Open Access Journal of
eISSN: 2576-4578


Research Article Volume 2 Issue 5
1Department of Intensive Care, University of Hawaii, USA
2Department of Respiratory, Castle Medical Center, USA
Correspondence: Ehab Daoud G, Department of Intensive Care, University of Hawaii, Castle Medical Center, Kailua, Hawaii, USA, Tel (440) 655-9697
Received: February 14, 2018 | Published: November 28, 2018
Citation: Daoud EG, Yamasaki KH, Nakamoto K. Esophageal pressure balloon and trans-pulmonary pressure monitoring in airway pressure release ventilation. different approach. Open Access J Trans Med Res. 2018;2(5):146-149. DOI: 10.15406/oajtmr.2018.02.00057
We are presenting a case of Pulmonary ARDS managed using esophageal balloon catheter to adjust inspiratory pressure and Positive End Expiratory Pressure (PEEP) according to the inspiratory and expiratory Trans-Pulmonary pressures (PL). We observed the pressures when switching the mode from a pressure controlled mode to Airway Pressure Release Ventilation (APRV) using the same inspiratory pressure (PHigh) and used various incremental release times (TLow) to calculate the expiratory Trans-Pulmonary pressure.
Conclusion: At all TLow levels, the Trans-Pulmonary pressure at exhalation was in the negative value, indicating alveolar collapse. A large study is needed to confirm our findings and to help guide setting APRV.
Keywords: esophageal balloon, trans-pulmonary pressure, APRV, PEEP
APRV, Airway Pressure Release Ventilation; PEEP, Positive End Expiratory Pressure in cmH2O; PHigh, Airway Pressure at inspiration cmH2O; PLow, Airway Pressure at exhalation or during release in cmH2O; THigh, Time of inspiration in seconds; TLow, Time of exhalation or release in seconds; PL, Trans-Pulmnary Pressure, Airway pressure minus Pleural pressure
The use of esophageal pressure monitoring as a surrogate for pleural pressure was described in the mid 20th century, however its use has been mostly limited to clinical research.1 Increased interest in using such technology has arisen over last decade after a study published in 20082 using esophageal pressure monitoring to set PEEP in Acute Respiratory Distress Syndrome (ARDS) using the Trans-Pulmonary Pressure (PL) that showed improved oxygenation, compliance and trend towards improved mortality. Further, our improved understanding of Ventilator Induced Lung Injury (VILI)3 makes this technique most appealing in mechanical ventilation to avoid lung stress and strain. Many ventilator manufacturers have incorporated the esophageal pressure monitoring in their products. APRV is considered a non conventional mode of mechanical ventilation that was introduced in the mid 80s of last century.4 APRV is an inverse ratio, pressure controlled, intermittent mandatory ventilation with unrestricted spontaneous breathing5 mainly used as an alternative mode of ventilation in the difficult to oxygenate patient. Among its potential benefits are the long inspiratory pressure phase (PHigh) that maintains alveolar recruitment, and the very short expiratory pressure phase (Plow) or release time creating Auto-PEEP to prevent end expiratory volume loss and alveolar dercruitment.6 However, setting APRV has been a subject of much debate5 with lack of consensus regarding its settings.7
A 61 year old obese male was admitted to the hospital with bilateral severe community acquired pneumonia leading to acute respiratory failure and severe ARDS with PaO2/FiO2 of 75. He was managed with pressure targeted controlled mechanical ventilation (PCV), to target a tidal volume (VT) 6ml/kg IBW, and PEEP was adjusted to 15 cmH2O to maintain oxygen saturation of 90%. However because of high Oxygen requirements (FiO2), an esophageal balloon pressure monitoring was inserted according to the manufacturer’s guidelines (Hamilton Medical AG, Switzerland). The ventilator settings were adjusted to keep inspiratory PL below 25 cmH2O and expiratory PL 0-5 cmH2O (Figure 1). The ventilator mode was changed to APRV as follows: PHigh was set as same of inspiratory pressure of PCV of 30 cmH2O, PLow was set at zero cmH2O, TLow started at 0.1 seconds and increased by increments of 0.1 to 0.7, Release number was 10, with each cycle 6 seconds THigh was variable from 5.9 to 5.3 seconds rselative to the incremental increased TLow. We measured and recorded the Airway pressure (Paw), Esophageal Pressure (Pes), inspiratory and expiratory Trans-Pulmonary Pressure (PL), Tidal volume (VT), expiratory flow, and percentage decay of expiratory flow from peak expiratory flow (PEF) at the end of the TLow. Each setting was recorded for two minutes.
The results are summarized in Figure 2. At all levels of TLow from 0.1 to 0.7 seconds, the expiratory PL were constantly in negative value indicating alveolar collapse. The expiratory flow at the end of the releases ranged from 87% to 75%.
The concept of using an esophageal pressure monitoring to guide setting mechanical ventilation especially PEEP has been on the rise and gaining momentum over the last decade. Research has shown that setting PEEP during conventional mechanical ventilation to maintain a positive Trans-Pulmonary pressure at end of expiration improve oxygenation, respiratory compliance and trend towards improved mortality.2 No such research was duplicated with the use of APRV. APRV setting especially release time (TLow) has been the subject of much debate. The concept of TLow is to create a short release time creating Auto-PEEP to avoid volume loss, and alveolar recruitment at end of expiration. In a previous review article published in 2012, our group described in details the different methods of setting TLow in APRV with the relative advantages and disadvantages of each method.5 Briefly, it has been suggested to set TLow empirically in a range of 0.2-0.8 seconds,6,8 others have advocated to set it to achieve 50-75% of PEF,6 while others have suggested to set it according to a certain time constant (τ)9 (calculated as the product of the static respiratory compliance and resistance), while others have suggested to adjust it for a certain tidal volume per release. DiRocco and colleagues suggested that alveolar recruitment still occur despite short release time in APRV in an animal model of lung injury.10 A previous simulator bench research by our group found out that the Auto-PEEP created during APRV is variable and may not be reliable,11 similarly another bench research that compared three different methods of setting TLow described the difficulties unpredictability of Auto-PEEP with such methods.12
In a recent published APRV review13 we called for research using innovative ways to set APRV, including the use of esophageal pressure monitoring or measuring the functional residual capacity (FRC). To our knowledge this is the first attempt to investigate the PL in APRV. A recent study by Kollisch-Singule and colleagues,14 the investigators used esophageal balloon monitoring in APRV to monitor respiratory mechanics in an animal model of extra pulmonary lung injury with no mention of PL during the release time (TLow). Our case is just “food for the thought” and hopefully will encourage more research into this controversial and critical aspect of setting APRV. An intriguing observation in our case is, the esophageal pressure change during the release did not parallel the airway pressure (Figure 2), though as expected the drop has increased steadily from the 0.1 to 0.7 seconds. The explanation for that is the different compliances and thus time constants between the lung and the chest wall. Our patient’s total respiratory system compliance (CRS) calculated as the tidal volume divided by plateau pressure (obtained during brief inspiratory pause) – total PEEP was 50 ml/cmH20, the chest wall compliance (CCW) calculated as tidal volume divided by esophageal/pleural pressure (PPL) was 29 ml/cmH2O, and finally lung compliance (CL) was 21 ml/cmH2O calculated as CRS - CCW (Figure 3). The worst compliance of the lung would mean faster emptying and collapse compared to the higher chest wall compliance. Furthermore an important issue not to be missed; as our patient time constant (τ) was 0.2 seconds, calculated as compliance X resistance, i.e. 0.05 L/cmH2O X 4 cmH2O/L/S, the expiratory flow did not decay by 63.2% each 0.2 seconds to almost reach zero at 4 time constants of 0.8 seconds as expected per a mathematical method previously published (Figure 4).5 This finding confirms our previous observation that the flow decay differs with the ventilator model and from the mathematical theory to the bedside10 and thus using the time constant to set TLow may not be accurate.

Figure 3 Ventilator graphics display during Volume Controlled Ventilation (VCV) with an inspiratory hold maneuver to calculate the static compliance of respiratory system (CRS) and airway Resistance (R) On the X axis from top to bottom: airway pressure, esophageal pressure, and trans-pulmonary pressure all in cmH2O. Y axis is time in seconds.
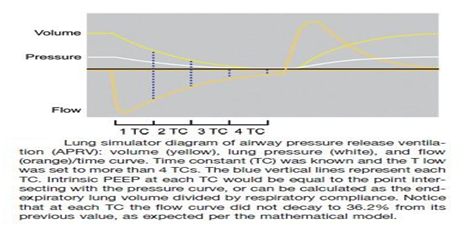
Figure 4 Lung simulator diagram of Airway Pressure Release VVentilation (APRV): volume (yellow), lung pressure (white), and flow (orange)/time curve. Time Constant (TC) was known and the T low was set to more than 4 TCs. the blue vertical lines represent each TC. Intrinsic PEEP at each TC would be equal to the point intersecting with the pressure curve, or can be calculated as the end expiratory lung volume divided by respiratory compliance. Notice that at each TC the flow curve did not decay to 36.2% from its previous value, as expected per the mathematical model.
Our case has some limitations in addition to the inherit limitation of the esophageal balloon pressure monitoring;1 first as being a report in one patient, and the short observation time. Secondly we kept the PHigh constant and didn’t adjust it, similarly we did not adjust the number of releases so consequently the THigh got shorter each time the TLow was increased, in retrospect we might have needed to change those variables to evaluate if that would have an effect on the expiratory PL. Additionally as mentioned above, the exact amount of Auto-PEEP in APRV is hard to obtain or calculate at the bedside, and doing an expiratory hold maneuver at the end of the release was never documented as the way to measure total PEEP or the auto-PEEP if using PLow of zero, consequently we did not apply an expiratory hold at the end of the release. Figure 5 shows an expiratory hold maneuver in a different patient on APRV. The expiratory PL was computed using the airway pressure at the TLow (bottom arrow), but if we used the airway pressure at the end of the expiratory hold (upper arrow) then PL would be different. This dilemma need to be further determined and accounted for. Hopefully new research and observations take an account of those limitations.
Setting APRV with the aid of esophageal balloon to measure PL is conceptually valuable and relatively feasible.
Setting TLow in APRV according to the percentage of PEF might not be valid in avoiding alveolar collapse. More studies are needed to confirm those findings.
None.
The authors declare that there is no conflicts of interest.

©2018 Daoud, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.