MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 1
1Doctor, attached to the department of Ginecología and Obstetricia, Cirugía Laparoscópica Hospital Español de México, Mexico City, Mexico
2Doctor of Gynecology and Obstetrics, Hospital Español de México, Mexico City, Mexico
3General Surgery Resident, Hospital Español de México, Mexico City, Mexico
4Medical intern of social service, Mexico City, Mexico
5Doctor assigned to the Department of Obstetrics and Gynecologic Oncology, Hospital Español de México, Mexico City, Mexico
Correspondence: Gallardo Navarro Elias, General Surgery Resident, Hospital Español de México, Mexico City, Mexico
Received: February 25, 2024 | Published: March 5, 2024
Citation: Acosta SV, Pioquinto AJP, Elias GN, et al. Intestinal adenocarcinoma of the uterine cervix with gastrointestinal metastasis. MOJ Surg. 2024;12(1):19-21. DOI: 10.15406/mojs.2024.12.00253
Introduction: Endocervical adenocarcinomas represent a very heterogeneous group of tumors. Mucinous adenocarcinoma of the intestinal type is a rare histologic variant.
Clinical case: 38-year-old female patient, who consulted for abnormal uterine bleeding, as well as more frequent cycles accompanied by dysmenorrhea, denying any other added symptomatology. She also underwent speculoscopy where a verrucous lesion was found, hypervascularized at that time, a biopsy which reported endocervical mucosa with moderate chronic inflammation and papillary, mild vascular congestion, compatible with endocervical polyp and MRI with enlarged uterus with thickened endometrium myometrium and nodular endometriotic implant of cystic appearance in the cervical isthmus junction. Due to the persistence of the symptoms it was decided to perform a total hysterectomy by laparoscopy, intraoperatively moderately differentiated adenocarcinoma implants were observed, compatible with endocervical primary. It was decided not to continue with the surgical time for neoadjuvant chemotherapy management.
Conclusion: Establishing the preoperative anatomopathologic diagnosis is decisive to improve the treatment to reduce morbidity and mortality of the patient.
Keywords: cervical adenocarcinoma of intestinal type, metastasis, abdominal pain, endometriosis
Endocervical adenocarcinoma is a heterogeneous group of neoplasms, accounting for 10-25% of all cervical carcinomas, more than 90% of adenocarcinomas are caused by persistent infection with high-risk human papillomavirus (HPV), the most common HPV types being 18, 16 or 45,1,2 endocervical adenocarcinoma of the usual type was defined as "the most common type of adenocarcinoma with relative mucin depletion", on the other hand, mucinous endocervical adenocarcinomas included gastric type, intestinal type and signet ring cell tumors, these groups can be present in tumors of diverse etiologies such as goblet cell adenocarcinomas (intestinal) which can be associated or independent of HPV, at present it is well established that gastric type mucinous adenocarcinomas are a highly aggressive tumor and its etiology is not related to HPV infection.1,3,4 The 2014 World Health Organization (WHO) Classification of Tumors of Female Reproductive Organs includes gastric-type adenocarcinomas as a variant of mucinous endocervical adenocarcinomas and other authors add the following varieties: villoglandular, serous, intestinal-type, signet ring, and metastatic adenocarcinoma, however in the new 2020, WHO categorization of endocervical adenocarcinomas, which is the subject of this review, and the international criteria and classification system for endocervical adenocarcinoma (IECC), which was first described in 2018, divides endocervical adenocarcinomas into different types based on association with HPV, correlates with clinical features, on p16 expression and HPV status, survival and response to treatment and prognostic parameters.1,5,6 This system is based on the identification of mitotic figures and apoptotic bodies at 40-100x magnification on hematoxylin and eosin (H&E) stained slides and is therefore easy to apply in daily practice. When readily identifiable mitoses and apoptotic bodies are observed at this power, the tumor is likely to be HPV-associated, when mitoses and apoptotic bodies are absent or found with difficulty at high magnification, the tumor is likely to be HPV-independent.1,7 The 2014 WHO classification system grouped HPV-positive and HPV-negative tumors (such as gastric-type adenocarcinomas) with abundant intracytoplasmic mucin into the mucinous category. However, the IECC and WHO 2020 systems include mucinous adenocarcinoma (non-gastric type) as HPV-associated adenocarcinoma, with the following subcategories such as intestinal by the presence of goblet cells, representing ≥50% of the usual type or mucinous background cells, also Paneth-like cells which can also occasionally be seen in this type, signet ring which are round cells with a mucinous vacuole that displaces the nucleus towards the periphery, representing ≥50% of the cells in a usual type background. Intestinal differentiation is also found in gastric-type tumors, which are HPV-independent, this intestinal subtype can be positive for CDX2 and CK20.3,5 Several HPV-related mucinous-type endocervical adenocarcinomas are sometimes misdiagnosed as gastric-type endocervical adenocarcinoma, and the distinction can be particularly difficult with a small biopsy specimen, thus most HPV-associated mucinous tumors have easily detectable mitotic figures and apoptotic bodies at 40 to 100× magnification, whereas in gastric-type tumors, mitosis and apoptotic bodies are usually rare but intestinal differentiation can occur in both types. Testing for p16 and HPV can help with diagnosis in problematic cases, but p16 is rarely negative in HPV-associated carcinomas and rarely positive in gastric-type carcinomas.1,6
This is a 38-year-old female patient, with no medical history of importance. Gynecological and obstetric history: menarche at 12 years of age, gestation 1, cesarean section 1 in 2020, she has a pap smear in April 2023 with negative report of malignancy. Her surgical history includes laparotomy with right oophorectomy in September 2023 due to the presence of endometrioma. Her condition began 6 months prior to her evaluation when she presented abnormal uterine bleeding due to an increase in the number of periods, as well as more frequent cycles accompanied by dysmenorrhea, she denies any other added symptomatology. On arrival, a complete physical examination was performed, where the vaginal examination revealed a barrel-shaped cervix, speculoscopy was performed and a verrucous lesion was found, hypervascularized at that time, a biopsy was performed which reported endocervical mucosa with moderate chronic inflammation and papillary, mild vascular congestion, compatible with endocervical polyp. No neoplastic cells were identified. Medical treatment is started with analgesics without improvement of the picture and an MRI is requested with mapping for endometriosis in which it is reported: Uterus in anteversion, globular appearance, increased in size with dimensions of 10.8 x 7.6 x 7.2 cm with an image on the posterior wall measuring 11 mm and is 100% intramural. Endometrial myometrial thickened area of 16 mm. Diffuse adenomyosis, endometrioma in left ovary of 3 cm. Nodular endometriotic implant of cystic aspect in cervical isthmus junction. For these reasons, together with the patient, it was decided to perform a total hysterectomy by laparoscopy and endometriosis resection. At the beginning of the procedure, lesions were observed (Figure 1), which macroscopically were not compatible with endometriosis, so biopsies of the lesions were taken and sent for transoperative study.
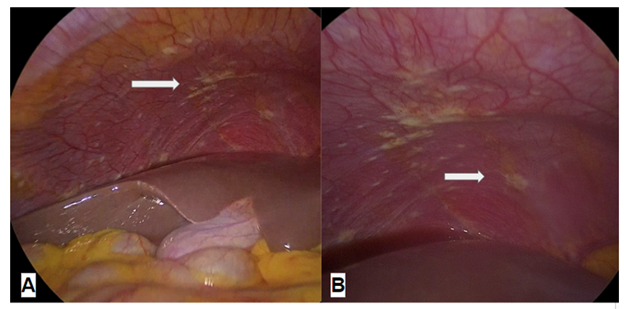
Figure 1 Laproscopic image of lesions at the level of the right costal grid, (B) Laproscopic image of lesions in the right parietocolic region.
While waiting for the transoperative report, the surgical plan was continued, finding thickened parametrium, bladder extremely adhered to the anterior uterine wall without success in the bladder descent, fixed ureters, so ureterolysis was performed (Figure 2), lesions at the level of the omentum and indurated nodes with enlargement at the level of the left parametrium (Figure 3). At that time, the gynecologic oncology service was consulted and a biopsy of the macroscopic lesions was indicated, a cervical biopsy was taken vaginally, hysteroscopy with endometrial biopsy and cystoscopy with bladder biopsy (Figure 4).
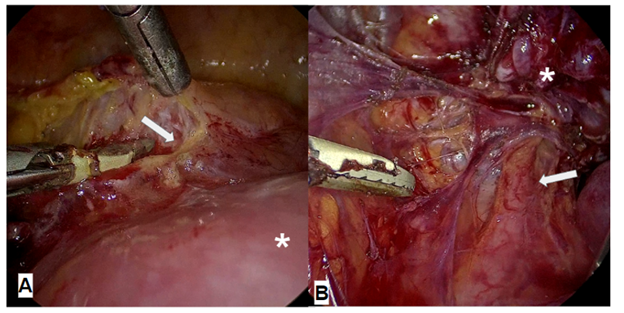
Figure 2 (A) Laproscopic image of the bladder (arrow) attached to the uterine body (asterisk), (B) Laproscopic image of fixed left ureter (arrow).
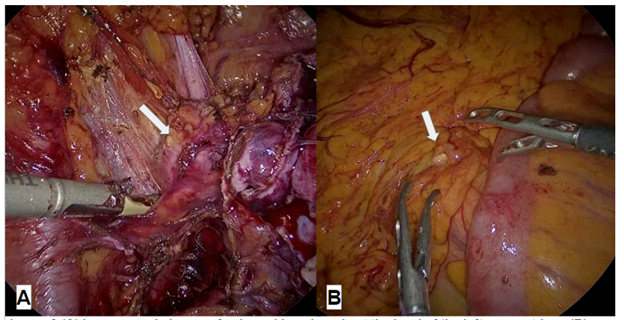
Figure 3 (A) Laproscopic image of enlarged lymph node at the level of the left parametrium, (B) laproscopic surgery of lesion at the level of the omentum.
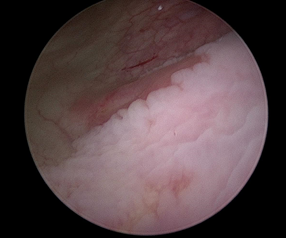
Figure 4 Cystoscopy Figureof bladder mucosa, Bladder mucosa biopsy: Negative for neoplasia. Chronic cystitis.
The transoperative study reports: fibroconnective tissue with moderately differentiated adenocarcinoma implants, immunophenotype CK7+ and MUC-4+. Compatible with endocervical primary, it was decided not to continue with the gynecological surgical time, and the patient was sent to the medical oncology service to start chemotherapy with Paclitaxel and Carboplatin for definitive pathology report in which it was reported, endocervical polyp biopsy: moderately differentiated endocervical adenocarcinoma of intestinal type, omentum biopsy: moderately differentiated adenocarcinoma implant. immunophenotype ck7+/ ck20+ patches/ protein p40+/ muc -4+/ protein o16+/ cdx-2+/ villin+/ ca125-5+/ ca 19-9+. compatible with primary endocervical primary of intestinal type with squamous differentiation, biopsy of endocervix, moderately differentiated endocervical adenocarcinoma of intestinal type and left parametrial lymph nodes: 2 lymph nodes with metastasis of moderately differentiated endocervical adenocarcinoma of intestinal type with squamous differentiation.
The usual and mucinous types are associated with HPV infection; gastric, clear cell, mesonephric and endometrioid types are not HPV-driven.8 The distinction between HPV-associated and HPV-independent endocervical adenocarcinomas has important clinical implications, as HPV-independent tumors tend to develop in older patients, present at a higher clinical stage, have a poorer prognosis, have different and unusual patterns of spread, and respond differently to typical oncologic treatment for cervical cancer. In addition, the fact that some endocervical adenocarcinomas are HPV-independent is important for HPV-based vaccination strategies and screening programs.1,9 Since HPV-associated and HPV-independent endocervical adenocarcinomas have different molecular drivers, it is imperative to understand their unique characteristics, which is necessary for the development of future targeted therapies, ongoing genomic studies and clinical trials, which will hopefully add further to our understanding of this rare group of tumors.2 Prognostic factors include TNM and FIGO staging, HPV status, lymphovascular invasion, histologic subtype and degree of tumor differentiation, with small cell and clear cell having the worst prognosis. The recently described HPV-associated type of mucinous endocervical adenocarcinoma has been described as having a poorer prognosis than other HPV-associated types 27,32,33.8,10 Of these, nodal status and number of involved nodes are the most important prognostic factors, with 5-year overall survival rates for stage IB-IIA of 88% to 95% without nodal involvement and 51% to 78% with nodal involvement, while the independent prognostic value of histologic subtype is still controversial. Endocervical EGA shows different morphological and immunological features than endocervical adenocarcinoma of the usual type, but it may be difficult to differentiate it from mucinous adenocarcinoma metastatic to the cervix due to the similar morphology and overlapping immunohistochemical profile.1 Therefore, knowledge of the morphologic features and immunohistochemical profile will enable pathologists to accurately recognize and diagnose this rare and aggressive entity. Even though the aforementioned publications suggest a decrease in the frequency and mortality of invasive cervical cancer, to date there is no documented information available in our setting regarding the increase or not in the frequency of adenocarcinoma of the cervix. Finally, metastasis from another organ should be ruled out in tumors with abundant intracytoplasmic mucin, clinically relevant information can also be used along with ancillary tests, including a panel of immunohistochemical stains and HPV testing. Regarding chemotherapy for patients with GAC, one study used therapeutic options such as Paclitaxel/Carboplatin, Irinotecan and Tegafur/Imeracil/Oteracile therapies, with the selection of agents depending on cancer staging and mainly with treatment in the adjuvant setting.1,11,12
In our experience, preoperative anatopathological diagnosis is of vital importance to offer adequate medical/surgical treatment, since the pathology does not always present in the usual way and becomes a challenge for doctors.
None.
The authors declare no conflicts of interest.

©2024 Acosta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.