Journal of
eISSN: 2469 - 2786


Case Report Volume 2 Issue 4
1Major General Hugh G Robinson Center for Neuropsychiatric Studies, USA
2Department of Neurology, Columbia College of Physicians and Surgeons, USA
Correspondence: Tony L Brown, Department of Neurology, Columbia College of Physicians and Surgeons, USA
Received: April 11, 2016 | Published: September 20, 2016
Citation: Ferdinand S, Meloche TM, Brown TL. Mycobacterium marinum: a case report. J Bacteriol Mycol Open Access. 2016;2(4):98-100. DOI: 10.15406/jbmoa.2016.02.00032
A 47-year-old male developed a lesion on his right hand after sustaining an abrasion which progressed to formation of other lesions that spread proximally on his right arm and resulted in an abscess to his right elbow. Eventually, he was diagnosed with a skin infection whose etiological bacterium was identified as Mycobacterium marinum. This atypical mycobacterium is found in fresh or salt water, and is the most common bacterial infection in humans. The lack of clinical suspicion, combined with other factors such as that the mycobacterium mimicry of other conditions and the sporotrichosis characteristics of the lesions, have frequently caused a delay in diagnosis and treatment, as well as misdiagnoses. We have concluded that the delay in accurate diagnosis and prompt treatment, was related to the clinical mismanagement and lack of clinical skill by the physicians and specialists who treated this patient prior to his self-referral to a skilled infectious disease specialist.
Keywords: mycobacterium marinum, atypical, freshwater, saltwater, abscess, skin infection, sporotrichosis, granuloma
The patient developed a lesion on his right hand after sustaining an abrasion while he cleaned his boat, which progressed to formation of other lesions that spread proximally on his right arm and resulted in an abscess to his right elbow. In this case report, we will discuss the patient’s history and clinical assessment, the timeline, the clinical course and interventions, and the epidemiology of the Mycobacterium marinum (M. marinum). Also discussed will be the consequences for this patient related to both the delayed accurate diagnosis and correct treatment, and inappropriate diagnoses and treatment recommendations.
Epidemiology
M. marinum has no known ethnic, gender, or age predilection, and infection most often occurs in individuals exposed, via occupational and recreational methods, to either fresh or salt water.1 Although reported cases of M. marinum are rare in the United States and worldwide, this mycobacterium has been well described in the literature. M. marinum is a slow-growth, nontuberculous mycobacteria, which is found in aquatic environments and is known to cause cutaneous disease when there has been exposure to that environment water (e.g., contaminated fish tank) when there is an abrasion or minor laceration present. Eighty-four percent of 63 cases from France were linked to fish tank exposure. “A similar epidemiologic pattern has been found in the United States, along with the recognition that M. marinum may cause a positive tuberculin skin test”.2 Septic arthritis and osteomyelitis were diagnosed in a 65 -year-old woman who had presented with edema and pain of a distal phalanx after having sustained a puncture wound. Synovial biopsy subsequently revealed M. marinum.2
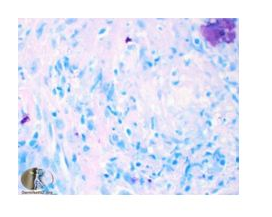
To date, there are 4 known species of atypical mycobacteria that cause skin infections: M. marinum, M. ulcerans, M. fortuitum, and M. chelonae. The clinical features, though, differ. There are two distinct strains of M. marinum. A study was conducted to determine the differences in pathogenicity of the two strains of M. marinum, in which the strains had been used to infect zebra fish (Danio rerio species).3 The mycobacterium was subsequently obtained. The diagnosis of an acute or a chronic disease in the fish was based on the strain recovered. Unrestrained proliferation and death within ~ 16 days for all of the fish categorized as having had the acute disease was noted, whereas the chronic disease was categorized when the survival of the fish was at least 4 to 8 weeks and organ formation of granuloma was present. The two strains were separated in two clusters. The strains in cluster I obtained from humans with fish tank granuloma were noted to cause acute disease, while cluster II strains found in poikilothermic species were associated with chronic disease. The virulence of cluster I was found to be more pathogenic to humans. “This difference in virulence was also observed in vitro: Cluster I isolate Mma20 was able to infect and survive more efficiently in the human macrophage THP-1 and the carp leukocyte CLC cell lines than was the cluster II isolate Mma11. We conclude that strain characteristics play an important role in the pathogenicity of M marinum.”.3 J.C. was infected with the cluster II type. He, therefore suffered from the chronic disease strain of M marinum. No stains results were available for this case study. Below are liver tissue stains for M. marinum (Figure 1).4
The probable pathway of mycobacterial granuloma formation was reported. Upon initiation of mycobacterial protein ESAT-6, epithelial cells secrete matrix metalloproteinase 9 (MMP9) when becoming in contact with infected macrophages, which in turn recruited naïve macrophages and initiated granuloma maturation and bacterial growth.5 Although nodular lymphangitis has most commonly been associated with sporotrichosis, this diagnosis was ruled out based on the history obtained from the patient. Improvement was noted just after two weeks of treatment, which re- assured the current plan of treatment as the best. Full recovery was anticipated. Effective, alternative therapies have included both radiation therapy and cryotherapy.
Case of J.C
J.C. was a healthy 47-year-old Caucasian male with no prior medical condition or surgery. He was married, and a lawyer by profession. The patient had two adult sons, both of whom he reported as having been healthy. His parents were alive and well, without significant medical conditions. He reported that he has enjoyed life and had often cruised on his boat. He reported that possible infectious contact occurred after having incurred an abrasion on his right hand while he cleaned the toilet bowl of his boat. The initial lesion developed two weeks after this exposure, and more lesions developed proximally in a linear fashion to his right arm, then disintegrated to form crusty sores.
The patient was seen by a variety of physician specialists within a well-known multi-specialty clinic. The dermatological lesions and granulomas, though, were misdiagnosed as possible skin cancer, then compounded by an erroneous referral for surgical intervention. No other interventions were discussed or recommended. Patient became very concerned and reportedly felt compelled to seek care elsewhere, as well as to be evaluated by an infectious disease (ID) specialist. After weeks of clinical evaluations by different specialists, and with no definitive diagnosis, J.C. was evaluated by an ID provider who, based on the history gathered from the patient and the physical examination, suspected the etiology of this infection was M. marinum. New lesions were now present on his hand and had also ascended linearly to his right arm, where an abscess on his right elbow has formed. The prognosis, with appropriate treatment, was excellent. Within two weeks after treatment began, various stages of granuloma resolution were observed (Table 1).
Weekend of 1/10 |
Weekend of 1/24 |
First Week of |
Second Week of |
2/15 |
2/29 |
Toilet bowl in |
Appeared at |
Nodular |
Multiple |
Infectious |
Visit. |
Table 1 Timeline
The M. marinum diagnosis was confirmed via histological examination and Lowenstein-Jensen agar culture. Prescribed was a treatment course with oral clarithromycin, to be continued for a minimum of three months. There was clinical improvement noted as early as after antibiotic initiation. The lesions were in various stages of healing. The right elbow abscess required surgical intervention, and was incised and drained. An antiseptic soap (chlorhexidine) body wash prior to surgery was performed by the patient. As a preventive measure, Bacitracin was also prescribed for topical application to the abscess prior to the procedure. Bacitracin is an antibiotic, and dependent upon the concentration, has either bacteriostatic or bacteriocidal properties.6
Clinical findings
At his initial ID examination, his vital signs were within normal range: Temperature, 98.9˚F; pulse rate. 87 beats per minute; respiratory rate, 20 breaths per minute; blood pressure 130/70 mmHg; oxygen saturation by pulse oximetry, 97%. Physical examination revealed a well-nourished, well-dressed, pleasant, Caucasian male who was alert and oriented, had a congruent affect, was in no acute distress, and with a chief complaint of right elbow discomfort. He denied having had, or currently, having, any fever, shortness of breath, nausea, vomiting, or diarrhea.
Extremities: No cyanosis, clubbing, or edema; sensation present in all four extremities with no focal deficits.
Musculoskeletal: Good muscle tone in all extremities, equal bilaterally, but with decreased range of motion of the right arm as secondary to discomfort at the elbow.
Integumentary: Right arm with crusty sores from right hand ascending proximally in a linear fashion to an abscess at the right elbow.
Review of systems except for noted findings, was otherwise unremarkable.
Diagnostic assessment
For diagnostic testing, a small sample of one of the patient’s skin ulcers was obtained and sent for histopathologic analysis; the granulomas confirmed the diagnosis of M. marinum. The culture of the lesions also revealed acid-fast bacillivia Ziehl-Neelsen Figure 2 and Fite stains acid-fast preparations. “M. marinum is a nonmotile acid-fast bacillus (AFB) that grows in 2-3 weeks, with optimum growth on Lowenstein-Jensen medium at 30˚C”.7
The lesion presentation was also characteristic of sporotrichosis, which perhaps led to the incorrect diagnosis from the prior physician specialists, and their subsequent unnecessary referral to a surgeon for surgical intervention, but also contributed to the delay in accurate diagnosis and treatment by a qualified provider.1 A diagnosis of M. marinum can be formulated by a skilled provider from the history and the clinical findings.8
Antimicrobial therapy has been the mainstay of treatment in M. marinum. Pharmacologic therapy consisted of an oral antibiotic, in this case clarithromycin 500 mg orally, b.i.d., the course of treatment was designated as having a minimum of 3 months’ duration. Ethambutol has been considered, and has been deferred until receipt of the sensitivity result and if there has been no clinical improvement within two weeks. M marinum is resistant to standard antituberculosis agents. Therefore, “the use of isoniazid, streptomycin and pyrazinamide as empirical treatment options should be avoided”.9 The patient’s entire body was disinfected with the antiseptic solution (chlorhexidine) as recommended. Education was provided to the patient on the topic of atypical mycobacterium infections, and appropriate precautions were emphasized. The patient was also advised to preventatively wear gloves at all time while cleaning his boat and to immediately cleanse the skin and apply an antibacterial preparation, then bandage the affected area, should any future cut or abrasion occur.
Bi-weekly follow-up evaluations were recommended during the antibiotic therapy; thereafter, 2- 6 weeks were expected to be implemented. Full recovery without significant sequelae was expected for this patient. Indeed, within 2 weeks of treatment the clinical presentation had already significantly improved. The appropriate identification and prompt treatment of this infection is critical, and typically has an excellent clinical outcome “with no major sequelae”.1
The delayed diagnosis and treatment despite multiple specialist physician encounters could have resulted in the involvement of deeper structures or even systemic sepsis. This patient had already developed bursitis, which is one of the several complications associated with M. marinum cutaneous infection. “M marinum infections are usually localized and typically do not spread past the skin in healthy people. ... undetected or untreated, the infection may progress and cause deeper and more longstanding infections. ...tenosynovitis, [and arthritis…”.10 Systemic or deeper tissue involvement with M. mycobacterium can result in osteomyelitis, tenosynovitis, septic arthritis, along with the presented condition of bursitis. The ascending lesions (nodular lymphangitis) have the potential to result in complications such as cellulitis, bacteremia, sepsis, and abscess.11
An appropriate course of oral antibiotic therapy and frequent follow-up evaluations with an infectious disease provider should have a positive outcome of complete eradication of the mycobacterium, which was anticipated in the case of J.C. Surgical debridement may also be indicated, which is dependent on the clinical presentation and course of the disease.6 Having knowledge of the clinical presentations of atypical mycobacteria, especially those inherent to the region in which one practices, and gathering the information for a detailed history are essential, and enable both the prevention of a delay in treatment and the reduction of potential misdiagnoses and the unwarranted and costly referrals and interventions. Equally important is the utilization of diagnostic testing to identify the bacterium. On the horizon is the widespread availability of laboratory diagnostic testing and clinical treatment application that utilize mycobacteriophages, a tool currently undergoing refinement, that reportedly “rapidly identifies the specific species in mycobacterial infections”.1 Any case presentation that has a history of possible exposure to contaminated water and presents with poor- healing wounds despite treatment, should always include the differential diagnosis of M. marinum.
None.
The author declares no conflict of interest.

©2016 Ferdinand, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.