MOJ
eISSN: 2379-6162


Review Article Volume 3 Issue 4
1Department of Surgery and Maxillofacial traumatology, State University of Feira de Santana (UEFS), Brazil
2Department of Surgery and Maxillofacial traumatology, Federal University of Bahia (UFBA), Brazil
3Department of Medical Sciences, Bahiana School of Medicine and Public Health (EBMSP), Brazil
4The Bahiana School of Medicine and Public Health (EBMSP), Brazil
Correspondence: Eduardo Azoubel, Department of Oral & Maxillofacial Surgery, State University of Feira de Santana, Bahia, Brazil, Rua dos Prazeres, 238, casa 4, Bairro Caji, Lauro de Freitas Bahia Brazil, Tel +557199827174, Fax +557133518637
Received: August 31, 2016 | Published: September 26, 2016
Citation: Azoubel E, Freitas AC, Azoubel MCF, et al. Reabsorbable wire use for fixing membrane on bone graft surgery. MOJ Surg. 2016;3(4):90-92. DOI: 10.15406/mojs.2016.03.00051
The ability to minimize or simplify the surgical procedure is a differential item for time and biological gain for patients, and often reduces the cost operative end. Added to this the use of common everyday materials in surgical and transport, which contribute to reducing the training time, also known as "learning curve" to master a surgical technique. Based on those principles, and the apparent lack of scientific literature related to patch clamp methods, this paper presents a simple and practical technique for stabilizing the same intra-oral surgery through the use of resorbable yarns stabilized in their own bone of the patient.
Keywords: alveolar ridge augmentation, grafts, membranes, bone regeneration, case report, dental implants, surgical flaps
Working with surgery you must have a vast knowledge of the techniques, anatomy, physiology and cell biology itself as this is quite specific when the healing time, an important factor in surgical postoperative.1-3 With all this knowledge becomes can minimize or simplify surgery, reducing the operative time and biological damage in patients also can often reduce the cost operative end.
Regarding bone grafts there is a greater concern vascularization, adaptation, tissue tension and stability.4-6 Therefore it is important to prioritize the dissection and preparation of tissues pair closure of the surgical wound so there is a healing for the first intention.4,7
Even taking all precautions, complications may arise with edema and tissue dehiscence, the most common complications. Edema may soon arise after surgery and stay for a period of 2 to 3 days, Reducing after.8,9 And dehiscence can occur due to some carelessness at the time of closure of the surgical wound, making the healing by first intention.4,10 In order to reduce time, cost and postoperative complications new techniques and materials have been used. Based on these precepts and apparent lack of scientific literature related to the patch clamp methods, this paper aims to provide a simple and practical technique to stabilize membranes by using resorbable wires stabilized the very bone of the patient.
To work with surgery have to be aware of several factors, including cell biology is very specific and the healing time after surgery in the epithelium takes place in a period of 12 h is approximately 0,5 to 1 mm per day, 1 tissue connective 0,5 mm bone day 2 and 50 micrometers per day and about 1.5 mm to month. 3 So protecting particulate bone grafts or blocks is essential to allow bone healing and prevent tissue proliferation which is much faster.
Both bone grafts as the tissue graft has been already used for some time and concern in both is closely related to vascularization, adaptation, stability and lack of tissue tension to allow closure by first intention, important details that are not observed can generate complications and limitations on acts cirúrgicos.4-6
Before starting any bone procedure is important to give priority to dissection and preparation of tissue will close the wound so that it can obtain sufficient elasticity so that there is a lock for the first intention4,7 and moreover the incision site can be a significant factor in the incidence of exposure of the membrane and reduced tissue necrosis.11,12
The biggest cause dehiscence in wounds is the failure flap closure causing stress, infection, trauma opposing tooth, irritation by a removable prosthesis and development of hematoma and when this type of complication is more prudent to allow it to close by secondary intention and should not try to suture area again.4,10
The edema can start within minutes or hours after surgery and continued for a period of approximately 2 to 3 days before starting its regression.8,9
Greater attention to the clinical success of the use of membranes should be evaluated, as they may be affected by the habits of the patients,13 morphological defects,14 manipulation of cortical bone, 7 type of material used15,16 and membrane stability.17
Many authors have suggested a variety of clinical protocols that include flaps positioned coronally, change pedicle flap techniques, gingival grafts and tissue expansion in an attempt to keep the soft tissue with a primary closure after guided bone regeneration.18-20
Studies have been conducted on cadavers through a study visualizing the course of the arteries using different techniques macroscopic and microscopic analyzes to develop incision type recommendations for implants and this analysis revealed that the largest number of arteries is located posterior to anterior, many arteries they run parallel to the alveolar crest in the hall and supracristal area there is an a vascular zone without anastomoseds.21
Among the methods for stabilizing membranes can cite rates, screws and many studies to bone fixation has been done and among them a more modern materials such as screw N-2-butyl cyanoacrylate for fixing bone blocks in the jaw has been tested22 but we believe that the best method is related to an easy technique, fast and available and routine surgical materials in our arsenal, a fact that encouraged us to describe this technique.
After examination of the area operated and the finding by radiographic examination, which must include a volumetric tomography, that there is deficiency in height or width of the region to be implemented the reconstruction procedure must indicate. The type of graft used depends on each surgeon and it is not our purpose to attempt to discuss this issue, but relevant points of the proposed technique.
The first technique to be discussed is the lifting of the maxillary sinus and after you do all maxillary sinus membrane lifting technique are held four symmetrical holes in the bone edges with drill 701 to reach the surgical cavity (Figure 1).
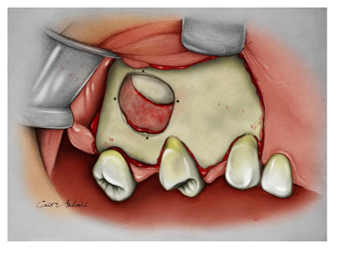
After drilling to insert the material that will fill the internal cavity of the maxillary sinus (Figure 2) fits the chosen membrane, either absorbable or non absorbable (Figure 3). And it will be sutured with absorbable wire using the holes previously made (Figures 4&5).
It is important to stress that in most cases the needle should be inserted into the inner part which is bone to the outside and great care must be taken when using collagen membranes, because the wire can come severs such membrane when shook too much the knot.
After it is found that the membrane has stability can thus counteract the retail muco-periosteal and complete the surgery with suturing the flap on the operated area and always worrying about tissue tension for the site to be closed passively
The use of resorbable wires allows the stabilization of membranes, so these remained stable even after the manipulation of the surrounding soft tissue, but should be intensified care in the management and control of force when suturing it may be lacerations of the membrane in the areas of suture when the inlet and outlet perforations were very close.
None.
The author declares no conflict of interest.

©2016 Azoubel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.