Journal of
eISSN: 2373-633X


This article aims to give a brief description of the history and overview of radiation therapy, as well as its most common pediatrics indications, restraint, sedation and treatment techniques employed, and finally discuss the possible side effects that may occur in our small "great "pediatric patients.
The word cancer has always been catastrophic for the patient and family, even when used in a child, who many times in their innocence, faces this struggle as the bravest of their superheroes.
During the last years have made extraordinary advances in surgery, chemotherapy and radiotherapy to treat cancer patients, however from the point of view of pediatric radiation oncology, despite the existence of protocols, improved patient immobilization, sedation, advanced and conventional irradiation techniques, we now know that we should delay the start of it as much as possible, as long as no decision commit with the possibility of cure or quality of life of the patient, a decision that must be taken into a multidisciplinary medical committee, which must rely on the other arms of oncology such as surgery and chemotherapy.
Radiation therapy is the art of using ionizing radiation to destroy malignant cells while minimizing damage to healthy tissue, in turn, ionizing radiations are those that are sufficient to remove an electron orbital energy of an atom. This type of radiation are those that produce biological changes by causing damage to the genetic material of cells, intervening in cell cycle, preventing growth and replication, causing their death if not repaired the damage as soon as possible.1
History
The path of the radiation oncology since the discovery of X-rays by Roengent been tortuous. In 1896 was the first application of X-rays described in a malignant breast tumor, shortly after Becquerel discovered radiation emitted by uranium. In 1898 Piere and Marie Curie discovered radiation emitted by radium salts.
The current brachytherapy has its basis in 1903, being developed in 1920 in various schools: Manchester, Stockholm and Paris. Coutard and Regaud instituted fractionated treatments and multiple entries for treating a tumor, but to that date the effect of radiation in tissues was empirical, using the common term "erythema dose" or redness of the skin, which defined the end of the treatment. In the 50´s can quantify the effects of radiation by cultured cells. Simultaneously pass through kilovoltage, the betatron and subsequently the cobalt bomb, until the appearance of linear accelerators. Was in 90's when radiation therapy has become one of the therapeutic weapons to neoplasms. Now with the development of planning systems, immobilization, imaging, computers, and protocols, we can treat patients using known techniques such as 3DCRT, IMRT, IGRT, SBRT, Brachytherapy, ART, SRS, tomotherapy, proton therapy, etc , achieving a very high dose to the tumor, irradiating the least amount of healthy tissue, thereby diminishing the feared side effects. Also in childhood cancer radiation therapy it has historically been a great contribution. Dr. Harvey Cushing (1869-1939) in 1919, pioneered the use of post-surgery radiotherapy for meduloblastoma2 cases. In 1950 Dr. Edith Patherson recognized the importance of the cranio-spinal irradiation in meduloblastoma3 control. Radiotherapy has been frequently used in some phase of the treatment of Acute Lymphocytic Leukemia, Hodgkin Lymphoma, rhabdomyosarcoma, Nephroblastoma, Ewing sarcoma, CNS tumors, among others.4
Despite advances in the treatment of childhood cancer have increased survival rate in five years to about 80%, cancer in children between 5 and 14years5 remains the second leading cause of death, after accidents.
According to the American Cancer Society (ACS), National Cancer Institute (NCI), Centers for Disease Control and Prevention (CDCP) and the American Association of Central Cancer Registry (NAACCR) (Table 1) covering 90% of the population, estimated in 2014, 15,780 new cases of cancer and 1960 deaths in children and adolescents from birth to age 19. The annual incidence of cancer in children is 186.6 per million children. Approximately 1 in 285 will be diagnosed with cancer before age 20.
Childrens (0-14years) |
Teens (15-19years) |
Acute Lymphocytic Leukemia (26%) |
Hodgkin Lymphoma (15%) |
Brain and CNS (21%) |
Thyroid Carcinoma (11%) |
Neuroblastoma/Ganglioneuroblastoma (7%) |
Brain and CNS (10%) |
Non Hodgkin Lymphoma (6%) |
Testicular germ cell tumors (8%) |
Nephroblastoma (5%) |
Non Hodgkin Lymphoma (8%) |
Acute Myeloid Leukemia (5%) |
Acute Lymphocytic Leukemia (8%) |
Bone tumors (including osteosarcoma and Ewing sarcoma) (4%) |
Bone tumors (including osteosarcoma and Ewing sarcoma) (4%) |
Hodgkin Lymphoma (4%) |
Melanoma (6%) |
Rhabdomyosarcoma (3%) |
Acute Myeloid Leukemia (4%) |
Retinoblastoma (3%) |
Ovarian germ cell tumors (2%) |
All the places (10,450) |
All the places (5,330) |
Table 1 Estimated New cases of cancer in children and adolescents, United States 2014
In Dominican Republic do not have an accurate record of cases of child cancer, however, according to some press publications from various sources related to the subject, for 2010, they appeared just over 300 cases in children under 15years, of which 40% is accounted for Acute Lymphocytic Leukemia.6 According to Dominican Society of Pediatrics, over the past six years, only in the Children's Hospital Dr. Robert Reid Cabral have been diagnosed between 85-90 cases per year.7
Depending on the histology and treatment received, patients survivors more than five years are at risk of recurrence or progression of their disease, as well as to develop secondary malignancies, chronic illness and impairment functional.5
The beggining
All treatment should be started after the discussion of a multidisciplinary committee where must be present or otherwise using current technology through teleconferences: pediatric hematologist oncologists, pediatric oncologists, surgeons, radiation oncologists, neurosurgeons, radiologists, psycho-oncologists, pathologists, nutritionist, nurses, among others.
Once the patient and their parents are sent to the radiation oncologist, has probably spent considerable time, so it is therefore necessary update some studies, you should not perform treatments considering only initial studies or those too old in a disease that can give surprising changes constantly. Of course, it is important to avoid asking those who do not provide us or change some behavior in our patient, particularly imaging studies, we must consider the acronym "ALARA": As Low As Reasonably Achievable".
In relation to this theme an excellent review was undertaken to reduce exposure to radiation from diagnostic medical imaging, promoting a campaign called "Image Gently" to raise awareness of the need to adjust the dose of radiation in medical imaging and need for radiation protection in children; also they implemented the "Image Wisely" campaign, whose goal was to raise awareness on radiation protection in adults. These issues are particularly important in the context of pediatric cancer.8
How does radiation therapy work?
Cancer in adults is often the result of a multifaceted process that usually progresses through several years and may be influenced by environmental factors.
Pediatric tumors usually develop in a shorter period of time. There are often caused by environmental factors, common mutations.
The treatment is limited by the fast-growing normal tissues, which are widely susceptible to radiotherapy and chemotherapy, can cause secondary malignancies.
Radiation therapy acts on the tissues in two ways:
Direct: yielding energy to a biological macromolecule such as DNA, RNA, proteins, causing disruption of the molecules by breaking their bonds.
Indirect: absorbing energy by the water molecule, causing its dissociation (radiolysis) and resulting in the release of H+ ions and free radicals with high chemical reactivity, which tend to recombine to form H2O2, H2O and HO (Figure 1).
This whole process takes place in the cell cycle and should be recalled that the cells are more sensitive to radiation when they are in the G2 and M phase and resistant in late S phase. We must also take into consideration important factors known as the "R" of radiobiology.
Reoxygenation: The fractionation usually allows hypoxic tumor center of a growing tumor, re-oxygenated during intervals between fractions, leading to increased tumor cell killing by free radical formation. Repopulation: During the radiation treatment both normal stem cells and malignant cells can repopulate and the result of this competitive process can influence the therapeutic efficacy. Repair: Fractionation allows normal cells to repair radiation-induced sublethal damage much better than the malignant cells. Redistribution: Those cells as neoplastic fast cycle are prone to death by radiation compared with slow or sluggish growth, which characterizes many normal tissues and finally the radiosensitivity/radioresistance: Capacity of tumor tissue to repair the damage caused by radiation during the corresponding treatment, which would class it as radioresistant and radiosensitive.
Radiation can cause effects, called: Non-stochastic or deterministic
Only occur when the dose reaches a certain threshold value. Its severity depends on the dose received and are usually immediate appearance.
Stochastic: Not required threshold. The likelihood that appear to increase with dose. Often severe and late-onset (radiation-induced cancer).
Immobilization
The time at which a child can cooperate and remain still during treatment is highly variable and depends on several factors: age, previous experience, understanding,9 position during treatment and duration. Some children require general anesthesia for simulation and probably in part or throughout the treatment, which is necessary for the radiotherapy department count on qualified personnel, equipment and areas to do it properly.
With advances in technology and the various equipment capable of delivering radiation, it is essential to maintain a proper immobilization (Figure 2) and accurately to ensure proper treatment, which must be verified by image-guided radiation therapy (IGRT), the treatment (Figure 3) that will be administered (Table 2).
Sedation level |
Characteristics |
Minimum level of sedation/anxiolysis |
Drug-induced state during which patients respond normally to verbal commands. Cognitive function and coordination may be affected. Ventilatory and cardiovascular functions are unaffected |
Moderate sedation / analgesia |
Decreased consciousness induced by drugs, during which patients respond purposefully to verbal, either alone or accompanied by tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained. |
Deep sedation / analgesia |
Decreased consciousness induced by drugs, during which patients cannot be easily aroused, responding to repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. |
Patients may need help maintaining a patent airway, and spontaneous ventilation may be inadequate. Cardiovascular function is usually maintained. |
|
General Anesthesia |
Loss of consciousness induced by drugs during which the patients are not excitable, even by painful stimuli. The ability to independently maintain ventilatory function is affected. Patients often need help maintaining airway and positive pressure ventilation may be required because of depressed spontaneous ventilation or depression drug induced neuromuscular function. Cardiovascular function may be affected. |
Table 2 Definitions of clinical states of sedation, proposed by the American Society of Anesthesiologists
Indications summary
Central Nervous System (CNS) is generally contraindicated in children younger than three years, suggesting chemotherapy to delay the onset of irradiation as much as possible.10–12
Whenever you can, proceed with surgery as first-line treatment, only irradiated tumor bed in high-grade astrocytomas, gliomas, highly selected low-grade non-metastatic ependymomas and subtotal craniopharyngiomas resection.13–16 The irradiation technique includes cranio-axis medulloblastomas, primitive neuroectodermal tumors (PNET) and pineoblastoma (Figure 4). Generally radiotherapy it was administered as adjuvant (chemotherapy « surgery).
Lymphomas: The current treatment protocols often use a tailored approach to risks, combining low-dose chemotherapy followed by radiotherapy at reduced fields meticulously planned in patients at high risk of relapse after complete the treatment and with a previous PET-CT after chemotherapy. Doses range from 15 to 25 Gy depending on the protocol. Radiation therapy may be omitted in early stage Hodgkin lymphoma with complete response to chemotherapy dose of 20-35 Gy have proven sufficient in patients with incomplete response after chemotherapy.17,18 It is important to radiate only positive nodal region "involved node radiotherapy" in those pediatric patients with Hodgkin lymphoma and a substantial reduction in the risk of severe long-term complications is estimated at lower doses in thyroid, lungs, heart and breast in female patients.
Ewing sarcoma: The femur is the most common site of initial presentation, usually presenting the shaft greater commitment. The spread is hematogenous, being the main site of metastases lungs and other bones. Nodal metastases are rare.
Radiotherapy as definitive local treatment indicated in unresectable disease or when surgery involves functional or cosmetic unacceptable compromise. Adjuvant radiotherapy should be considered after subtotal resection (positive or close margins). Dose of 45 Gy in 25 sessions 1.8 Gy/day are suitable for microscopic disease and 50-60 Gy for gross disease.
The total lung irradiation at 12 Gy may be indicated in lung metastases, with cure rates <30%.19
Nephroblastoma: The first treatment option is surgery. This type of tumor is curable in most children. The spread is through peritoneal cavity, especially if perioperative rupture occurred. The first site of metastasis is lung followed by liver. NWTS-4 (National Wilms Tumor Study) indicates that radiotherapy protocol were to be initiated in a period ≤9 days after surgery, a delay usually increases the risk of relapse according to NWTS-2 protocol, confirmed NWTS-3. Stage I-II favorable histology no need radiation therapy. The indication of total abdominal irradiation includes: preoperative tumor rupture, intraoperative diffuse peritoneal dissemination and planting. Usually indicated 10 to 12 Gy to the flank affect (depending on the protocol), after surgery and chemotherapy. The bilateral pulmonary irradiation is indicated in disease stage IV with pulmonary metastases who have not adequately responded to chemotherapy, with the usual dose of 12 Gy, with an additional boost of 7.5 Gy, and unresectable liver metastases could received 19.8 Gy, with daily doses varying between 1.5 and 1.8 Gy.
Neuroblastoma: neuroblasts derived from fetal tissue adrenergic neural crest. The primary originates in the adrenal gland (35%), abdominal and pelvic paraspinal ganglia (30%), posterior mediastinum (20%) and cervical sympathetic chain (1%). Postoperative radiotherapy is not required in the INSS (International Neuroblastoma Staging System) stages I and 2. Recommended irradiation doses to the primary is around 20-25 Gy (1.5 Gy/day) in patients at high risk.
Rhabdomyosarcoma: The initial therapeutic modality should be surgery. There are controversies in the ideal dose of irradiation to achieve local control especially when there postsurgical macroscopic residual disease. The dose may vary between 45 and 55 Gy, depending on the residual disease; prescribing 54-55 Gy in gross disease and 45 Gy with concurrent chemotherapy in microscopic disease. When there is evidence of clinical or pathological nodal commitment often prescribed dose of 45-50 Gy.
Retinoblastoma: most common intraocular tumor in childhood (3-4 years). Hereditary in 40% of cases. Leukocoria usually present with strabismus and increased volume. Forecasts negative factors include invasion of the orbit, the optic nerve, spread to the central nervous system and bilateral tumor. Enucleation is indicated if tumor produces unilateral blindness, invasion of the optic nerve or choroid, glaucoma or tumor recurrence. Ideally by irradiating it is to achieve adequate and uniform dose to respect as much healthy tissue. They can be use radioactive plates with Co60, Ir192 and Ru103 in tumors 2-16mm, ≥3mm from the fovea, and <10mm thick preferably used with 125. When retinoblastoma is multifocal, close to the macula, optic nerve or vision preserved enucleation is very drastic and treatments such as photocoagulation, cryotherapy or radioactive plates are not suitable. In these cases, the external radiation dose of 40-45 Gy is acceptable (Figure 5) when administered chemotherapy can be decreased to 35-40 Gy.20,21
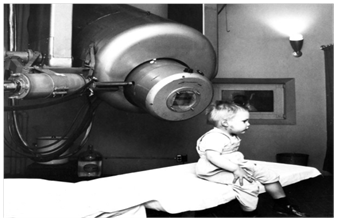
Figure 5 Isaac Gordon: first pediatric patient treated for retinoblastoma linear accelerator in 1957.
Delayed effects
While it is true that with technological advances, types of immobilization, decreased total daily dose and have slowed late effects associated with radiotherapy, they have not been able to eliminate, meriting a very close monitoring of patients. In tissues children develop are at different rates and sequences, but in the same adults tissues are in an equilibrium state with relatively slow kinetics of cell renewal. The vulnerability of the tissues to radiation usually increases during periods of rapid proliferación.22 There are no Emami23 tables or pediatric QUANTEC,24 however there are tables that suggest certain limitations to organs such as: thyroid ~ 20 Gy, teeth ~10.4 Gy, bones ~10 Gy, testes 1.2 Gy, ovaries 6-10 Gy, eyes~10 Gy (cataract), 25 Gy (dry eye), but for example, some studies have reported no toxicity in pediatric patients with brain stem gliomas treated with opposing lateral fields at doses of 54-60 Gy/2 Gy daily. The main limitation of these was the short survival of patients, less than 12 months.
Apart point: stereotactic radiosurgery
It is a treatment technique that allows to concentrate high doses of ionizing radiation in a single fraction generally, but not exclusively (1-5 sessions) on a well defined volumetric injury or anatomical structure and spatially neighboring structures respecting all achieved by the principles of stereotaxy. The name of the procedure is radiosurgery, and can be performed with various well known and FDA (Food and Drugs Administration) equipments like GammaKnife, Linear Accelerator and CyberKnife (Figure 6). Pediatric intracranial stereotactic radiosurgery can be used in low and high grade gliomas, medulloblastoma, ependymoma, arteriovenous malformations (AVM), among others. In the Eight Annual International Symposium of Stereotactic Body Radiation Therapy (SBRT) and Stereotactic Radiosurgery (SRS) held in United States, Orlando Florida in February 2015, they suggested that it would be an indication in inoperable low and high grade gliomas, as adjuvant or recurrence. In medulloblastoma and ependymoma boost or as reinforcement to bed or residual tumor, recurrence and metastases. In arteriovenous malformations (AVMs) are administered dose range from 15.5 to 18 Gy in one session (2-5), but in two to five session the dose range is usually 17 Gy. Factors favoring a complete response in this type of vascular lesions are: nidus <2.5cm, single drainage vein, volume and single session.
The multidisciplinary approach is essential to achieve improved survival daily. In the vast majority of cases, the first option is surgery or chemotherapy, existing exceptions like the dreaded pontine gliomas where the first choice is radiotherapy, irradiation of rest tumors should be delayed with the use of chemotherapy as much as possible, provided that do not compromise the patient's prognosis. We must notify the patient and/or family members own side effects of treatment that is about to be used. Daily use of anesthesia or sedation improves immobilization techniques and along with images of daily check pretreatment, we reduced field sizes to be irradiated. Always have to know the toxicity caused. Using modern techniques irradiation, significantly reduce the likelihood of side effects. It is essential the image fusion of CT-MRI-PET CT in the definition of treatment volumes and is recommended to reduce the total dose of radiation, the daily fractionation and treatment volumes following the many guidelines and consensus published.
None.
The authors declare there is no conflict of interests.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.