eISSN: 2576-4470


Research Article Volume 9 Issue 1
Affiliation Lecturer, Faculty of Humanities & Social Sciences, Department of Social Sciences, Chuka University, Kenya
Correspondence: Affiliation Lecturer, Faculty of Humanities & Social Sciences, Department of Social Sciences, Chuka University, Kenya
Received: January 11, 2025 | Published: January 24, 2025
Citation: Kiswili JK. Understanding the Covid-19 vaccine uptake in Kenya: knowledge, myths, misconceptions and attitudes.Soc Int J. 2025;9(1):15-21. DOI: 10.15406/sij.2025.09.00409
The Covid-19 pandemic was one of the most devastating health pandemics in recent times disrupting the economic and social lives of billions of individuals across the globe. Study Objectives: The study sought to
Methods: A sample size of 300 was drawn through systematic sampling from a database of 650 online contacts. A semi-structures online questionnaire was used to collect data. Quantitative data was analyzed using SPSS and qualitative Data coded for thematic and content analysis.
Results: Only 250 full-filled questionnaires were returned representing an 83% response rate. This represented 128 males (51.2%) and 122 females (49.8%) drawn from different counties in Kenya. Findings from the study show that majority of Kenyans were knowledgeable about the Covid-19 vaccine(s). The study also established that Kenyans have different myths and misconceptions and social Media outlets are the biggest transmitters of negative information on the vaccine. Lastly, the study established that these myths and misconceptions have a big impact on vaccine uptake.
Discussion: The findings from this study an in tandem with other studies carried out in different parts of the world and more recently in Kenya that shows Vaccine refusal or hesitancy remains a major problem for health interventions in the face of deadly pandemics. However, there is still opportunity for policy makers to come up with clear communication on the benefits of such interventions.
Keywords: covid-19 vaccine(s), knowledge, myths and misconceptions, vaccine uptake, Kenya
Covid-19 hit the globe in December 2019 and, since then the pandemic has continued to ravage the world with devastating consequences. As of April 13th, 2021, the number of Covid-19 cases which had been reported according to the World Health Organization3 was 136,115,434 including 2,936,916 deaths.1 This comes against a background of sustained efforts to curb the spread of the virus through instituting an array of non-pharmaceutical interventions such as social distancing, mask wearing; sanitizing and hand washing, and, in some cases severe measures such as partial or total lockdowns. Despite all these efforts, the number of new cases seems to keep rising with more hospitalizations and fatalities. This has led to an acknowledgment within the health care and policy circles that the long-term success of the public health response to Covid-19 will largely depend on acquired immunity in a sufficient proportion of the population.2 which is estimated to be 67% for COVID-19. However, attaining this kind of immunity through natural means across the global population will translate to millions of deaths on top of putting a tremendous strain on the already stretched health resources.2 Widespread vaccination, therefore, remains the most efficacious strategy for managing the spread of Covid-19, although there is no clear indication on the degree and duration that these vaccines will offer.3
Vaccine refusal and hesitancy
In a bid to counter the spread of the pandemic, various efforts were put in place develop a vaccine and this culminated in one of the most ambitious vaccination program in medical history. While this was a promising outcome, studies done in the post-pandemic period found different levels of vaccine acceptability in various countries. For instance, an April 2020 study found out 26% of adults across seven European countries including the UK were unsure or unwilling to get a COVID-19 vaccine when available.4 Other studies have found that around a quarter of the French.5 and US adult population.6 do not intend to receive the vaccine even if offered it. Vaccines are widely accepted medical interventions by health authorities and the medical fraternity as a major tool for achieving public health successes such as the eradication of smallpox.7 Despite their potency for eradicating potentially deadly health pandemics, vaccines are not readily embraced by members of society whole-heartedly. For many individuals, the doubts about vaccines rotate around their perceived benefits and safety, and whether there is any value in their uptake which ultimately leads to what is referred to as vaccine hesitancy in health policy. There is a need to differentiate between vaccine hesitancy and refusal; the former refers to a situation whereby some individuals owing to some perceived doubts over a vaccine may defer its uptake while the latter refers to a situation whereby some individuals owing to the same reasons completely refuses to consume of the vaccine. In 2015, the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization defined vaccine hesitancy as a 'delay in acceptance or refusal of vaccination despite the availability of vaccination services'.8
Several studies done over the years have shown that the twin problems of vaccine hesitancy and refusal are found in both advanced and developing nations. For instance, a UK study of 14,578 children found that three-quarters of parents whose children were not vaccinated with MMR made a conscious decision to not vaccinate (Pearce et al., 2008). Another notable example in Africa was the polio vaccine boycott in Nigeria in the period 2003–2004 which, significantly pushed up incidence and also contributed to polio outbreaks in three continents.9 Vaccine hesitancy has been singled out as one of the most significant barriers towards achieving herd immunity among communities thereby predisposing individuals to possibilities of an outbreak should a vaccine-preventable organism start circulating in the same communities.10 Due to this, vaccine hesitancy has been identified by the World Health Organization as a top health priority issue (WHO, 2014).
Vaccine hesitancy and refusal are not new phenomena. It is a medical challenge affecting both underdeveloped and developing nations. Consequently, these twin issues have been singled out, as one of the most significant barriers towards achieving herd immunity among communities thereby predisposing individuals to possibilities of an outbreak should a vaccine-preventable organism start circulating in the same communities.10 Due to this, vaccine hesitancy has been identified by the World Health Organization as a top health priority issue (WHO, 2014).
Studies done across the world have reinforced the idea that vaccine hesitancy and refusal and refusal are not isolated cases unique to certain regions of the world, but rather are rampant health challenges spread equally across the globe. For instance, available studies in Austria suggest around 1-11% of parents refuse vaccination, while many more are hesitant and consider refraining from some but not all of the recommended vaccinations.11 A national survey done in Italy in 2016 found out that 83.7% of parents were pro-vaccine, 15.6% vaccine-hesitant, and 0.7% anti-vaccine. Safety concerns were cited as the main reason for refusing (38.1%) or interrupting (42.4%) vaccination.12 Another notable example in Africa was the polio vaccine boycott in Nigeria in the period 2003–2004 which, significantly pushed up incidence and contributed to polio outbreaks in three continents.9
A systematic review of Covid-19 vaccine acceptance globally undertaken in December 2020 yielded interesting results. In this particular review, a systematic search of the peer-reviewed English survey literature indexed in PubMed was done. Overall, results from 31 peer-reviewed published studies met the inclusion criteria and formed the basis for the final COVID-19 vaccine acceptance estimates. Survey studies on COVID-19 vaccine acceptance rates were found from 33 different countries. Among adults representing the general public, the highest COVID-19 vaccine acceptance rates were found in Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%), and China (91.3%). However, the lowest COVID-19 vaccine acceptance rates were found in Kuwait (23.6%), Jordan (28.4%), Italy (53.7), Russia (54.9%), Poland (56.3%), US (56.9%), and France (58.9%).
A study done in China in 2021 found out that 67.1% of the participants were reportedly willing to accept the COVID-19 vaccination, while 9.0% refused it. 834 of the participants accounting for (35.5%) reported vaccine hesitancy. According to the study, the current coverage was 34.4%, which was far from reaching the requirements of herd immunity. The predicted rate of COVID-19 vaccination was 64.9%, 68.9%, and 81.1% based on the rates of vaccine hesitancy, willingness, and refusal, respectively.13
Longitudinal studies in the United States have shown the tendency for vaccine refusal to decline over time.14 However, no longitudinal study has been carried out in low income countries to measure the same. Likewise, there are very few studies done in Kenya to document the factors and rates of vaccination refusal (Anyiam-Osigwe T,2021, Kyobutungi C.2021, Dyer O). However, a recent study in four Kenyan counties using cross-sectional data from February 2021 found that 60 % of respondents were vaccination hesitant and identified factors associated with vaccination refusal including older age, lower education, not adhering to COVID-19 mitigation strategies, and concerns with the safety and effectiveness of the vaccine (Anyiam-Osigwe T,2021). This study found that COVID vaccination refusal has decreased dramatically over the course of 2021 in Kenya, from 24 % in February 2021 to 9 % in October 2021. This suggests some degree of success on the part of the Kenyan Government, as well as confirmation that several temporal factors address vaccination refusal over time. However, despite the significant drop in vaccination refusal in Kenya, the country’s full vaccination rate remained below 10 % at the end of 2021.
Theoretical framework for the study
This study can be approached by using the Protection Motivation Theory (PMT) that was propagated by Rogers in 1975, to explain the motivations for individuals to act in ways geared towards self-protection in the face of a perceived health threat. This theory posits that human beings will more often than not engage in protective behavior(s) that ultimately minimizes the impact(s) from perceived threats. The Protection Motivation Theory (PMT) tries to explain how individuals make decisions and take actions especially when they perceive their health to be in jeopardy.15 For instance, how would one react if they believed that their health is at risk because of obesity?
PMT argues that individuals will usually decide on whether to engage in a health-related behavior(s) through two processes; threat and coping appraisals. The former is related to the level of threat as perceived by an individual. In this process, an individual actor will replay the various predisposing factors to the threat and appropriately choose behavior(s) that may reduce harm. The twin concepts of perceived vulnerability and perceived severity are very instrumental to an individual's decision-making process under this appraisal. Perceived vulnerability is the belief that he/she is susceptible to a disease that is potentially a health threat. Perceived severity, on the other hand, is that feeling in an individual that the health threat will have devastating consequences. The amount of fear generated by the two sets of situations determines how individuals react to any perceived health threat. Coping appraisal deals with how an individual evaluates the different factors that may ultimately push him/her to pursue a preventive response. This appraisal works on three sets of beliefs; response efficacy, the belief that engaging in a certain behavior is desirable for lessening the threat; self-efficacy, the belief that one has the requisite capabilities to engage in the desired behavior and lastly the perceived-response costs that deal with the costs that accrue from engaging in a specific behavior.15
PMT is not difficult to apply in explaining individuals’ inclination to be vaccinated in the face of the Covid-19 onslaught. Individuals will most likely engage in the practice if they believe that they are sufficiently susceptible to the virus and that contracting it will potentially prove harmful to their health. They will also most likely agree to be vaccinated if they are convinced that it will reduce the threat of infection. They are also likely to be vaccinated if they feel that they are capable and if they feel that the advantages of engaging in the practice outweigh the disadvantages. Therefore, for this study, the rate of vaccination uptake as a Covid-19 mitigation practice represents the threat appraisal which signifies a call to action based on the perceived threat; the barriers to adoption represents the capacity to engage in the practice and the perceived implications of the opportunity cost of engaging in the behavior.
Problem statement
Kenya has not been spared the ravages of Covid-19. As of 13th April 2021, Kenya's caseload according to the WHO dashboard stood at 145,670 confirmed cases of COVID-19 with 2,348 deaths (WHO, April 2020). This is despite the raft of measures that the president of Kenya, Uhuru Kenyatta instituted after the onset of the third wave of the pandemic which even the most skeptical observers felt was much more deadly than the previous two waves. Among the measures which were put in place including the cessation of movement out of the four counties of Nairobi, Machakos, Kajiado, and Kiambu; stoppage of in-person instruction in all institutions of learning; restricted numbers for social gatherings such as religious functions and burials; closure of bars and restaurants and a national curfew which commences at eight o’clock every night.
Kenya like all other nations has embarked on a vaccination drive to stem the spread of the virus. According to an article in the Conversation journal, Kenya received its first batch of 1.02 doses of Astra Zeneca Vaccine on the 3rd of March 2021. This batch came through the Global COVAX initiative, which aspires to provide equal access to COVID-19 vaccines. The initial beneficiaries for this first phase of vaccination were high priority groups such as frontline workers in health care, education, and the security forces but two weeks after roll-out the target group was expanded to include individuals aged over 58 years and those persons living with co-morbidities. Two weeks after the vaccination roll-out only 280,000 Kenyans had received the jab, which was considered low relative to the targets the government had set.16
One of the greatest challenges since roll-out has been hesitancy towards vaccination that was first manifested by a section of health workers. This is not unique to Kenya, as there have been fears and suspicion in Africa and other parts of the world around the AstraZeneca vaccine after reports of blood clotting started merging after vaccination. Unfortunately, AstraZeneca is the only official vaccine being administered in Kenya. The Kenyan Government was well aware of a growing hesitancy towards the Covid-19 vaccine even before the roll-out but there were no concerted efforts to stem off the skepticism. This has led to very slow uptake of the vaccine by the target groups
Objectives of the study
Against all this background, this study sought to establish the level of knowledge as well as documenting the myths and misconceptions around Covid-19 vaccine(s) among Kenyans. Further, the study sought to find out if such myths and misconceptions have affected people's attitudes and ultimately influenced their willingness to participate in the ongoing vaccination drive.
The study, therefore, was guided by the following objectives and research questions,
Rationale for the study
Health experts believe that the safest way to tame the spread of Covid-19 is the realization of herd immunity among the world's population. There was also a consensus that the only safest way to achieve this is through mass vaccination. This study therefore will shed some light on the myths and misconceptions that Kenyans have developed towards the Covid-19 vaccines and how these influence uptake. Ultimately, such insights would be invaluable to policymakers in drafting measures to circumvent cases of vaccine hesitancy and rejection among the populace.
Research design
This study used a cross-sectional design simply defined as a type of research design in which you collect data from many different individuals at a single point in time. In cross-sectional research, the researcher observes variables without influencing them. This research design was deemed appropriate for the study because the researcher wanted to capture the views of the respondents at the same time without influencing any of the variables under study. Overall, the study used a triangulation of both quantitative and qualitative research methodologies.
Sampling and data collection tools
The restrictions imposed for Covid-19 in the country were limiting factors when it came to the sample size and data collection. The study, therefore, taking cognizance of all these limitations, targeted a sample size of 300 respondents drawn randomly from a database of 650 WhatsApp contacts. The 300 respondents were drawn using systematic sampling method with a sampling interval of 2, i.e 650/300=2.2(rounded off to 2). An online self-administered semi-structured questionnaire was employed to collect data for the study.
Data handling and analysis
Incoming data was captured on an online template. The first step was to clean all the incoming data. Qualitative data were coded and subjected to thematic analysis using NVivo. Quantitative data on the other hand was input into SPSS for descriptive statistics (Table 1). This indicates that the majority of those who participated in the study were young people under 30 years of age. Respondents’ demographics such as sex and age and are important variables when interrogating an individual’s attitudes and behavior patterns.
|
Total (250) |
Percentage |
|
|
Gender |
||
|
Males |
128 |
41.9 |
|
Females |
122 |
|
|
Level of Education |
||
|
Secondary school leavers |
6 |
2.4 |
|
Diploma |
45 |
18 |
|
First degree holders |
135 |
54 |
|
Masters |
50 |
20 |
|
PhDs |
14 |
5.6 |
|
Age variation |
||
|
Median |
25 Years |
|
|
Mode |
20 Years |
|
|
Mean age |
30.34 years |
|
|
Standard Deviation |
10.88 |
Table 1 Respondents’ demographics
Respondents’ county of residence at the time of the study
The respondents in this study were drawn across 26 out of Kenya’s 47 counties with Nairobi having 85 participants accounting for (33.6%); Tharaka Nithi 30 (12%); Machakos 17 (6.8%); Makueni 13 (5.2%); Kiambu 11 (4.4%); Nakuru 9 (3.6%); Kajiado 8 (3.2%); Mombasa 7 (2.8%); Meru 6 (2.4%); Kitui 5 (2%); Kilifi 4 (1.6%); Embu 4 (1.6%); Kirinyaga 3 (1.2%); Nandi 3(1.2%); Laikipia 3(1.2%); Nyeri 3 (1.2%); Kisumu 3 (1.2%); Uasin Gishu 3 (1.2%); Homabay 2 (0.8%); Kakamega 2 (0.8%) ;Kisii 2 (0.8%); Muranga 2 (0.8%); Bungoma 2 (0.8%);Nyandarua 2 (0.8%); Trans Nzoia 1(0.4%); Baringo 1 (0.4%); Narok 1 (0.4%); Migori 1 (0.4); Kwale 1 (0.4); Kericho 1 (0.4) and Samburu 1 (0.4) (Graph 1).
This indicates that the majority of those who participated in the study were young people under 30 years of age. Respondents’ demographics such as sex and age and are important variables when interrogating an individual’s attitudes and behavior patterns.
4.5 Respondents’ knowledge about the ongoing Covid-19 vaccination program in Kenya and the vaccines being administered
The respondents in this study were drawn across 26 out of Kenya’s 47 counties with Nairobi having 85 participants accounting for (33.6%); Tharaka Nithi 30 (12%); Machakos 17 (6.8%); Makueni 13 (5.2%); Kiambu 11 (4.4%); Nakuru 9 (3.6%); Kajiado 8 (3.2%); Mombasa 7 (2.8%); Meru 6 (2.4%); Kitui 5 (2%); Kilifi 4 (1.6%); Embu 4 (1.6%); Kirinyaga 3 (1.2%); Nandi 3(1.2%); Laikipia 3(1.2%); Nyeri 3 (1.2%); Kisumu 3 (1.2%); Uasin Gishu 3 (1.2%); Homabay 2 (0.8%); Kakamega 2 (0.8%) ;Kisii 2 (0.8%); Muranga 2 (0.8%); Bungoma 2 (0.8%);Nyandarua 2 (0.8%); Trans Nzoia 1(0.4%); Baringo 1 (0.4%); Narok 1 (0.4%); Migori 1 (0.4); Kwale 1 (0.4); Kericho 1 (0.4) and Samburu 1 (0.4) (Graph 2).
From the above responses, it is quite evident that majority of the respondents are very much aware of the Covid-19 vaccine that is being administered in Kenya to fight the pandemic. The Oxford-AstraZeneca has been the official Covid-19 vaccine the Kenyan government has rolled out in its vaccination drive. Though some doses of the Russian manufactured Sputnik V vaccine found their way into the country, the government categorically refused its usage. Based on these facts, it is still interesting to note that some of the respondents still listed vaccines such as Mordena, Sinovac, Jansen, and EpivacCorona as being officially used in the country’s Covid-19 vaccination campaign.17
4.6 Sources of information on the Covid-19 vaccination program
It is important to establish the sources of medical information, especially during health emergencies. This is because the information people receive has a big bearing on their decision-making process when it comes to the utilization of critical health interventions. The success of health interventions rests on an effective communication strategy.18 That being the case, this study sought to find out the sources of information regarding the Covid-19 vaccination program in the country. Graph 3 below summarizes the different sources of information on the subject (Graph 3). Due to the regulatory frameworks under which they operate, mainstream communication sources like television, radio, and newspapers are likely to transmit credible information as opposed to other sources such as social media that do not have any inherent regulatory mechanisms. Policy makers and official health communication agencies should be worried by the fact that a majority of the respondents singled out social media as their major source of information on the Covid-19 vaccination campaign.19 This is because Social media has been known to post unaudited content that can pose a grave danger in the consumption of vital health interventions. For instance, a study done in the USA found out that vaccine-hesitant individuals are more likely to identify social media as their sole source of information. This is because of the potency of social media to successfully mount intentional anti-vaccination disinformation campaigns.20
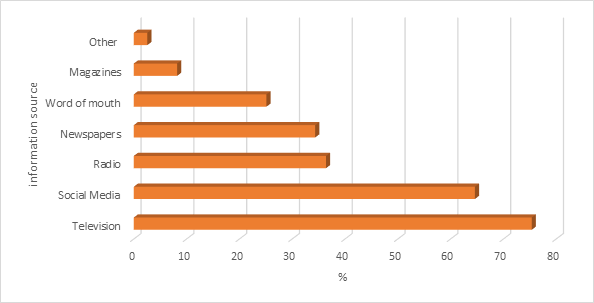
Graph 3 Television is the leading medium followed closely by social media, radio, Newspapers, Verbal, magazines, and other unspecified sources.
Respondents’ knowledge on vaccines (how they work and the need for vaccination)
It should be noted that this particular theme of the study was not in any meant to measure the respondents' technical knowledge of vaccines but rather their basic understanding of the subject. This is because proper knowledge on the subject is ultimately important in people’s decision to get vaccinated. Overall, it is safe to note that the majority of the respondents exhibited a fair knowledge of the general working of vaccines on the human body. Since this was an open-headed question, it yielded qualitative data but the key theme that emerged is that vaccines work towards boosting human body immunity. Other words that were commonly used to describe the purpose of being vaccinated were “strengthening”, “building” and “increasing” immunity.
Myths, misconceptions, and attitudes about the Covid-19 vaccine (s)
The second objective of this study was to find out the various myths, misconceptions, and attitudes respondents harbored around the Covid-19 vaccine. 220, (88%) of the respondents reported that they had received negative information about the Covid-19 vaccine. They were presented with a list of eleven myths and misconceptions on the Covid-19 vaccine and the responses are captured in the following table (Table 2). From the above table, it is apparent that there is a lot of myths and misconceptions around the covid-19 vaccine. It was also important to establish the sources of these myths and misconceptions and what came out was that Social media outlets (WhatsApp, Facebook, etc.) was the leading source of information accounting for 70.26%; word of mouth 44/1%; television 18.46%; radio 8.72%; Newspapers 7.18% and magazines 2.05%. This again shows the power of social media in transmitting vital information about the Covid-19 vaccine. As discussed earlier in the paper, social media has a lot of potency in influencing consumers' perceptions about health interventions that consequently affects their uptake for the same. As pointed earlier, due to the lack of a regulatory framework to filter content, social media renders itself to abuse whereby unreliable information is transmitted to a large audience within a very short period.
|
Myth/Misconception |
Frequency |
Percentage (%) |
|
The COVID-19 vaccine has severe side effects such as allergic reactions |
124 |
63.59 |
|
The COVID-19 vaccine is unsafe because it was developed so quickly. |
79 |
40.51 |
|
The COVID-19 vaccine will alter my DNA. |
41 |
21.03 |
|
The COVID-19 vaccine causes infertility in women. |
38 |
19.49 |
|
You can get COVID-19 from the vaccine |
35 |
17.95 |
|
Once I receive the COVID-19 vaccine, I no longer need to wear a mask. |
25 |
12.82 |
|
I have already been diagnosed with COVID-19, so I do not need to receive the vaccine. |
21 |
10.77 |
|
I am not at risk for severe complications of COVID-19 so I do not need the vaccine. |
21 |
10.77 |
|
The COVID-19 vaccine includes a tracking device. |
21 |
10.77 |
|
If I receive the COVID-19 vaccine, I am at a greater risk to become sick from another illness. |
21 |
10.77 |
|
Certain blood types have less severe COVID-19 infections, so getting a vaccine is not necessary. |
20 |
10.26 |
Table 2 Myths, misconceptions, and attitudes about the Covid-19 vaccine (s)
The respondents were asked whether they believed the negative information they were receiving about the Covid-19 vaccines and 165 representing 66% of the total sample size said they did not while the rest 85 (34%) reported they did. Statistically, 34% of the sample reporting that they believe in these myths and misconceptions is a little bit worrying because if this were to be generalized to the general population, then the number of people believing in the same would be quite high. This has serious implications on the uptake of the vaccine.
4.9 Implications of the myths and misconceptions on vaccine uptake
The third objective of this study was to establish if the myths and misconceptions individuals had received about the Covid-19 vaccine(s) would pose any threat to the uptake of vaccination. 156 (62%) of the respondents agreed that it would while the remainder 94 (38%) said that it would not. Even though a significant percentage of the respondents (66%) had said they did not believe in the negative information they had received on the Covid-19 vaccine(s), it should be worth noting that the percentage of those who believe that this would have an impact on vaccine uptake has gone up. This presents a startling contradiction that might interest policymakers and agencies tasked with the responsibility of rolling out the vaccine program.
As a way of confirming whether indeed these myths and misconceptions had an impact on vaccine uptake, the respondents were asked to state their willingness to participate in the vaccination drive. Out of the 250 participants, only 32, a paltry 12.8% had been vaccinated at the time of the study. Out of the rest (218) who had not yet been vaccinated, when asked if given an opportunity if they would, only 107 answered in the affirmative; 65 said they would not while 46 said they were not sure (Table 3).
|
Vaccination Status |
Total (250) |
Percentage (%) |
|
Vaccinated |
32 |
12.8 |
|
Not vaccinated |
218 |
88.2 |
|
Willing to be vaccinated (not Vaccinated at the time of the study) |
-218 |
|
|
Yes |
107 |
49.08 |
|
No |
65 |
29.81 |
|
Not Sure |
46 |
21.1 |
Table 3 Respondents vaccination status at the point of the study
The reasons for those refusing to get vaccinated and not those not sure revolved around the same myths and misconceptions captured in table 1 above. Below is a verbatim paraphrase of some of the responses.
“I don't think it is necessary if am perfectly healthy and fine”, “Still waiting to see the effects as above”
“Until the controversial statements about these vaccines fade it is when I will go for it”
“Still gauging the effectiveness of the vaccine”
“Side effects scare”
“I'm skeptical of the vaccine”
Therefore, it can be fairly deduced that fears related to the vaccine account for the main reason why most of the participants were reluctant to be vaccinated. The number of respondents not willing to be vaccinated and that not sure accounted for almost 44.4% of the total sample size, which in itself should be worrying from a public health perspective.
Respondents’ views on whether the government has effectively and adequately managed the flow of information on the Covid-19 vaccination
Opinion was divided almost equally on this matter with 124 (49.6%) reporting that the government had done a good job of relaying information about the vaccine while 126 (50.4%) felt that the government had not done a good job on the issue. This should be an area of concern when half of the participants in the study feel that the government has not handled the transmission of information on such a serious health intervention in an effective and timely manner. The success of any government public health initiative relies heavily on a good communication strategy. There is a mountain of evidence on the impact of proper communication on the efficacy of public health interventions. It is widely acknowledged that to promote and sustain healthy behavior, communication is very important. An effective health communication strategy serves an array of functions; it creates awareness on an existing health challenge and the solutions available to counteract it; it equips individuals and groups with knowledge, skills, and capacity to deal with health challenges.21
While it is worth noting that the sample size for this study is too small for generalization, it is nonetheless important to point out the study has come up with very illuminating insights on the state of the Covid-19 vaccination program in Kenya. One of the most positive outcomes is that there is a very high level of awareness of the vaccination program (including the vaccine on offer). This level of awareness is good for the country because it shows people are keenly following the vaccination narrative. Another positive finding out of the study is that almost half of the participants are willing to be vaccinated given the chance. Though this number is low, it is still a good starting point and the government should put in place a good communication strategy that promotes citizen enthusiasm on the Covid-19 vaccination program.
On a negative note, the study has established that there exists a lot of myths and misconceptions around the Covid-19 vaccine. Social media is responsible for spreading most of this erroneous information about the vaccine. The drawback of this is that majority of the participants feel that these myths and misconceptions will have a big bearing on vaccine uptake. It is imperative to counteract this fallacious information by putting together a well-coordinated and elaborate communication strategy that among other things provides adequate and timely accurate information about the vaccination program.22
Citizens' willingness to partake in any health intervention rests on three fundamental considerations; one is the perceived benefits accruing from embracing the intervention; two is the cost of partaking in the intervention and lastly is the level of credibility/ legitimacy of the intervention. The government has the responsibility of ensuring that these three considerations do not become barriers especially in the uptake of the Covid-19 vaccine. Vaccine hesitancy and refusal as noted in earlier discussion in this paper is not a new phenomenon. In addition, it is not endemic to only poor nations of the world. This phenomenon has been classified a medical threat by the World Health Organization. If not well managed, it can pose serious challenges to the global efforts to turn the tide against the Covid-19 pandemic. The Kenya government should commission a national survey to find out the levels of Covid-19 hesitancy and refusal and the factors responsible for the same. This will go a long way in the formulation of a persuasive and evidence-based response strategy to counter the twin challenges that may prove devastating to the country’s push towards herd immunity for the population. This study though having some methodological limitations offers useful insights that can be utilized by policy makers in the health sector to tailor vaccination programs to have the best efficacy.
None.
There is no conflicts of interest.

©2025 Kiswili. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.