MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 1
Departamento de Ciencias de la Salud, Universidad Técnica Particular de Loja, Ecuador
Correspondence: Alexander Lozano Samaniego, Departamento de Ciencias de la Salud, Universidad Técnica Particular de Loja, Ecuador
Received: December 14, 2024 | Published: January 8, 2024
Citation: Rivera SM, Samaniego AL, Lozano RA, et al. Decoding complex mediastinal masses in children: insights from a clinical case. MOJ Surg. 2024;12(1):1-4. DOI: 10.15406/mojs.2024.12.00248
Introduction: In the pediatric population, any mediastinal mass represents a diagnostic challenge considering that most of these lesions have been associated with neoplasms. Advanced imaging modalities such as computed tomography (CT) have proven essential for the identification and characterization of mediastinal lesions.
Objective: To explore the general nature of nerve cell tumors with a radiological approach.
Clinical case: Three-year-old girl with respiratory symptoms with a mass in the mesogastrium of approximately 3 cm. Abdominal ultrasound reports a complex mass. Chest X-ray evidenced radiopacity in the left hemithorax. Plain contrast-enhanced CT of the chest and upper abdomen shows a solid, contrast-enhancing mass with a volume of approximately 387 cc.
Discussion: In the posterior mediastinum, nerve cell tumors are generally grouped into three categories: peripheral nerve, paraganglia, or autonomic ganglion cells, whether sympathetic or parasympathetic, with an incidence of 70%, 25%, and 1-2%. respectively.
Conclusion: Posterior mediastinal lesions in pediatric patients should focus on the study of lymph node tumors due to their high incidence, in addition, they should be evaluated using objective radiological characteristics to avoid complications and consequently take prompt therapeutic action.
Keywords: intrathoracic masses, tomography, radiology, children
The mediastinum, a vital intrathoracic extrapleural compartment, comprises crucial structures with referential limits dividing it into three anatomical spaces (anterior, visceral, and posterior).1 Pathologies affecting these spaces are closely linked to demographic and physiologic factors. The anterior mediastinum, characterized by the 4T mnemonic (thymoma, germ cell tumors, lymphoma, and thyroid tumors),2 presents specific lesions, while the visceral mediastinum harbors conditions like foregut duplication cysts (FDC), lymphadenopathy, and infectious sequelae-associated lesions. Nerve cell tumors, arising from ganglionic chains or autonomic nerves, predominate in the posterior mediastinum, typically located in the abdominal region.3 Tumors originating from peripheral nerves include schwannoma, neurofibroma and malignant peripheral nerve sheath tumor (MPNST); whereas, sympathetic ganglion tumors include neuroblastoma, ganglioneuroblastoma, and ganglioneuroma.4
Pediatric population, mediastinal masses pose diagnostic challenges due to their association with neoplasms. Early evaluation focuses on distinguishing malignant lesions from benign or locally aggressive inflammatory conditions. Advances in noninvasive imaging, particularly computed tomography (CT), play a fundamental role in identifying and characterizing mediastinal lesions. CT offers crucial information about tumor location, size, and anatomical relationships, boasting high sensitivity (88.9%) and specificity (92.6%).5
This article delves into the clinical case of a pediatric patient diagnosed with a sizable mediastinal mass, emphasizing the exploration of nerve cell tumors, their pathogenesis, and histologic classification. By conducting an in-depth review of noninvasive imaging, the aim is to guide the medical team in formulating an optimal therapeutic strategy based on precise tumor characteristics.
Three-year-old girl with no significant personal or family history, attended with her father, who reported that the patient presented clinical symptoms characterized by pain in the mesogastrium since 6 months ago, to which she did not pay attention, a week ago the pain intensified accompanied by nausea that did not lead to vomiting. On physical examination, on deep palpation in the mesogastrium there is evidence of a mass of hard consistency, well-defined borders of approximately 3cm in diameter, non-mobile. An abdominal ultrasound was sent and reported a complex mass in the pancreas, round edges, slightly heterogeneous content, negative Doppler, measuring 8.9x7.9x9.6cm. Due to limited resolution capacity, the patient was referred to a more complex health care facility, and the clinical picture was accompanied by a wet cough and an unquantified thermal rise. Chest X-ray reports blurring of the left costo-diaphragmatic angle, blurring of the cardiac silhouette due to the presence of radiopacity in the left hemithorax (Figure 1). CT Scan of the Chest with Contrast and upper abdomen shows a solid mass that captures contrast and with vessels inside, located in the left pleural cavity measuring 8.1cm x 11.2cm x 8.2 cm (width x height x depth) with a volume of approximately 387cc (Figure 2). Due to the complexity of the lesion she was referred to pediatric cardiothoracic surgery where she underwent exploratory thoracotomy obtaining a complete exeresis of the mediastinal mass without complications. A sample was sent for histopathological study which was compatible with ganglioneuroma. The patient was continuously monitored in the pediatric intensive care unit and was successfully discharged after 15 days.
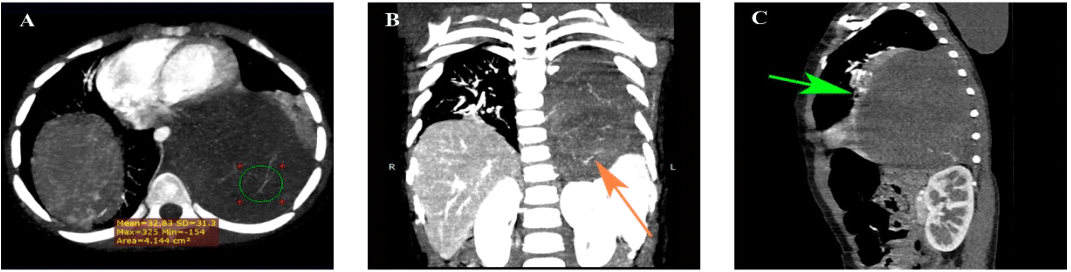
Figure 2 CT Scan of the chest with intravenous contrast media. (A) Axial: In the left lung field there is a homogeneous solid mass of well-defined smooth contours, with heterogeneous enhancement, without contrast medium has an attenuation of 40 HU, there are several visible vessels inside the lesion that appear to depend on intercostal and aortic branches, after the application of contrast medium increases between 10 and 20 HU of attenuation. (B) Coronal: It is located between vertebral levels T3- T11, measuring 8.1cm x 11.2cm x 8.2 cm (width x height x depth) with a volume of approximately 387cc, caudally causes descent of the left diaphragm inferiorly displacing the left spleen, adrenal gland and kidney. (C) Sagittal The mediastinal mass forms acute angles with the parietal pleura and displaces anteriorly the middle mediastinal structures. In addition, it causes left lower lobar atelectasis (green arrow). The mass contacts the descending aorta, esophagus and pericardium, but maintains preserved cleavage planes.
Mediastinal mass is frequently an incidental finding that may include a variety of differential diagnoses, mainly in the pediatric population and, therefore, initial approach is focused on determining or ruling out the presence of malignancy, a characteristic that will be evaluated depending on the compartment in which the lesion is located using radiological and histological criteria.6 According to the classification of the International Thymic Malignancy Group (ITMG), 2017 that allows to delimit with greater precision the mediastinal compartments when using CT as a diagnostic tool, it was possible to establish that the patient presented a mass with paravertebral (posterior) location and consequently associate it with the main differential diagnoses.1
Nerve cell tumors have been characteristically described in the posterior mediastinum and emerge as a particularly interesting and relatively rare entity. Neurogenic tumors are the most frequent posterior mediastinal lesions, they may represent approximately 80% of the lesions found in this compartment, being found in 20% of all tumors in adults and 35% of all mediastinal tumors in pediatric patients.3,7,8
Generally are grouped into three categories according to tumor origin within the mediastinal nerve tissues: peripheral nerves, paraganglia or autonomic ganglion cells, either sympathetic or parasympathetic, with an incidence of 70%, 25% and 1-2%, respectively.7 Of these 3 major groups, the most frequent tumors in pediatric or young adult patients originate from sympathetic ganglia which comprise 25% of neurogenic tumors and include neuroblastoma and ganglioneuroblastoma (malignant tumors) with a frequency of 20%, whereas, ganglioneuroma (rare benign tumor) has a prevalence that reaches up to 42%.7
Radiologically, neuroblastomas present as large, heterogeneous, lobulated soft tissue masses showing heterogeneous or sparse enhancement, low attenuation areas seen within tumor represent pseudonecrosis or hemorrhage. In addition, coarse, finely punctate or curvilinear calcifications may be observed in 50% of thoracic lesions (Table 1).6 About 50% of the patients present with concomitant metastatic lesions.7,9
Ganglioneuroblastoma is a transitional tumor of the sympathetic nervous system that represents an intermediate point between a well-differentiated low-grade ganglioneuroma and a high-grade undifferentiated neuroblastoma, radiologically it can have a more fusiform morphology with respect to neuroblastoma, however, it is difficult to differentiate them (Table 1). Therefore, their definitive diagnosis is made by histopathological analysis.10
Further, ganglioneuroma is a benign tumor located in the posterior mediastinum in 42% to 86% of cases.7,9 In plain CT they are seen as well-demarcated, solid and encapsulated masses that can reach a large size, iso or hypoattenuating to the muscle, although they can also show homogeneous or heterogeneous hypodensity, accompanied by calcifications (~25%) (Table 1). This variable density may mimic other lesions ranging from benign cystic tumors such as large cystic teratoma, bronchocele, esophageal cyst and cystic lymphangioma to malignant tumors including neuroblastoma.9
Table 1 Tomographic characteristics of posterior mediastinal masses
Etiology, clinical stage and radiological findings of these mediastinal masses can sometimes be indistinguishable from each other, which makes it difficult to answer the main question that arises in these cases: is it a benign or malignant lesion? Faced with this dilemma, well-established radiological characteristics have been described to guide us in making an objective assessment. Benign lesions manifest as oblong, well-demarcated, broad-based masses along the anterolateral aspect of the spine; however, as mentioned above, in early stages malignant lesions may have this same presentation. Craniocaudal length ratio (CC) to major axis (MS) is a measurement that helps narrow the differential diagnosis in this category of neurogenic tumor (Figure 3). Benign ganglion tumors generally tend to have a CC/MS ratio >1, which may be related to their plane of growth that follows sympathetic chain path and spans three to five vertebrae, i.e. radiologist can visually have an appreciation only by seeing that the transverse axis is greater than the caudal craniocaudal. This simple measurement can represent a very useful screening method when it is not possible to make a differential diagnosis based solely on the lesion morphological characteristics.8
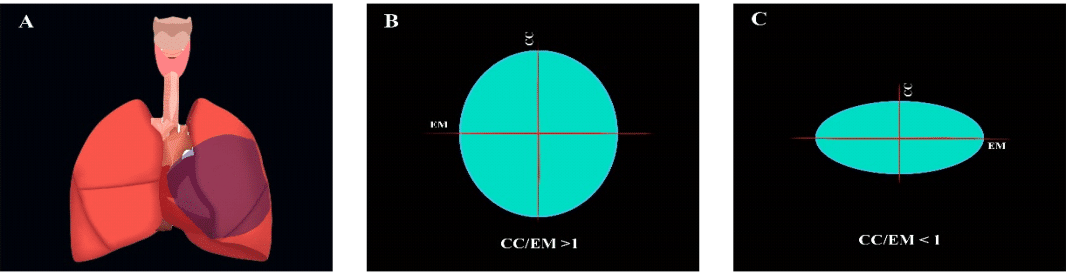
Figure 3 Assessment of mediastinal masses. (A) Uncharacterized mediastinal lesion. (B) Craniocaudal coefficient (CC) in relation to the major axis (MA) >1 associated with benign lesions. (C) Craniocaudal coefficient (CC) in relation to the major axis (MA) > 1 associated with neoplasms.
Standard treatment for mediastinal neurogenic tumors is complete resection by thoracoscopic surgery or thoracotomy; in the case of malignant tumors, radiation or additional chemotherapy may be performed. In any of aforementioned cases, another goal when studying these masses is to avoid or otherwise resolve complications caused by a progressive increase in size that can cause compression of adjacent structures and tissues such as large vessels or nerves, causing acute symptomatology. Definitive therapeutic conduct will depend on the surgical and histopathological findings.7
In this case, despite the patient's age and size of mediastinal mass associated with some imaging findings that initially showed a discouraging outlook, it was possible to perform a complete resection that not only improved the patient's quality of life, but also provides a new learning opportunity to highlight the importance of noninvasive imaging studies as a diagnostic pillar in such complex pathologies that constitute great challenges in medicine.
Posterior mediastinal lesions in pediatric patients should be focused on the study of lymph node tumors due to their high incidence. Furthermore, they should be evaluated using the radiological characteristics like CC/MS ratio, borders, calcifications and density. We emphasize that although CT is not the imaging study of choice for this type of lesions, due to its wide availability compared to magnetic resonance (MR) or PET/CT, considering these radiological parameters could enhance its usefulness as an initial study to perform an early diagnosis. Size of a mediastinal lesion or even its radiological characteristics should not discourage us; this case, in addition to enriching us with a new learning point, emphasizes that in medicine the only invaluable measure is hope.
Patient parents, pediatric area of the IESS Machala General Hospital especially to the nursing staff and Doctors: Byron Pontón, Sandra Sangurima, and Yadira Silva. Finally, to the teaching department of the institution coordinated by Lic. Azucena Sornoza y Tngla. Jessenia Salazar.
The authors declare there are no conflicts of interest.

©2024 Rivera, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.