MOJ
eISSN: 2379-6162


Letter to Editor Volume 11 Issue 1
1Hospital Regional de la Orinoquía, Colombia
2Estudiante de medicina, Juan N. Corpas, Colombia
3Magíster VIH/SIDA, Hospital Regional de la Orinoquia, Colombia
Correspondence: Julio César Velasco Castro, 1MD. Hospital Regional de la Orinoquía,Yopal, Colombia. Celular: 3108799898. Dirección: Carrera 8B N°45-32
Received: February 15, 2023 | Published: March 31, 2023
Citation: Velasco JC, Corredor JM, Agudelo LG. Letter to the editor regarding a case of clinical and tomographic simulation of leiomyosarcoma and leiomyomatosis. MOJ Surg. 2023;11(1):49. DOI: 10.15406/mojs.2023.11.00220
In a conversation with the medical staff of the gynecology area and the research department, cases of patients with particularities in the presentation of the natural history of each disease that hinder a timely diagnosis and effective treatment are occasionally discussed. A 37-year-old female patient with a history of myomatosis 8 months earlier and lower abdominal pain accompanied by abnormal uterine bleeding presented to our institution. A contrasted abdominal CT scan showed giant uterine myoma without ruling out leiomyosarcoma (Figure 1). The expert panel and with the patient's consent performed total abdominal hysterectomy and bilateral salpingectomy. The histological report showed leiomyomatosis and a diagnosis of leiomyosarcoma was ruled out.
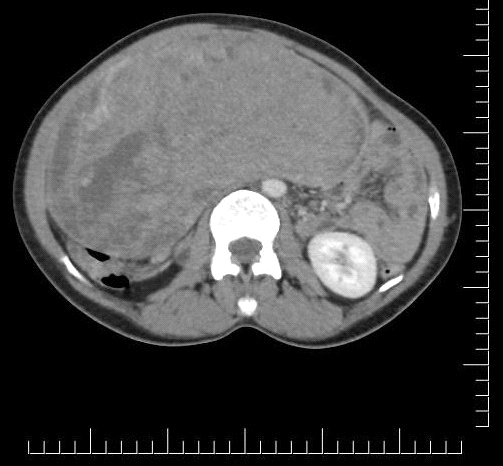
Figure 1 Computed axial tomography of the abdomen with contrast, solid image dependent on the myometrium, with defined contours, with areas of greater and lesser density in its interior (14-50 HU), vascularization can be seen when the contrast medium is applied.
Leiomyosarcoma represents 1% of malignant tumors of the uterus and is diagnosed in 30% of women between 40 and 60 years of age; in most cases survival is low due to aggressive behavior and high mortality.1 It is known that uterine myomas are usually associated with the development of leiomyosarcoma and that some sarcomas usually transform to malignant in 3-5% of cases due to alterations in mitosis.2 From the tomographic study, clinicians can have a diagnostic approach according to the imaging characteristics presented, finding a large tumor in the abdominopelvic region, heterogeneous, solid cystic appearance are the main characteristics of a sarcoma in the context of a young patient with a significant history of myomatosis and a clinical picture suggestive of tumor lesion.2,3
In clinical practice, a complete anamnesis allows inferring more precise diagnostic probabilities; however, some pathologies make their timely diagnosis difficult due to their clinical and imaging similarities. The purpose of this case is not to underestimate the clinical expertise of physicians and even less to make them lose importance, but to show that based on the experience of a panel of experts, a diagnostic presumption of leiomyosarcoma was initially made, but based on the recommendations of the American guidelines, these neoplasms are studied histologically to give a confirmatory diagnosis, showing that in some cases the clinical accuracy is erroneous and in most cases, the therapeutic approach ends up being surgical in all gynecological tumor lesions.
None.
The authors declare no conflicts of interest.

©2023 Velasco, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.