Journal of
eISSN: 2373-633X


Febrile neutropenia (FN) is characterized by a decrease in neutrophils number to values below 500 cells/ mm3 and an occurrence of fever higher or similar to 38.3ºC. It commonly occurs in cancer patients as a result of chemotherapy regimens. Chemotherapy destroys carcinogenic cells but also attacks in many cases some normal cells including essential elements of the immune system. Fever is one of the characteristic symptoms of FN and is usually associated with the presence of an infection caused by various microorganisms.
Bacteria, including Gram-positive isolates (currently dominating) and Gram-negative species (Dominant in the 1970s), are usually reported as the main microorganisms responsible for FN and cause complicated infections leading to death. Other types of microorganisms such as fungi and viruses are also associated with the condition. The incidence and epidemiology of FN are variable according to a multitude of factors such as the type of cancer, the age, and sex of the patient, the type and cycle of treatment.
The morbidity and mortality rates of FN have decreased over the years as a result of the use of appropriate antibiotic treatment, preventive measures, risk assessment procedures and adequate patient management plans. However, FN, mainly associated with complicated infections remains a significant threat and an oncological emergency. The threat is amplified with the continuing occurrence of antibiotic resistant microorganisms, which causes infections that are difficult to treat, leading to the death of millions of people worldwide.
Due the oncological significance of FN, the development of new technologies and medications for cancer treatment for use in modern medicine should take into account the risks associated with the occurrence of FN.
Keywords: febrile neutropenia, cancer, chemotherapy, sepsis, neutrophils, immunodeficient
Due to the type and intensity of treatment received and other risk factors, many cancer patients experience a decrease of elements of the immune systems that make them more exposed to various infections. In the latter condition, the body in not able to fight against the causative agents effectively. One type of blood elements whose number commonly decreases during cancer is the group of neutrophils, which constitutes the first line of the body defence against diseases. The decline in the neutrophils number associated with fever is known as febrile neutropenia (FN). Neutropenia is considered as an oncology emergency and can lead to serious adverse consequences such as serious infection complications and death.1,2
The appearance of fever during FN is usually related to the presence of various microorganisms, including bacteria, fungi, and viruses. The most severe infections are seen with Gram-negative bacteria, which used to be the predominant bacteria in FN in the 1970s.
However, Gram-positive bacteria, which became the main microorganisms in the 1980s and well as, fungi and viruses can also cause life-threatening infections leading to significant morbidities and possible mortality in the immune deficient neutropenic individuals.1,2 It is hard to prevent the occurrence of FN in people undergoing intensive chemotherapy, but preventive measures can be applied to diminish the risks factors and broad range antibiotic treatments are given to patients with suspected FN. A modification of the dose and period of chemotherapy as a result of neutropenia may have severe consequences in the long-term on the outcome of cancer especially those being treated with a curative intend.
With the development of new technologies, pharmacological tools, and medications, the occurrence of new pathogenic microorganisms including microbes that used to be non-pathogenic is eased and this associated with the increase of antibiotic multi-resistances constitute a serious public health concern at a global level Viscoli et al.3 The current review aimed at providing an overview of the type of infections that are associated with FN.
Neutropenia is a condition characterized by an abnormal low concentration of neutrophils granulocytes (<500 cells/mm3), the most abundant circulating white blood cells that constitute the first line of the organism defence against infections Viscoli et al.3
Various symptoms are related to neutropenia, and when the condition is associated with fever (≥38.3ºC), it is referred to as febrile neutropenia (FN). The occurrence of fever is generally the result of a microbial infection as the patients are immune-compromised and more subject to infections. Any type of neutropenia can develop into febrile condition, but cancer patients undergoing chemotherapy usually exhibit the condition especially when the treatment suppresses the bone marrow from producing blood cells. It is commonly reported that a neutrophils count lower than 500cells/mm3 is indicative of neutropenia. However, this number can vary depending on different factors such the severity of the condition. For example, a neutrophil count below 1000 cells/mm3 is considered moderate Lustberg1 2012 whereas a very profound neutropenia is characterized by a neutrophil count below 100 cells/mmmm3 Kristjanson.4 Table 1 described different definitions of FN reported by health institutions in different countries.
Source |
Fever (ºC) |
Neutropenia (x 109 cells/L) |
Bugs & Drugs ( 2012) |
≥38.3 oral temperature or ≥38.0 over 1 hour |
ANC < 0.5 x 109/L (500 cells /mm3) |
Infectious Diseases Society of America (2011) |
≥38.3 |
ANC <0.5 or predicted decline to <0.5 over next 48 hours |
National Comprehensive Cancer Network (2011) |
≥38.3 oral temperature. or ≥38.0 over 1 hour |
ANC <0.5 or <1.0 with predicted decline to ≤0.5 over next 48 hours |
European Society of Medical Oncology (2010) |
>38.5 oral temperature or 2 consecutive readings of >38.0 for 2 hours |
ANC <0.5 or predicted decline to <0.5 |
British Columbia Cancer Agency (2008) |
>38.3 |
ANC <0.5 |
Japan Febrile Neutropenia Study Group, 2005 |
≥38.0 single oral or ear probe temperature or >37.5 single axillary temperature |
ANC <0.5 or <1.0 in subjects with predictably deteriorating clinical condition |
Table 1 Published definition of febrile neutropenia18
Febrile neutropenia is routinely screened in cancer patients undergoing treatment such as chemo/radiotherapy. It is diagnosed by e.g. a physical observation to screen the occurrence of fever and a complete blood count test to screen a decrease in the number of blood cells and especially neutrophils Lustberg.1
One of the most life-threatening complications of cancer treatment is FN whose incidence is variable according to different factors, such as the type and cycle of therapy, the type of cancer, the sex and related conditions of the patients. The incidence of FN in the USA is estimated at 60,294 per year including 7.83 cases per 1000 cancer patients. Moreover, the incidence rises to 43.3 cases per 1000 in individuals that are suffering from hematological malignant tumours BMJ Best Practice.5
Jacob et al.6 conducted a study on the occurrence of FN in individuals suffering of solid tumours and hematological malignancies who were undergoing chemotherapy at a health institute in India. All cases of FN (including 75 episodes of FN and 55 patients) that occurred from July 2011 to December 2011 were collected and screened. The investigation revealed that FN episodes occurred more frequently in patients with solid tumours (57%) than those suffering from hematological malignancies and were associated more with Gram-negative bacteria infections (56.25%). However the morality level between the two types of patient was not significantly different (14% vs. 12.5%). Also, although more infections were related to Gram-negative bacteria, a higher mortality rate was seen with Gram-positive microorganisms.
To screen the incidence of chemotherapy-induced neutropenia and current practice of prophylaxis with granulocyte colony-stimulating factors (G-CSF) in cancer patients, Jolis et al.7 conducted a study on patients suffering from breast cancer (734) and lymphoma (291) from different health center’s in Spain. These patients who were starting chemotherapy were believed to be at risk of developing FN at a rate of ≥ 10%. It was revealed that after the initial four chemotherapy cycles, cancer patients developed 3-4 grade neutropenia (absolute neutrophils count <1.0 × 10(9) /L) and FN (absolute neutrophil count <0.5 × 10(9) /L and fever ≥38 °C) with an incidence of 11% and 4.3% respectively. Patients suffering of lymphoma exhibited a higher incidence of 40.5% for 3-5 grade neutropenia and 14.8% for FN. The rate of required hospitalization due to FN was 2.0% and 12.0% for breast cancer and lymphoma patients respectively.
Schelenz et al.8 demonstrated the variability of the incidence of FN according to several factors including e.g. cancer type, chemotherapy regimen, antibiotic treatment, age and sex. Patients suffering from both solid tumours and FN and receiving a routine care at a local cancer centre in the UK were investigated over a one year period. It was shown that the incidence of FN over the 12 months period was 19.4 per 1000 oncology admissions. The cancer types that were most associated with FN were breast, lung, ovarian and esophageal malignant tumours, accounting for 27%, 16%, 13% and 13% respectively. With regards to the age and sex, the mean age was 63 years (71.9% were at least 60 years old) and 56% of patients was female. Table 2 provided more information about the type of cancer and patients screened as well as the outcomes of the study.
Underlying cancer |
No. (%) |
Death No. (%) |
Age (%), >60 years |
Breast cancer |
9/32 (28.1) |
0/9 (0) |
5/9 (56) |
Lung cancer |
5/32 (15.6) |
1/5 (20) |
5/5 (100) |
Oesophageal cancer |
5/32 (15.6) |
0/5 (0) |
4/5 (80) |
Ovarian cancer |
4/32 (12.5) |
2/4 (50) |
3/4 (75) |
Brain tumour |
2/32 (6.3) |
2/2 (100) |
2/2 (100 |
Sarcoma |
2/32 (6.3) |
0/2 (0) |
0/2 (0) |
Pancreatic cancer |
1/32 (3.1) |
1/1 (100) |
1/1 (100) |
Bladder cancer |
1/32 (3.1) |
0/1 (0) |
1/1 (100) |
Colorectal cancer |
1/32 (3.1) |
0/1 (0) |
1/1 (100) |
Thyroid cancer |
1/32 (3.1) |
0/1 (0) |
1/1 (100) |
Melanoma |
1/32 (3.1) |
0/1 (0) |
0/1 (0) |
Total |
32 |
6/32 (18.8) |
23/32 (71.9) |
Table 2 Distribution of cancer type, mortality and febrile neutropenia.8
The epidemiology of FN is also variable according to several factors. It has been reported that 50% of deaths in patients receiving chemotherapy for solid tumours is attributable to FN. In patients being administrated chemotherapy for acute leukemia, FN represents 50% to 75% of deaths. The rapid administration of antibiotics has triggered a response rate of up to 60% to 70% and reduced the mortality to 10%. In the USA, a mortality rate associated with grade 3 and 4 neutropenia ranging from 3.4 % to 10.5% with an overall mortality ranging from 6.8% to 9.5% was reported Ozguler.9
There have been some significance advances in the prevention and treatment of FN that have led to a decrease in the number of death. However, the condition remains one of the most worrying complications of chemotherapy de Naurois.10
In patients suffering of solid tumors and some hematological malignancies, the overall mortality rates are 5% and 11% respectively. This increases to 15% in patients with confirmed bacteraemia related to Gram-negative bacteria, whereas Gram-positive bacteraemia accounts for 5% de Naurois.10 The group of patients which is at a higher risk of FN and which exhibits the worst morbidity and mortality rates is constituted by the elderly patients.
In the study of Schelenz et al.,8 conducted in the UK, it was shown that the epidemiology of FN varies according to e.g. the type of cancer and the age. The total mortality rate was 18.8%, and 83% of the patients who died were aged 60 or over. No FN related death was observed with patients suffering from melanoma, thyroid cancer, colorectal cancer, bladder cancer, and sarcoma and oesophageal cancer. The rest of the types of cancer exhibited a variable mortality rate (Table 2).
According to National Comprehensive Cancer Network (NCCN) guideline Patients who develop neutropenia can be categorized as at low risk or high risk of complications. The practical implication of risk assessment is to allow the development and implementation of a management plan (Figure 1) To be applied to the particular FN case (e.g. type of treatment, outpatient or hospitalization) Villafuerte-Gutierrez.2
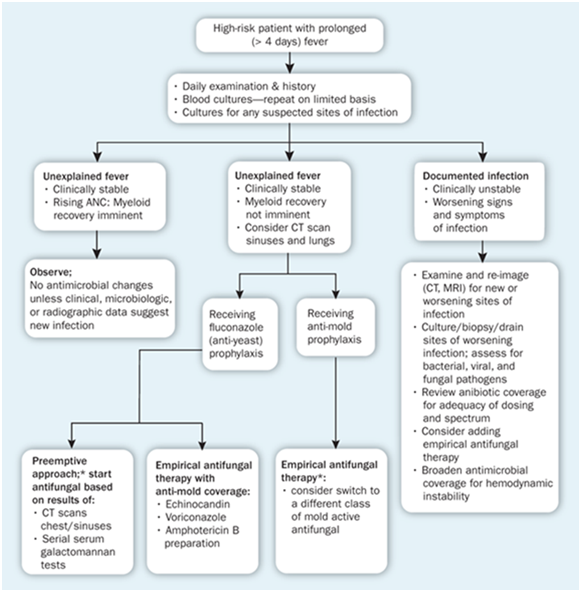
Figure 1 Example of initial management of a patient suffering from febrile neutropenia.19
The National Comprehensive Cancer Network (NCCN) and other institutions have issued guidelines for the stratification of FN risks and encourage the usage of the Multinational Association for Supportive Care in Cancer (MASCC) index to identify patients according to the risk t According to the MASCC scores, a patient with a score <26 is to be considered at low risk and treated as an outpatient, whereas a patient with a score> 21 is at high risk and should be hospitalized. Table 3 depicts the conditions associated with patients at low and high risk according to the NCCN and other guidelines.
Low risk Low risk |
High risk |
(most of the factors listed below) |
(any of the factors listed below) |
no high risk factors |
|
MASCC risk index score ≥21 |
MASCC risk index score <21 |
outpatient status at time of development of fever |
inpatient status at time of development of fever |
no associated acute comorbid illness independently indicating inpatient treatment or close observation |
insignificant clinical comorbidity or medically unstable, including: |
Hemodynamic instability |
|
anticipated short duration of severe neutropenia (≤100 cells/mcL for <7 days) |
anticipated prolonged severe neutropenia (≤100 cells/mcL and ≥7 days) |
good performance status (ECOG 0-1) |
uncontrolled/ progressive cancer; pneumonia or other complex infections at clinical presentation; alemtuzumab therapy; mucositis grade 3-4 |
no hepatic insufficiency |
hepatic insufficiency (five times ULN for aminotransferases) |
no renal insufficiency renal |
insufficiency (creatinine clearance <30 mL/minute) |
<60 years |
|
Cancer partial or complete remission |
|
No focal findings of infection |
|
Temp <39 °C |
|
Normal chest x ray |
|
Absence hypotension |
|
Respiratory rate ≤ 24 |
|
No chronic lung disease or diabetes |
|
No dehydration/ confusion |
|
No history of fungal infection or antifungal therapy in past six months |
Table 3 Characteristics of patients at risk for complications from febrile neutropenia18
The microbiological profile of FN associated infections has evolved internationally over the years. It has been stated that in the 1060 and 1970s Gram-negative microorganisms were mainly reported (60 to 70%), whereas in the 1980s and 1990s, Gram-positive bacteria dominated (55 - 70%).3,4,11 The mechanisms behind this shift in not well known but may be attributed to factors such as the type of treatment that have undergone various modifications as a result of modernization. The intensification of cancer treatment have resulted in the occurrence of more severe oral mucositis and diarrhea that cause significant damage of mucosal barriers and an elevated risk of local Gram-positive microbial infections. Also, the increased use of partially or totally implantable intravenous catheters may have contributed to the occurrence of staphylococcal infections Viscoli et al.3
Kristjanson4 reported that the common bacteria isolated from blood cultures are coagulase-negative staphylococci and Viridans group Streptococci and that the frequency of antibiotic-resistant Gram-negative bacterial infections is increasing. The Gram-positive bacteria commonly reported in FN associated infections are coagulase-negative staphylococci, Staphylococcus aureus, including methicillin-resistant isolates, Enterococcus species, including those which are resistant to vancomycin, Viridans group streptococci, Streptococcus pneumoniae (increasing macrolide resistance), Group A β-haemolytic streptococci such as Streptococcus pyogenes Kristjanson.4
For Gram-negative microorganisms associated with FN infections, different types of bacteria have also been reported including e.g. Escherichia coli (most common GNB), species of Klebsiella, Enterobacter, Citrobacter, and Acinetobacter as well as Stenotrophomonas maltophilia, and Pseudomonas aeruginosa Kristjanson.4
A broad range of antibiotics are used to treat cancer patients who exhibit a febrile condition and there are many resistant microorganisms that cause further complications. Antibiotic resistance is a current serious international public health concern and special care with regards to resistant microorganisms is need. Well known resistant bacteria associated with cancer patient febrile infections include e.g. methicillin-resistant Staphylococcus aureus (MRSA), coagulase-negative staphylococci, vancomycin-resistant enterococci, viridans group streptococci, ciprofloxacin-resistant Escherichia coli, and Pseudomonas aeruginosa Zuckermann et al.12
Some FN infections are not associated with bacteria but other types of microorganisms such fungi mainly may also be present. It is estimated that more than 20% of all neutropenic patients may develop systemic fungal infections whose causative agents include Candida, Aspergillus, Fusarium, Scedosporium species mainly (90%) Donowitz et al.11
Zuckermann et al.,12 conducted microbial investigations of FN patients and revealed that the causative agents include bacteria (43.5%) and fungi (5.7-6.1%). In the period 2001-2003, the latter authors observed 52.8% and 47.2% prevalence of Gram-positive and Gram-negative bacteria respectively. For 2004-2005, a prevalence of 38.1% and 61.9% for Gram-positive and Gram-negative bacteria respectively was observed. The predominant Gram-negative bacterium was Pseudomonas aeruginosa, including multi-drug resistant isolates, whereas Oxacillin-resistant Staphylococcus species was the most isolated Gram-positive bacterium.
A study conducted by Hakim et al.13 on FN in children with cancer showed the presence of bacteria and viruses in the patients. Bacteria included e.g. Viridans streptococci, Escherichia coli, Pseudomonas aeruginosa, Coagulase-negative staphylococci, Klebsiella pneumonia, Capnocytophaga sputigena, Staphylococcus aureus, Bacillus cereus, Enterococcus gallinarum, Enterobactercloacae, Moraxellanon liquifaciens, Eikenella corrodens and Clostridium difficile. The viruses included isolates of EBV (Epstein Barr virus), HSV (herpes simplex virus), RSV (respiratory syncytial virus), Para influenza virus, Influenza, Rhinovirus, Adenovirus and Rota virus.
Although various organisms are identified, the causative agents and infection focus of many FN remain unclear and a resurgence of Gram-negative bacteria has been observed lately Zuckermann et al.11
Neutropenia is most commonly seen as a result of cytotoxic therapy although the ANC of individuals can drop significantly through cancer’s direct interaction with hematopoiesis (e.g. in leukemia) or the bone marrow metastatic replacement Lewis et al.14
The types of chemotherapy that can highly induce neutropenia include products such as the anthracyclines, taxanes, topoisomerase inhibitors, platinums, gemcitabine, vinorelbine, and certain alkylators like cyclophosphamide and ifosfamide Lyman et al.15
When neutropenia is associated with an increase in the body temperature, the patient has usually developed a pathological infection which is caused in 33% of the cases by pathogenic microorganisms BMJ Best Practices .5.
As mentioned earlier various microorganisms including Gram-negative and Gram-positive bacteria as well as fungi and viruses can cause serious infections in cancer patients with FN. The fever associated with FN is believed to be related to the production of cytokines responsible for activating the immune responses that cause the occurrence of fever. The production of cytokines is mediated by exogenous pyrogens Saito & Aiba.16
Lewis et al.14 reported that the nadir in ANC happens 5 to 10 days after the last dose in most outpatients undergoing chemotherapy regimens. Inpatient medications provided for the treatment of e.g. hematologic malignancies usually results in a severe and long term neutropenia. The intensity and length of FN are important risk factors for complications. Other risk elements are e.g. the speed of the ANC decline, previous history of FN or current immunosuppression pre-treatment, augmentation in alkaline phosphatase, bilirubin, or aspartate aminotransferase levels, low glomerular filtration rate and cardiovascular comorbidities.
When neutropenia is related to fever, therapeutic actions are required to help the immune-deficient body target an active infection efficiently. It is advised to hospitalize individuals exhibiting FN and to provide rapidly an initial treatment made broad-spectrum antibiotics. The patients should be kept under close observation until, the neutrophils count is acceptable e.g. > 500 cells/mm3 Lustberg.1
Before administrating any treatment to FN patients, it is important to consider carefully the medical history of the patient and proceed to various examinations and tests in order to provide the best treatment option. Table 4 depicts examples of screening and medications that can be given to cancer patients suffering from FN.
Investigations |
CBC and differential |
Transaminases, bilirubin, alkaline phosphatase |
|
Electrolytes |
|
Creatinine and urea |
|
Blood and urine cultures |
|
Sputum gram stain and culture if productive |
|
AST |
|
Nasopharyngeal swab for viral respiratory panel PCR, if respiratory symptoms are present |
|
Chest x-ray (should be obtained even in the absence of pulmonary symptoms or signs) |
|
Monotherapy |
Cefipime 2 grams IV every 8 hours. |
Carbapenem monotherapy is an alternative to piperacillin-tazobactam. In order to prevent the selection of carbapenem resistance, carbapenems should not be used in first line unless there is a known or suspected infection with ESBL/AmpC cephalosporinase-producing organisms or a penicillin allergy. |
|
Ceftazidime monotherapy is not recommended, as it: 1. Has no reliable Gram positive (Enterococci, Streptococci, Staphylococci) activity compared to piperacillin-tazobactam, 2. May promote antimicrobial resistance (ESBL and AmpC cephalosporinases), 3. Is not optimal in patients with profound (<0.1 x 109/L)/prolonged neutropenia |
|
Combination Therapy |
Piperacillin-tazobactam 4.5 grams IV every 8 hours is the treatment of choice. |
β-Lactam plus an aminoglycoside plus vancomycin is recommended until C&S results are available in patients who are hemodynamically unstable or have septic shock. In such circumstances, vancomycin 15 mg per kg IV every 12 hours should be administered, in combination with either gentamicin 5-7 mg/kg IV every 24 hours or tobramycin 7 mg/kg IV every 24 hours |
|
Recommendations for the Use of Vancomycin |
Empiric vancomycin should not be used routinely, but should be considered in the following circumstances: Concern of a major β-lactam allergy, Obvious IV catheter/tunnel infection, Gram stain of culture reveals gram-positive organism, with organism not yet identified, Known colonization with MRSA or penicillin-resistant S. pneumonia o Hypotension/shock, Quinolone antibiotic prophylaxis oSkin or soft tissue infection o Pneumonia o Hemodynamic instability |
Vancomycin therapy should be stopped on day 2 or 3 if cultures are negative for β–lactam resistant Gram positive organisms. |
|
Anti-Fungal therapy |
Fluconazole |
Voriconazole, |
|
Posaconazole, |
|
Amphotericin B |
|
Itraconazole, |
|
Posaconazole |
|
Caspofungin |
It is difficult to prevent the occurrence of FN, but measures can be taken to decrease the risks of infections, the first action being the maintenance of a good hygiene (e.g. body, environment, and food) for both patients and medical staff. Precautionary measures for FN are variable according to different aspects such as the degree of neutropenia, type of cancer and risk factors. In individual suffering prolonged hematologic malignancies and bone marrow transplantation where prolonged neutropenia is observed it is advised to reduce the contact with pets and live plants. This is not applicable to other types of cancer such solid tumor malignancies where long periods of FN are not observed in many cases Lustberg.1 It has been suggested that a diet low in live bacteria may help reduce the occurrence of FN, but the efficiency was not confirmed. Since FN in cancer patients is usually a direct consequence of chemotherapy, an evaluation of risks factors associated with FN is necessary before any attempt to prevent the occurrence of the condition Klastersky.17
For patients suffering from solid tumors, intensive chemotherapy is provided. Therefore for such patients, the most common chemotherapy medications have been considered as predictable risk and the patients are usually carefully screened and care for to avoid as much as possible the occurrence of FN. However, medication is not the only risk factor, and the other factors should be taken into account. In the elderly patients (aged 65 and over), there is an elevated risk of FN occurrence and particular consideration should be given to this category of patients. Additional FN risks include e.g. the level of the disease, history of FN episodes, lack of prophylaxis and treatment related to other adverse medical condition such as diabetes, cirrhosis that include the use of immunosuppressive agents Klastersky.17
When some cancer medication regimens are used, FN cannot be prevented, but additional procedures can be applied to prevent severe complications. Also, the period of FN can be reduced by using granulocyte colony- stimulating factors (G-CSFs) in particular patients. In the NCCN guidelines, it is recommended that individuals who are at high risk of neutropenia (>20% risk of developing FN) before the beginning of their treatment regimen or who are receiving a chemotherapy regimen that is related to a high risk of neutropenia benefit from the usage of G-CSFs. Reduction of chemotherapy dose and change of the dosing interval are also preventives procedures that can be used Lustberg.1
Lustberg,1 also reported that one important factor that can help in the prevention of FN is the education of patients and their families as it can raise the awareness of individuals about the types of activities that should be avoided or done to minimize the FN occurrence risk and infectious complications during neutropenia. In general, when preventive strategies are applied, many risk factors are reduced, and most patients are able to receive safely and complete the chemotherapy regimen of choice for their malignancy Klastersky.17
None.
The authors declare no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.