Journal of
eISSN: 2373-633X


Mini Review Volume 13 Issue 5
Community Care, Department of Veterans Affairs Medical Center, USA
Correspondence: Alexandria K Reddelle, Community Care, Department of Veterans Affairs Medical Center, Columbus, USA, Tel 206-549-5164
Received: September 13, 2022 | Published: September 22, 2022
Citation: Reddelle AK. Battlefield Acupuncture (BFA): theoretical use in pre and post operative back surgery pain control. J Cancer Prev Curr Res. 2022;13(5):121-123. DOI: 10.15406/jcpcr.2022.13.00500
Chronic back pain is a common ailment due to various conditions and events. Military personnel have statistically suffered from chronic back pain at higher intervals than their civilian counterparts for various reasons. Whether from standing in military formation for long periods of time, the extreme physical requirements, or injury, it has become a profound and expensive medical condition affecting the overall quality of life. Battlefield acupuncture (BFA) was developed by Dr. Robert Niemtzow as an alternative treatment to manage the pain that affects a multitude of veterans. This article discusses the theoretical use of the BFA treatment technique in the civilian environment for preoperative and postoperative pain control in patients undergoing back surgery.
Keywords: acute pain, chronic pain, battlefield acupuncture, acupuncture, holistic, auricle, back surgery, pain control, post-operative pain, back pain
Chronic pain, defined as persistent and unrelenting for greater than three months,1 consequently has been a significant medical issue for many people. The spinal column contains the pain receptor nerves. Due to this biological fact, post operative spinal surgery pain can be extreme and difficult to manage. Historically prescription medications, including opioids, have been the standard of care. These medications have limited capability and typically do not control the depth of pain experienced. Opioid use can slow down the recovery process and increases the risk of opioid addiction, adding to the opioid crisis in our society.
Exploring alternative treatment is essential to both controlling pain and preventing further complications, including those related to opioid use. Alternative medicine to treat chronic pain has become a common practice over the last decade among providers in the United States. The Department of Veteran’s Affairs (VA) is no different. According to the VA, chronic pain affects more than 50 million people in the United States alone. Studies done by the VA found that chronic pain is “more prevalent and intense among veterans” than among the general population in America.2
Battlefield Acupuncture (BFA) was developed by a U.S. Airforce physician, Dr. Richard Neimtzow. BFA was formulated on the strong beliefs of traditional Chinese medicine. This traditional theory states pain or disease within the body are the result of an imbalance of energy. Stimulation of the acupressure points within the auricular results in an energy pathway activation and thereby reducing pain within the body.3 The belief behind BFA is its probable effect on the pain centers of the central nervous system (CNS) and the auricular somatotopic organization of the body.4
Developed in 2001 as an alternative to opioids, specifically to target chronic low back pain, BFA is a form of auriculotherapy.3 As a focused approach, BFA uses specific points on the body to place continual pressure, thereby reducing pain. Using specific points on the auricular site (or ear), five tiny sterile pins are placed in specific spots in the outer ears bilaterally. The pins remain at their insertion site for approximately 3-4 days and fall out on their own. This procedure takes only a few minutes to complete for the experienced and well-trained provider.
Through the mapping of acupuncture medicine in the following diagrams the appropriate placement for the BFA needles is seen, figure 1. This placement has been found to be the most effective sites for distribution and proper pain control. Five predetermined locations in the auricle (outer ear) based on specific acupressure points, the cingulate gyrus, thalamus, omega 2, point zero, and the Shen men. These specific areas of the outer ear, figure 1 identifies acupressure points of the ear which correlate to specific areas of the body.
Figure 2 identifies the specified points where BFA is placed. When comparing the two pictures it is evident the placement of BFA maintains constant pressure on these identified acupressure points for continual relief. Reportedly the use of BFA has resulted in a significant reduction of both acute and chronic pain as well as neuropathic pain.4
BFA was not meant as a replacement for physical therapy but only as a method to manage chronic low back pain more effectively in relation to opioid use. Physical therapy is essential to recovery and return to normal function, but physical therapy alone is not always effective. According to the Department of Veteran’s affairs, approximately 80% of those who undergo BFA treatment find the relief sought.
Federman et al.,11 conducted a study of 112 veterans receiving BFA. The study showed an average pre-treatment pain level of 6.8 (on a 0-10 scale) which decreased to 2.4 immediately following receiving BFA. Approximately 88.4% of veterans in the study exhibited this sudden decrease in pain. Additional information from the study found that the decrease in pain continued through the following thirty days. Measured at day 0,1,7, and day 30, the post treatment analysis found that while at day 1, 80.7% continued to have decreased pain, and at day 7, approximately 52.4% of veterans who received treatment still reported significant pain relief. At day 30, 51% of those treated continued to report a decrease in pain level. This study determined that BFA has both short and long term affects on decreasing chronic low back pain and could be useful for long-term care.
Both this study and personal experiences have proven the BFA treatment to be effective in the majority of patients who received it. Pre and post operative pain relief for back surgery patients is the next step in managing such a difficult area of the body to treat.
Over the years, more conservative approaches have been developed to help patients. A more holistic approach that lessen medical expenses and improve the overall quality of life to control chronic pain have proven beneficial. BFA is a minimally invasive procedure developed to address chronic back pain conditions among veterans. Over the last ten years, BFA has been established and integrated into VA medicine with great success. Through the specialized training among approximately 1500 VA physicians, this treatment has become common place within the Veterans Health Administration (VHA) and is part of the physical medicine and rehabilitation department. BFA is meant to manage chronic low back pain and not replace physical therapy need.
While veterans reportedly have a significantly higher incidence of chronic back pain, the civilian world also suffers from this condition at a large rate. This condition can be debilitating and disruptive to daily life. Finding alternative means of treatment that is not only cost effective but also minimally invasive and easily incorporates into the busy lifestyles of today, is beneficial to the overall wellbeing of the patient and can enhance their quality of life.
Many patients who suffer from chronic back pain choose a surgical option to relieve this pain with the goal of returning to normal function. Back surgery is a very invasive procedure which comes with potential complications and a significant amount of pain. Patients who chose this option are typically to a point of no other choice for a more permanent solution for the chronic pain. The following picture (figure 3) illustrates the most common surgical procedure, Laminectomy, these patients undergo.
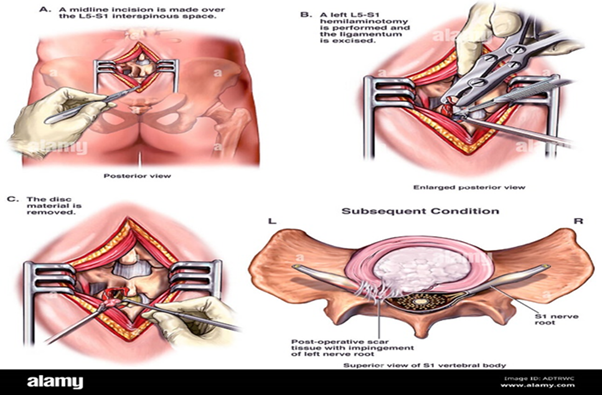
Figure 3 Surgical procedure, laminectomy.7
According to Correll,5 multiple factors contribute to post operative pain. These other factors can range from anxiety, and other psychological factors, such as depression to functional loss. During the initial postoperative phase, the first few days to week are critical as patients will typically experience the highest intensity of pain. Maintaining proper pain control in this initial phase affects the healing process and overall recovery. Appropriate pain control and timely return to normal function is essential to an improved outcome. According to studies, proper pain control is directly related to the healing process.6 While timing of the BFA insertion is not critical, administering the treatment prior to leaving the operating room or immediately in the post operative phase 1 would provide the most initial benefits for pain control. For pre-operative pain control, this treatment would be best utilized one week prior to the scheduled surgery.
Implementing BFA as a means of pain control pre and post operatively
As a non-pharmacological and minimally invasive means to control pain and given its proven success, BFA theoretically could be used in the surgical arena. As holistic approaches have been breeching the threshold of medicine for the last decade, they have shown significant improvement in overall health and wellbeing. With the focus being patient-centered care that provides the most comprehensive overall improvement of health and wellbeing.5 Dr. Niemtzow contended that implementing new advancements within a large health system is a process and typically met with adversity.6-10
The training developed within the VHA for this treatment can be adapted to the public arena. Currently, forms of BFA are already becoming available to the public, while not widespread yet, BFA has the potential to become common place in the civilian as it has become a regularly used treatment in the VHA. According to Dr. Niemtzow there are barriers to overcome when implementing a new program within a large healthcare system. He identifies five main steps to overcoming barriers, beginning with selecting an evidenced based product or treatment that is safe and reproducible and standardized training from highly qualified instructors to having ongoing support through technology and/or qualified personnel.10
As the BFA system has already been implemented successfully within the VA and ongoing for several years, coordination with this organization for program establishment and training support would be advised.
Research is continually ongoing for noninvasive pain control and avoidance of opioids for both the back and neck. BFA has been proven to be an effective and alternate means of managing the chronic pain experienced by more than half the nation’s veterans. BFA is a cost-effective and a non-invasive means of controlling pain. Through the use of BFA in the immediate postoperative period, theoretically the pain can be significantly reduced resulting in not only improved pain control but a decrease in the use of opioids. BFA is not intended to replace necessary physical therapy, only assist in pain control, particularly in the critical timeframe of post operatively. As BFA was developed to assist with back pain, this paper on theoretical use is constrained to back surgery patients only.
Studies have shown this to be an effective means of pain control. This procedure can be beneficial for use in the private sector to reduce pain both preoperatively and postoperatively, specifically with patients undergoing back surgery. This article discusses the use of BFA and its benefits not only in the veteran population, but its potential use in the civilian environment to manage preoperative and postoperative pain. The non-pharmacological treatment could have significant advancement in post operative pain control. Based on the success of BFA treatment among the veteran population shows this minimally invasive treatment to have potential for application in the civilian sectors. Through appropriate training and application, BFA can benefit an increased number of patients undergoing back surgery. Based on the evidence of noting the success of BFA for pain control, personal experience, and professional insights, BFA could prove to aid in the healing process and increase the patient’s potential for recovery and return to an active lifestyle more quickly.
None.
Authors declare that there is no conflict of interest.

©2022 Reddelle. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.