 2020; 2019 was the year of largest manufacture for all MFP types, except the facials. This can be justified by the information dissemination of rehabilitation services among the institution's professionals, who increasingly referred patients for care in the section. On the other hand, the reduction observed in 2020 is probably associated with the COVID-19 pandemic, which implied a reduction in institutional patient flows. Considering all prostheses, the obturators stand out as the most frequent. This can be explained by its direct impact on patients' functional re-establishment, sealing oral communication, preventing food and air passage, and directly contributing to chewing, swallowing, and phonation.6,16 Ocular prostheses also represented a significant portion of the sector’s MFP; even though they do not reestablish function, they are directly related to aesthetics, contributing to the patient's self-esteem reestablishment.17 The higher male and middle-aged individuals' MFP prostheses frequency is consistent with the classically head and neck tumors described profile.18 Likewise, the higher incidence of carcinomas is also consistent with the classically histological head and neck tumors classification,18,19 since carcinomas represent 90% of this region's tumors. It is important to highlight that the age of ocular prostheses rehabilitated individuals was lower when compared to other MFP types, with a higher incidence at 10 years old; this is explained by the predominance of retinoblastoma in this group.20
Regarding the family history of neoplasms, most patients reported as being absent; this information, however, must be cautiously analyzed, since the lack of knowledge of the previous family history and the absence of diagnoses in many cases can represent a confounding factor. Considering education, most patients reported having incomplete elementary education. In this sense, most users of the Brazilian public health system (Sistema Único de Saúde - SUS) belong to the lower social classes, therefore having fewer educational opportunities. Furthermore, when analyzing ocular prostheses rehabilitated individuals, there was a predominance of illiterates, justified by the higher frequency of these tumors in children under 10 years of age.21 Regarding the location, the regions in which the tumors appeared are directly related to the type of prosthesis the patient was rehabilitated with. The rationale for this relationship is based on the need for MFP to rehabilitate a surgical resection or defect generated by the tumor. Furthermore, as there are no other studies with the same proposal as this one, it is hard to discuss this data.
The average evolution time of the lesions until diagnosis was 15.5 months. However, in this sense, it is necessary to consider that regarding the lesion's location and the patient's orientation, there may be a considerable time lapse before the tumoral identification, which can also imply a confounding factor. Clinical staging was mostly of advanced-stage tumors, III or IV, agreeing with the literature and reflecting the Brazilian scenario of late diagnosis.1,22 In this sense, periodic assessment for oral cavity program implementation emerges as an evident need, thus allowing early diagnosis of lesions, directly impacting the staging and patient prognosis. Most of the analyzed patients underwent multimodal therapy, mostly surgery associated with radiotherapy, which is compatible with literature regarding head and neck tumor treatment therapeutic modalities, especially if diagnosed in advanced stages.1 However, regarding survival, most patients had complete remission at the time of data collection, which goes against what is established in the literature, since the expected 60-month survival for stage III tumors is 60-80%, and for stage IV, 20-60%.23 This divergence may be associated with the small number of analyzed individuals, the distinct tumoral histological types and behaviors, or the different follow-up periods.
Regarding MFP variables, all obturators, oculars, surgical plates, and modified lower MFP were confectioned with acrylic resin. This agrees with the previous literature, that elects this as the material of choice for these prostheses.24 Opposedlly, nasal, facial, and oculo-palpebral prostheses can be manufactured of thermally activated acrylic resin and silicone.5,25 In this study, most nasal MFP were made of acrylic resin; the facial and oculo-palpebral ones were made of silicone. It is worth noting that although acrylic resin has a lower cost when compared to silicone, is more durable, and is more easily obtained, it does not have flexibility, which is essential for the prosthesis aesthetics patients require. Silicone is closest to the ideal in this sense,7,9 as it allows for more satisfactory aesthetics, is easier to color, is simple to handle, allows thin margins, and has adhesive compatibility;5,26 however, it has a high associated cost and is difficult to obtain in the country since most of the existent brands are foreign.14 The MFP duration was mostly 0 to 6 months, with those of acrylic resin lasting an average of 7.45 months and those of silicone, 6 months; the data regarding MFP duration in literature is not unanimous, with studies indicating an average duration of 6 months5,27,28 and others, between 1.5 and 2 years.7 However, it is necessary to consider that marginal deterioration of the prostheses (both by loss of material properties and by breakage), changes in color, and colonization by fungi are classically clinically observed in this device, related directly to the usage time, ultraviolet radiation, factors related to the environment and patient hygiene and can directly impact the reduction of the prosthesis's useful lives.5,7,9,26 In addition, it may also be needed to replace the prosthesis due to changes in the surgical defect, disease recurrence, or post-operative tissue shrinkage.27
The patient’s adaptation and satisfaction with the prostheses were observed in most cases and hygiene was recorded as satisfactory. Most patients did not report any adverse events or difficulties associated with MFP. Among those who reported, the complaints were mainly in those with facial and nasal prostheses, related to marginal adaptation and bonding. This can be justified by the facial mimic muscle movement, causing maladjustment and making its use more difficult. In silicone MFP this adaptation can be optimized using glue to marginal adapt, but implies an additional cost for the patient and the need for manual dexterity to perform this process.28 Furthermore, it is important to highlight that 3 cases (2%) of allergy to glue or silicone were identified, which can also be considered a limiting factor for silicone prostheses. Regarding MFP-related adverse effects, the modified lower prostheses patients stand out, referring to pain and trauma associated with use. It is necessary to consider the additional difficulty associated with these cases in the rehabilitation process. The prosthetic instability caused by the greater bone resorption in the mandible, leaving a smaller area for support, is added to anatomical defects such as bone resection region, flap, or tongue fixation to the floor or gingival ridge. This compromises the prosthesis adaptation and makes it prone to cause trauma and pain during use.13
Due to the limitations of this study model and understanding that the absence of data in many medical records is linked to the fact that the study is based on secondary data from the medical records, the importance of correct filling and legible letters is emphasized. Despite this, the results of the present study show the importance of rehabilitating patients through MFP, aiming at the recovery of speech, chewing, swallowing, breathing, aesthetics, self-esteem, and reintegration into their social functions. This process should be part of the multidisciplinary and comprehensive treatment to which patients are submitted.29,30 Understanding that INCA represents, in the national context, an oncological treatment center of reference, it becomes clear that this Dentistry service concentrates on a high number of cases most patients with these needs. This scenario becomes even more significant when we consider that this is the only institution in Rio de Janeiro state that makes MFP free of charge.31 Furthermore, this study is the first to trace the epidemiological profile of MFP rehabilitated patients in a national scenario, constituting, therefore, a reference point in the structuring of a complete rehabilitation system flows for these patients. As it was carried out in a reference institution at the national level, its results can be useful in elaborating specific public policies for comprehensive care for patients with head and neck tumors.
From August 2015 to August 2020, 202 individuals were rehabilitated in the Dentistry section of Instituto Nacional de Câncer, through 282 MFP. The most common type of prosthesis was the obturator, with 2019 being the year with the highest number of MFPs manufactured. These data highlight the importance of MFP as an effective and accessible tool in the rehabilitation process especially in cases where rehabilitative surgery is not possible. The MFP contribute to aesthetics, self-esteem and the development of physiological functions. Finally, these results highlight the need for a multidisciplinary team to work in oncology, with the dentist being an essential player in this context.
None.
The authors declare that there are no conflicts of interest.

©2024 Alves, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.