eISSN: 2377-4304


Research Article Volume 1 Issue 2
1Department of Obstetrics and Gynecology, Hofstra University School of Medicine, USA
2Division of Radiology, Hofstra University School of Medicine, USA
Correspondence: Jeffrey Schachar, Division of Urogynecology: Female Pelvic Medicine and Reconstructive Surgery, Department of Obstetrics and Gynecology, North Shore-Long Island, Jewish Health System-Hofstra University Medical School, 865 Northern Blvd. Ste 202, Great Neck, NY 11021, Fax 516-622-5045
Received: November 07, 2014 | Published: November 17, 2014
Citation: Nosseir S, Schachar J, Naidich J, et al. Midpubic line to stage pelvic organ prolapse by MRI defecography as compared to POP-Q. Obstet Gynecol Int J. 2014;1(2):37-41. DOI: 10.15406/ogij.2014.01.00011
Objective: To compare the degree of pelvic organ prolapse (POP) as measured by the pelvic organ prolapse quantification (POP-Q) system to the degree of prolapse as measured by magnetic resonance imaging (MRI) defecography and to merge clinical and radiologic terminology in reference to POP.
Methods: A retrospective analysis of 29 patients who presented with POP and defecatory complaints and underwent MRI defecography (2008-2011). POP-Q scores were recorded by two attending urogynecologists. A radiologist, blinded to the clinical POP-Q scores, measured the maximum prolapse of the anterior vagina, posterior vagina, and vaginal apex/cervix on each subject’s MRI.
Results: Prolapse as measured by MRI defecography was significantly more advanced as compared to the clinical POP-Q measurements in all three compartments studied. The differences were both statistically significant and potentially, clinically relevant. A mean difference of 2.0 centimeters ±1.5SD, 2.3 centimeters ±2.7SD, and 5.0 centimeters±2.0SD was observed in the anterior, apical, and posterior vaginal compartments, respectively.
Conclusions: The increased degree of prolapse as demonstrated by MRI defecography may change clinical decision making and surgical planning. Therefore, MRI defecography may be a valuable adjunct in the clinical assessment of POP.
Keywords: MRI, defecography, pelvic, organ, prolapse, POP-Q
POP, pelvic organ prolapse; POP-Q, pelvic organ prolapse quantification; MRI, magnetic resonance imaging; TR, repetition time; TE, echo time; CI, confidence interval
The pelvic organ prolapse quantification (POP-Q) system is currently the most broadly accepted method of quantifying pelvic organ prolapse (POP).1 However, using magnetic resonance imaging (MRI), investigators have shown that patients who appear to have single compartment prolapse clinically, had multiple compartment defects on MRI. 95% of patients presenting with symptoms in only one vaginal compartment have been shown to have tri-compartment abnormalities on dynamic cystoproctography.2 Therefore, surgical candidates for repair of an apparent single compartment problem are at risk of surgical failure due to underestimation of anatomic deficits. Images obtained during defecation have been shown to improve the identification of additional cases of abnormal bladder, vaginal, and rectal decent.3
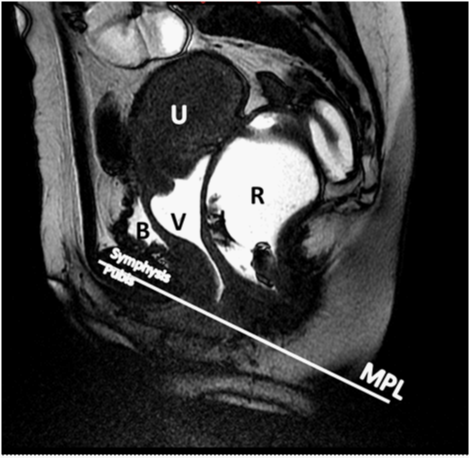
A major obstacle in comparing the POP-Q system to an MRI defecography evaluation is the selection of a reference point available on both MRI and clinical exam. For purposes of this study, we selected the point at which the midpubic line intersects the longitudinal axis of the vagina as the radiologic representation of the hymen (Figure 1).The use of the midpubic line has been described as a landmark for MRI staging of pelvic organ prolapse. Fresh cadaver data has established the midpubic line as a reliable indicator of the clinical hymen, which is the landmark used for clinical scoring.4
Previous studies have shown MRI to demonstrate a more advanced degree of prolapse; however, none have attempted to establish POP-Q equivalent MRI scoring. The merging of clinical and radiological reference points would allow detailed compartmental comparison between clinical and MRI evaluation.
This retrospective study was conducted at North Shore University Hospital. Institutional review board approval was obtained. Thirty-six women presenting for assessment of POP, who required MRI defecography as part of their clinical assessment, constituted the study population. The senior authors examined all patients in the study using the standard guidelines for the POP-Q examination. The clinical exams and MRIs were performed prior to any intent of studying the relationship between MRI and the POP-Q examination.
MRI technique
Patients underwent MRI with a 1.5-T scanner (Signa Excite HDx; GE Healthcare, Milwaukee, WI) with an 8-channel phased array coil in the supine position. Patients administered a fleet enema in the morning and emptied their bladders prior to imaging. 60ml of sterile lubricating jelly (Triad Disposables, Inc, Mukwonago, WI) was instilled into the vagina. 200ml of lubricating ultrasound transmission gel (Aquasonic, Parker Laboratories, Inc, Fairfield, NJ) was instilled into the rectum.
Following an initial three plane localizer sequence, sagittal images were obtained employing a steady-state acquisition (FIESTA=fast imaging employing steady-state acquisition). From this initial sequence, the midsagittal image that optimally displayed maximal prolapse was selected. Dynamic cine FIESTA imaging was performed in the midsagittal plane with the following parameters: TR/TE=3.9/1.7, 24x24cm field of view, 224×192 matrix, 7mm section thickness (TR=repetition time; TE=echo time). This sequence was used to acquire one image per second for 60 seconds. Images were obtained at rest, maximal sphincter contraction, straining, and defecation. This sequence has the advantage of combining high contrast and temporal resolution, which allows the sequence of images to be combined into a moving image (cine loop).
Finally, axial and coronal fast relaxation fast spin echo T2 weighted images were obtained with the following parameters: TR/TE=3700/102, 25 x 25 cm field of view, 384×256 matrix, with 6mm section thickness. These sequences were performed to better visualize the pelvic anatomy and evaluate for muscle defects.
Image assessment
The midline image of the resting and straining sequence of each subject’s MRI was selected by the radiologist. This image was enlarged until the mullerian structures were obscured from view to avoid measurement bias. The radiologist selected representative midsagittal images at rest and images demonstrating maximum prolapse.
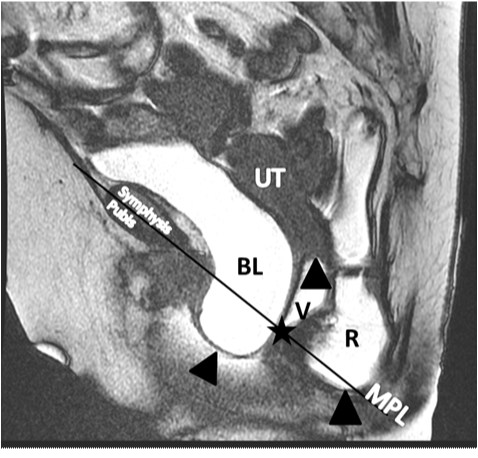
The image sequence was measured for the degree of POP in both static and in cine loop mode. The MRI coordinates of the maximal descent of the anterior, posterior, and apical compartments of the vagina were recorded to compare to the clinically assessed POP-Q points; Ba, Bp, and C, respectively (Figure 2). In the straining sequences, the MRI equivalents of POP-Q points Aa and Ap could not reliably be tracked as the vaginal walls folded on one another and clarity could not be reliably obtained on the straining images for a point precisely three centimeters from the hymen.

The reference lines, axes of measurement, and MRI equivalents of POP-Q points were defined as follows (Figure 1) (Figure 2):
Prolapse of the anterior vaginal wall, cervix or cuff, and posterior vaginal wall was recorded in centimeters by calculating the difference between the coordinates of maximal prolapse and the hymen (Figure 3).
Statistical analysis
The primary objective of the study was to determine whether MRI and POP-Q measurements were in agreement. The primary variable of interest was the difference in measurement between MRI and POP-Q (difference = MRI - POP-Q) for each of Ba, Bp, and C. A positive difference means that the measurement using MRI was greater than POP-Q. A t-based 95% confidence interval (CI) for the difference corresponding to a single measurement of an individual was computed.5 In the current context, average difference is less relevant because the clinical interest is the difference in measurements for individual patients. The sample size of n=29 was based on availability of patients with both MRI and POP-Q data during the period of 2008 to 2011. Since this is an observational study and the first of its kind, a sample size and power calculation was not applicable. Typically, such calculations rely on knowledge of inherent variability in the data and desired effect sizes, neither of which existed.
The interpretation of the results was approached from a confidence interval (“limits of agreement”) perspective. If both the lower and upper limits of agreement were clinically insignificant, then the two methods would be declared “in agreement”. If either of the limits was beyond what would be deemed a clinically acceptable discrepancy, then the two methods would be declared “in disagreement”.
In 7 of the 36 (19.4%) subjects, artifact in the images did not allow measurement of the three desired prolapse points. Folding of vaginal tissues or lack of retention of vaginal or rectal contrast rendered these seven images un-interpretable. For the 29 subjects studied, the mean age was 59.4 years (range 48-83), mean parity was 2.9 (range 1-8), and mean BMI was 26.4 (range 18-35).
For all POP-Q equivalent measurements, MRI assessment of prolapse was greater than the clinical exam. The 95% t-based confidence intervals included values which were clinically relevant in all three compartments. A mean difference of 2.0 centimeters ± 1.5 SD was observed in the anterior vaginal compartment, 2.3 centimeters ±2.7SD in the apical compartment, and the largest mean difference of 5.0 centimeters ±2.0SD in the posterior compartment (Table 1).
POP-Q point |
95% Confidence interval (CI) |
Standard deviation (SD) |
Difference mean (cm) |
Anterior vagina (Ba) |
-6.2 |
1.5 |
2 |
Posterior vagina (Bp) |
0.9–9.1 |
2 |
5 |
Cervix or cuff (C) |
-3.2–7.8 |
2.7 |
2.3 |
Table 1 MRI assessment of prolapse was greater than POP-Q for all POP-Q points studied. The 95% confidence intervals included values which were clinically relevant in all three compartments. PROLAPSE: Agreement between POP-Q and MRI defecography measurements
The POP-Q method is the current standard for assessment of POP1.We hypothesized that MRI defecography would demonstrate a more advanced degree of prolapse than the clinical POP-Q assessment. The comparative data from our study is confirmatory in that the degree of POP in all three compartments was significantly greater when measured by MRI defecography.
Clinical POP-Q assessment is not conducive to demonstrating maximal prolapse. In the office setting, the patient is guarded, fearful of urinating or defecating while straining, and the physiologic tendency to contract the pelvic floor when straining is exacerbated by the presence of an observer. In addition, not all patients fully understand how to valsalva.
The MRI experience for a patient is also far from ideal. However, defecating in an MRI may allow a different level of pelvic relaxation because the patient is intentionally allowing the physiology of defecation to occur.
It is likely, that during defecation there is a certain amount of descent that would be considered normal even in a healthy nulligravid patient such that the pelvic floor may descend more than what would be seen on a clinical exam. This may partially explain the significant difference between the MRI and clinical exam findings. Schreyer et al performed MRI defecography on ten asymptomatic nulligravid volunteers. They found eight patients to have a radiologically defined rectocele, six a cystocele, and three a uterine prolapse.6 It would be difficult to use this study as a control group because they did not perform POP-Q exams and thus, could not correlate radiologic and clinical exam findings. We recommend further study with the use of a control group to confirm the significance of our findings.
An obstacle in comparing the two groups was the selection of a reference point readily available on both MRI and clinical exam. We observed that typically, the direction of organ movement in someone experiencing POP as reported by MRI is not in the same directional plane as what is recorded in a clinical POP-Q system. In the POP-Q system, the axis of measurement is in reference to cephalad or caudal relation to the hymen. In contrast, MRI defecography most commonly reports movement of pelvic organs in reference to the pubococcygeal line (PCL). The PCL extends from the inferior border of the pubic symphysis to the last joint of the coccyx and is intended to represent the level of the pelvic floor in normal subjects. This plane cannot be established on physical exam and thus was not used for purposes of our study. Previous studies have demonstrated that the midpubic line has higher agreement with POP-Q staging than the PCL.7 According to the International Incontinence Society and the original POP-Q publication, the lower edge of the pubic symphysis should be given high priority as a landmark for reporting pelvic organ prolapse to allow comparison to the physical examination.1 Based on existing literature, the midpubic line has the best correlation with the clinical hymen.4 The midpubic line begins from the posterior edge of the pubic symphysis, which is easily palpable on clinical exam and readily apparent on radiologic imaging. Unlike the hymen, the pubic symphysisis fixed in space and is easily identified in both clinical and radiologic examinations. Furthermore, for patients with atrophic changes, the actual hymenal remnants are not readily apparent.
We propose that the intersection of the midpubic line and the longitudinal axis of the vagina be routinely included in radiologic reporting because it enhances the clinical POP-Q examination with radiologic information measured in a similar axis. Our observations suggest this to be superior to measurement of prolapse in relation to the PCL, which tends to be more anterior to posterior in direction and results in radiologists and clinicians taking measurements of movements which are almost at right angles to one another.
According to previous studies, patient positioning, force of valsalva, and bladder distention have been shown to affect the severity of POP.8–12 Our POP-Q exams were performed in the supine position with the patient straining. Some authors report more advanced prolapse when patients are examined in the standing position8. In contrast, a study by Swift et al demonstrated no significant difference in prolapse staging in supine and standing positions.13 In light of this data and our findings, we support further studies to confirm whether MRI defecography in the seated position could preserve the same level of image clarity and allow for a more physiologic set up for elimination and demonstration of maximal prolapse.
A number of prior studies which have also compared MRI assessment of prolapse to the clinical exam similarly highlight the disagreement between clinical and MRI staging of POP. Singh et al previously compared POP as measured by clinical examination to MRI staging using the midpubic line in 20 subjects. There was a 75% correlation between MRI and clinical staging, with over-staging by MRI in 25% of the subjects. It is noteworthy that the terms “under” and “over” staging presume that clinical staging is accurate. We propose that MRI evidence is objective and the clinical assessment was likely “under” staging maximal prolapse in the Singh study. Other studies reported a broad range in the agreement between MRI and clinical prolapse assessment, ranging from 41-85%.14,15 Some studies reported discrepancies between MRI and POP-Q measurements as high as 3, 4, and 5cm for points Ba, C, and Bp, respectively.16
A notable differentiating factor of this study is the utilization of dynamic MRI to measure a patient during the defecation phase. The majority of prior studies measured patients during rest and maximal straining only. According to Flusberg et al, images obtained during the defecation phase improved the identification of additional cases of abnormal bladder descent in 51% of examinations, abnormal vaginal descent in 61% of examinations, and abnormal rectal decent in 13% of examinations.3
The retrospective nature of our study presented some limitations. Seven of our patients’ MRIs were not interpretable. The radiologist asserted that had the goals of measurement been set at MRI execution, nearly all patients would have had interpretable MRIs. Instilling more gel or re-instillation of gel and repeating the defecogram may have converted several patient images to appropriate clarity.
Although dynamic MRI has been used to evaluate POP, there is a lack of shared terminology between the radiology and pelvic surgery disciplines. The terms utilized and anatomic measurements recorded are mutually exclusive. To our knowledge, no attempt had been made prior to this study to merge the methods and terms in order to allow both disciplines to accurately communicate. Creating a common language will serve to improve both diagnosis and surgical planning.
Despite being a relatively small cohort study, the difference between the MRI results and clinical exam measurements achieved statistical significance due to the substantial disparity between the measurements. Hetzer et al.17 noted that findings on MRI defecography led to changes in the surgical approach in 67% of patients who underwent surgery.17 Correctly identifying the severity of defects in all compartments may lead to changes in surgical decision making and improve overall surgical success rates.
In conclusion, the degree of POP as measured by MRI defecography was greater than that reported on clinical POP-Q examination. The differences were quantitatively significant enough to warrant considering implementing changes to clinical decision making and surgical treatment plans. Therefore, we suggest that MRI defecography may be a valuable adjunct to the clinical POP-Q examination even in the absence of defecatory complaints. The use of the midpubic line, which is available as both a clinical and radiological reference point, is quite promising for the evaluation of pelvic organ prolapse. Additionally, if ongoing studies continue to prove that the midpubic line reliably correlates with the clinical hymen; this study may propel a much needed merging of terminology between pelvic prolapse surgeons and radiologists.
None.
The author declares that there is no conflict of interest.

©2014 Nosseir, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.