MOJ
eISSN: 2573-2927


Mini Review Volume 3 Issue 4
1Department of Biological Sciences, Federal University Gusau, Nigeria
2Department of Biological Sciences, Bayero University Kano, Nigeria
Correspondence: Muhammad Ali, Department of Biological Sciences, Federal University Gusau, Nigeria, Tel +2347032967252
Received: July 22, 2018 | Published: September 6, 2018
Citation: Ali M, Nas FS. Exercise for the management and treatment of cervicogenic headache: a narrative review. MOJ Yoga Physical Ther. 2018;3(5):85-88. DOI: 10.15406/mojypt.2018.03.00050
Headache is probably the most common problem seen in clinical practice by health care professionals, with tension type, cervicogenic headache, and migraine as the most common forms. Cervicogenic headaches may cause either mild discomfort or severe pain due to damage or injury to the nerves in the cervical spine. Most cases of this form of headache can be alleviated, or prevented, by stretching and strengthening the head and neck muscles, tissues, and bones. Clinical studies have shown improvement of cervicogenic headache episodes when combining stretching exercises with targeted strengthening exercises. Such exercise include; Craniocervical Flexion (CCF) Exercise, Flexion and Extension Exercise, Rotation Exercise, Lateral Flexion Exercise, Chin Tuck Exercise, Back-Strengthening Exercise and Shoulder Blade Exercise. This paper reviews the causes, sign and symptoms, anatomy and physiology as well as some exercise used in the management and treatment of cervicogenic headaches.
Keywords: cervicogenic headaches, cervical spine, exercise, nerves
HIS, international society of headaches; CGH, cervicogenic headaches.
In the twenty-first century, headaches are very common and cause substantial pain and disability. Headache is probably the most common problem seen in clinical practice by health care professionals, with tension type, cervicogenic headache, and migraine as the most common forms.1 These headaches are associated with a high burden of suffering and considerable socioeconomic costs.2 According to the World Health Organization (WHO) at least 47% of adults have suffered from headaches in the last year. Worldwide, only a minority of the headaches is diagnosed correctly.3 Ignorance on the part of the professionals and the underestimation of this pathological entity are factors that make it difficult to diagnose it, and consequently, the treatments prescribed to the patients are inadequate. The headache, in addition to causing pain, impact negatively on the quality of life of the person, incapacitating him for the accomplishment of activities daily and causing socio-economic problems.3 The International Society of Headaches (IHS) published in 2013 the third edition of the International Classification of headaches, dividing in primary and secondary and between primary headaches, in which the pain is unique or main symptom are: migraine, tension headache, trigeminal-autonomic headaches and other primary headaches (headache, physical exertion, external pressure). On the contrary, secondary headaches, pain is a consequence of some other process. This group highlights the headaches attributed to head trauma, cervical, vascular disorders and psychiatric disorders.4–6
Cervicogenic headaches (CGH) are chronic or recurring in nature and have been found to arise from musculoskeletal dysfunction of the cervical spine (neck). The lifetime prevalence of headaches in adults may be as high as 20 to 30 percent. Conservative treatment, such as physical therapy, often is recommended as a first line of headache management. Treatment may include manual therapy, pharmacological drugs, physical therapy, and relaxation/cognitive therapies.5 Cervicogenic headache pain has been mostly related to joint, disk, and ligament pain from the upper cervical spine. However, the upper cervical spine also receives afferent inputs from muscles. The role of referred pain to the head elicited by muscle tissues has received particular interest in recent year. 6,7 Patients with cervicogenic headache demonstrated declines in the quality of life comparable to Migraine patients and patients with tension-type headache, with even lower scores for physical functioning.8
Cervicogenic headaches (CGH)
Cervicogenic headaches (CGH) are chronic or recurring in nature and have been found to arise from musculoskeletal dysfunction of the cervical spine (neck).9 Although the prevalence of CGH is considerably lower than tension-type headache and migraine, patients with CGH have a substantial quality of life burden, comparable to patients with migraine and tension-type headache.9 The first part of “cervicogenic” refers to the cervical spine, comprising seven bones more commonly known as the neck; “genic” means that the headache is generated in this area, particularly the upper three bones. In other words, what feels like a dull, achy pain in the head really has its roots in the neck.10
A “cervicogenic episode” can last one hour to one week. Pain typically is on one side of the head, often correlating with the side of the neck where there is increased tightness.9 Almost certainly, range of motion will be compromised. Common causes of CGH can be chronic: poor posture, as noted above, or arthritis. They also can be traumatic: the result of sudden, forceful movement of the skull and neck as with whiplash caused by a car accident, a fall, or an athletic collision. Headaches that develop three or more months after a concussion, according to one study, generally are not caused by brain or head injury. This suggests a connection to the cervical spine.11 This study also indicated that CGH affects four times more women than men. Neck positions and specific occupations, such as hairdressing, carpentry and truck/tractor driving; have been linked to CGH.11 Diagnosis of CGH can be tricky because it can resemble other headaches and can trigger other headaches, such as a migraine. Most often, CGH results from the joints of the neck being stiff, sore and inflamed. The adjacent nerves become irritated and refer pain to the neck, shoulder and head, including the face and behind an eye.9 Known as a secondary headache, a cervicogenic headache may be caused by a blocked nerve or other health condition originating at a source within the cervical spine (Figure 1). This may include the blood vessels, discs, ligaments, or muscles of the neck or back.11
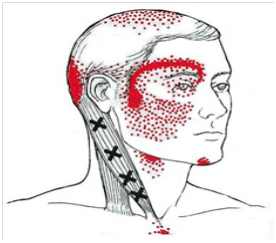
Figure 1 Cervicogenic headach.12
Anatomy and physiology of a cervicogenic headache
What distinguishes a cervicogenic headache from more classic headaches like migraines or tension type headaches are that cervicogenic headaches are actually caused from dysfunction from the neck. Cervicogenic headaches are a form of referred pain – meaning that although the source of the pain is in the cervical spine, the sensation of pain is felt in the head as a headache. This happens because there are nerves in the upper cervical region (C1, C2, and C3) that have connections to nerves of the head (cranial nerve V via the trigeminal nerve spinal tract). Although some controversy exists, a vast majority of the literature agrees that the most common cause of cervicogenic headaches is dysfunction from the C2-3 zygapophysial joints (facet joints).12 However, there is also literature to support that cervicogenic headaches can arise from dysfunction in the C2-3 and C3-4 intervertebral discs of facet joints, as well as the atlantoaxial (C1-2) and atlanto-occipital (C0-1) joints.13
Signs and Symptoms of Cervicogenic headaches
A “cervicogenic episode” can last one hour to one week. Pain typically is on one side of the head, often correlating with the side of the neck where there is increased tightness.9 According to Physical Therapy Institute (PTI),14
Cervicogenic headache exercises
Cervicogenic headache exercises may be the key to alleviating the pain and discomfort of the neck-related headache. The maneuvers are specialized strengthening techniques and stretches for neck pain and headaches that work to relieve the tension, as well as improve a range of motion. Physical therapy and prescription medications may serve as complementary treatments in severe cases.15 Cervicogenic headache treatment tends to focus on the stretching and strengthening of the bones, ligaments, and muscles of the neck. An appropriate regimen of targeted exercises can be determined during any required physical therapy for headaches, specifically those of a cervicogenic nature. Begin by performing cervicogenic headache stretching exercises three to five times daily, increasing the number of repetitions each time.16
i. Craniocervical Flexion (CCF) Exercise: This is done by lying down on the back with a rolled towel behind the neck. A nodding motion will be made with neck and head and hold for 10 seconds. This is Progress to raising arms on either side for the duration of the hold. Once the neck and head are strong, sit against a wall and perform the nodding motion and holding position without neck support.17
ii. Flexion and Extension Exercise: In a sitting or standing position, the chin was brought to the chest slowly and hold for 30 seconds for a gentle stretch to the back of the neck. Next, the head is moved back so that the eyes are focused on the ceiling to stretch the front neck muscles. This position is to be hold for 30 seconds. Strengthen the neck muscles by placing hand on forehead and attempting to push it against the hand. Hold the position for 10 seconds. Next, is to place the hand on the back of the neck and head and move the head backward with eyes looking up toward the ceiling. Hold this position for 10 seconds (Figure 2).18
iii. Rotation Exercise: This is done by standing or sitting in an erect position as the head turning to the right, looking over the shoulder. This positioning is to be hold for 30 seconds before returning to the original position. The procedure is repeated on the left side. Then gradually progress to placing the right hand on the right temple of the head for resistance as turning the head. The position is to be hold for 10 seconds before repeating on the left side with the left hand and temple (Figure 3).17
iv. Lateral Flexion Exercise: This is done by standing or sitting and dropping the head to the right side. This is followed by touching right shoulder to the right ear without moving the shoulder upward. This positioning is to be hold for 30 seconds and return to the starting position. The procedure is repeated on the left side. These muscles were strengthens by hand as resistance support against the temple. The position is to be hold for 10 seconds on each side (Figure 4).17
v. Chin Tuck Exercise: While in a standing or sitting position, gently move the shoulders backward as the chin is tucked down towards the chest. Remain forward facing and hold the position for 10 seconds. The procedure is to be repeated 10 times (Figure 5).16
vi. Shoulder Blade Exercise: This is done while sitting or standing with hips straight, not leaning forward or backward. Slowly move the shoulders backwards and gently thrust the chest outwards and hold the position for five seconds. Release and return to the staring position and repeat 10 times (Figure 6).16
vii. Back-Strengthening Exercise: During back strengthening exercise, one lie on stomach with face down to floor. This is followed by deep inhalation and exhalation several times. Then prop the upper body onto elbows and hold the position for up to two minutes (Figure 7).17
Most cases of cervicogenic headache can be alleviated, or prevented, by stretching and strengthening the head and neck muscles, tissues, and bones. Clinical studies have shown improvement of cervicogenic headache episodes when combining stretching exercises with targeted strengthening exercises. Such exercise include; Craniocervical Flexion (CCF) Exercise, Flexion and Extension Exercise, Rotation Exercise, Lateral Flexion Exercise, Chin Tuck Exercise, Back-Strengthening Exercise and Shoulder Blade Exercise.
None.
The author declares there are no Conflicts of interest.

©2018 Ali, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.