MOJ
eISSN: 2379-6383


Research Article Volume 12 Issue 2
1School of Public Health, College of Medicine and Health Science, Wachemo University, Hosanna, Ethiopia
2School of Nursing, College of Medicine and Health Science, Wachemo University, Hosanna, Ethiopia
Correspondence: Taye Mezgebu, School of Nursing, College of Medicine and Health Science, Wachemo University, Hosanna, Ethiopia, Tel 0910237995
Received: June 24, 2023 | Published: July 17, 2023
Citation: Tumdado A, Erkalo D, Gizachew A, et al. Infection prevention practice and its associated factors among health care workers at Wachemo University comprehensive specialized hospital, Southern Ethiopia. MOJ Public Health. 2023;12(2):114-121. DOI: 10.15406/mojph.2023.12.00418
Background: Healthcare-acquired infections are a typical global problem mainly in low socioeconomic countries. The acquisition of nosocomial infections may result in prolonged hospitalizations, high antibiotic resistance, lifelong disability, early death, and financial burden on health systems. However, there is scarce data about the level of practice towards infection prevention among Health Care workers and associated factors particularly in the study area.
Objective: To assess infection prevention practice and its associated factors among healthcare workers working at Wachemo University Compressive Specialized Hospital in Hadiya Zone, Southern, Ethiopia.
Methods: A facility-based cross-sectional study was conducted among 379 randomly selected healthcare workers at Wachemo University Compressive Specialized Hospital in Hadiya Zone, Southern, Ethiopia, from July 15 to 30, 2022. Self- administering questionnaires were used. Binary logistic regressions were used to assess the association between the outcome variables and the explanatory variables. The adjusted odds ratio along with 95% confidence interval and p-value less than 0.05 was declared as significant to the outcome variables.
Results: The study found that 168 (45.9%) healthcare workers (95% CI: 40.7%-51.0%) had good infection prevention practices. Having more than five years of work experience (AOR: 4.48, 95%
CI: 2.45-8.16), getting in-services training on infection prevention (AOR: 2.17, 95% CI: 1.303.63), and awareness of the existence of infection prevention guideline in their institution (AOR: 5.59, 95% CI: 3.14-9.92) were significantly associated with the good practice of infection prevention.
Conclusion: Nearly half of the healthcare workers had good infection prevention practices. Having more than five years of work experience, taking in-service training on infection prevention and awareness of the existence of infection prevention guidelines in the institution were all significant factors associated with good infection prevention practices.
Keywords: infection prevention, practices, hospital, health workers, Ethiopia
Infection prevention plays a key role in preventing and reducing the rate of healthcare-associated infection.1 Hospital-acquired infections (HAI) are infections acquired during hospital care that are not incubated at admission and manifest after 48 hours of admission to the hospital. Healthcare-associated infection occurs within 3 days after discharge or 30 days after an operation due to another case. Infection prevention standards enable the entire hospital community safe by preventing, controlling, and reducing Hospital Acquired Infections (HAI). This assists healthcare facilities in following proper( infection prevention) IP practices in a standardized manner, as facilities with substandard IP practices are expected to have several consequences as a result of the cause of poor implementation IP practices.2,3
The most common way of HAI transmission is through the infected hands of healthcare professionals such as physicians, nurses, and other workers. The transmission of pathogens from one patient to another causes the majority of hospital-acquired infections, especially among healthcare workers who do not wash their hands after examining a patient.4
HAI is a typical global problem mainly in low socio-economic countries. Globally, 100 million patients are affected by healthcare-associated infections annually.5 An estimated 10% of hospitalized patients in developed countries and 25% in developing countries develop HAI.6 A systematic analysis of Algeria, Burkina Faso, Senegal, and the United Republic of Tanzania regarding healthcare-associated infections revealed that HAI prevalence ranged from 2.5% to 14.8 %.7 A systematic review and meta-analysis of Ethiopia regarding healthcare-associated infection revealed that HAI prevalence was 16.96%.8
In Zabol, Iran, only 22 % of nurses had good knowledge of nosocomial infection prevention, and 34% of nurses had good practices towards hospital-acquired infection prevention.9 A study done in Bahir Dar shows that 54.2% of health professionals had safe infection prevention practices.10 Few studies conducted in Africa indicated that most nurses working in various health facilities have inadequate knowledge, and skills and lack proper training in standard protocols on infection prevention practices.11
Poor Practice in Infection prevention significantly affects the quality of care for patients in the health facility. To the authors’ knowledge, there is no research done in this kind in the study area. Hence, it can be used as baseline data for future researchers. The findings of this study will also give significant evidence to health professionals, policymakers, and other concerned bodies to improve the practice of infection prevention among health workers.
Therefore, this study aimed to assess practice and its associated factors of infection prevention among Health workers at the Wachemo University Compressive Specialized Hospital, South Ethiopia.
Study Area and study period
The study was conducted at WCUNEMMCSH, which is found in Hadiya Zone, Southern Nations Nationalities, and People’s Regional State (SNNPR), Ethiopia. Hosanna Town is one of the largest towns in the Southern Nation Nationalities and People Region (SNNPR), which is the capital of the Hadiya Zone. It is found 230 KM from Addis Ababa and 168 KM from Hawassa, the capital city of the SNNPR. The Hadiya zone contains an estimated 2 million people. In the zone, there are 65 health centers, three district hospitals, and one comprehensive specialized hospital. WCUNEMMCSH has established in 1976 E.C. It has around 18 outpatient departments. It supports three district hospitals and 65 health centers. In addition to teaching the students, those at WCUNEMMCSH provide preventive, curative, and rehabilitative clinical services structured into four case teams in outpatient, inpatient, emergency, and maternal and child health. The study was conducted from July 15 to July 30, 2022.
Study design
A facility-based cross-sectional study was conducted among Health care workers who work at WCUNEMMCSH in Hadiya Zone, Southern, Ethiopia
Source population
All Health Care Workers who were worked at WCUNEMMCSH in Hadiya Zone, Southern, Ethiopia, 2022
Study population
All selected Health Care Workers who were worked at Wachemo University Comprehensive Specialized Hospital and available during the data collection period.
Inclusion and Exclusion Criteria
All Health Care Workers who had work experience 6 months and above during the data collection period were included in the study, while Health care workers who had been given free service and were seriously ill during the data collection period were excluded.
Sample size determination
To determine the sample size, the outcome variable and factors that are significantly associated with the outcome variable were considered. The sample size was calculated separately then the larger sample size had been taken. For the prevalence of infection prevention practice, the sample size was calculated using a single population proportion formula. The desired sample size for this study was estimated by taking the prevalence of good infection prevention practices among HCWs (66.1%) from a previous study conducted in Addis Ababa.12 Assuming a 95% confidence level, and a 5% margin of error as follows;
n = the minimum sample size required, p= estimated proportion of infection prevention practice=0.661 z = the standard value of confidence level of α=95% d = the margin of error between the sample and the population (0.05).
Z=1.96, P =0.661%, d = 5% =0.05,
By considering 10% for the non-response rate the final sample size for specific objective one was 379.
The sample size of the second specific objective was determined by considering factors that are significantly associated with the outcome variable,13 the two-sided confidence level of 95%, power of 80%, and the ratio of exposed to unexposed 1:1 using Epi Info Version 7.2.2.6 and the calculated sample size for the selected factors were shown in the table below: (Table 1)
|
Factors Associated with infection prevention practices |
% of non-exposed |
% of exposed |
% CI |
Power |
Allocation |
Total sample size |
|
Knowledge of infection prevention practice AOR=2.21(1.32, 3.71) |
24.4 |
57.7 |
95 |
80 |
1:01 |
78 |
|
The attitude of nurses toward infection prevention practices AOR= 5.11 (3.05, 8.57) |
20.4 |
35.1 |
95 |
80 |
1:01 |
316 |
|
Infection prevention training AOR 2.22(1.29, 3.82) |
23.8 |
65.5 |
95 |
80 |
1:01 |
52 |
|
Educational status AOR= 2.52(1.14, 5.54) |
14.3 |
45.9 |
95 |
80 |
1:01 |
76 |
|
PPE availability AOR 2.57(1.46, 4.49) |
24.4 |
66.5 |
95 |
80 |
1:01 |
52 |
Table 1 Sample size determination for infection prevention practice and associated factors among healthcare workers working at WCUCSH 2022
Finally, the required sample size for this particular study is decided by taking the maximum sample size (i.e. first specific objective=344) from the calculated sample size. Then, by considering, 10% non-response rates, the final sample size became 379.
Sampling technique and procedure
The sample was selected from Wachemo University Comprehensive Specialized Hospital, after getting a sampling frame of eligible participants for this study from human resources. First, an estimated sample size (n) was divided by the total surveyed number of Health Care Workers (N) which yielded a proportionate value (p). Secondly, a proportionate value was multiplied by the total number of HCWs in each profession at WCUNEMMCSH which yielded a proportionate value for each profession. Finally, a simple random sampling technique was used to obtain the required sample from each profession. (Figure 1)
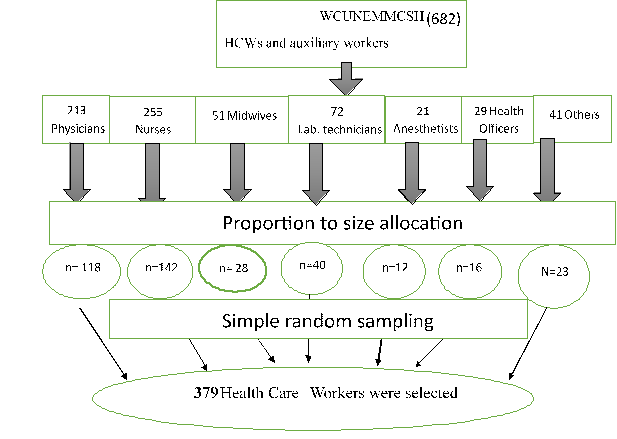
Figure 1 Sampling procedure for selecting study participants from Wachemo University Comprehensive Specialized Hospital, 2022.
Operational definition
Good practice was HCW who scored the mean and above from the provided question regarding infection prevention practice.14
The poor practice was HCW who scored the less than mean value from the provided question regarding infection prevention practice.14
Good knowledge was HCW who scored the mean and above from the provided question regarding infection prevention.14
Poor knowledge was HCW who scored the less than mean value from the provided question regarding infection prevention.14
The positive attitude was HCW who scored the mean and above from the provided question regarding infection prevention.14
The negative attitude was HCW who scored the less than mean value from the provided question regarding infection prevention.14
Data collection instrument
A self-administered questionnaire was used which is adapted from structured questionnaires from different literature.11,15,16 A pre-test was carried out on the 5% of a sample size of HCWs who are working at Worabe compressive specialized hospital for clarity of questions, to eliminate repetitive and ambiguous questions as well as consistency of understanding the survey tool then based on the result obtained, the necessary modification will be made accordingly. The reliability test was performed for the knowledge, attitude, and practices component of questions. The tools contain 52 questions which were designed to cover the following sub-sections;-sociodemographic characteristics, organization-related factors, knowledge-measuring questions, attitude-measuring questions, and infection prevention practices measuring questions.
Data collection procedure
The data was collected by two B.Sc. nurses and supervised by the principal investigator. The data collectors were trained for one day by the principal investigator about the purpose of the study, tools, and field methods. The data collector collected data after obtaining informed consent from study participants, and then distributed structured self-administered questionnaires for each enrolled study participant using simple random sampling methods.
Data quality control
To maintain data quality by using an adapted questionnaire from published research. A pre-test was carried out on 5% of a sample size of HCWs who are working at Worabe compressive specialized hospital. One day of training was given to data collectors regarding data collection tools and procedures of data collection. Data collectors were supervised by the principal investigator. The reports were received regularly by the principal investigator. The completeness of the data was checked by data collectors during data collection. Simple frequencies and cross-tabulation were done for missing values and crosschecked with hard copies of the collected data.
Data processing and analysis
The data were coded and then enter into Epi-data version 4.6v software final export to SPSS version 25 for analysis. The collected data were checked for completeness and consistency and cleaned after entry into a computer. Different dummy tables, graphs, and descriptive summaries were used to present the study variables. Binary Logistic regression was performed to assess the strength of the association between each independent variable and the outcome variables. Bivariate analysis perform for variable selection so those variables with P value < 0.25 were fitted into multivariable binary logistic regressions. Model fitness was checked by the Hosmer and Lemeshows goodness of fit test which was found to be 0.57. Finally, only those independent variables that maintain their association with outcome variables in multivariable logistic regressions (p-value <0.05) were used to construct the final models. The odds ratio with its p-value and confidence interval were reported in each logistic regression analysis. For measuring the strength of the association between the outcome and independent variables, Crude Odd Ratio (COR) and Adjusted Odd Ratio (AOR) along with a 95% Confidence interval (CI) were calculated.
Ethical considerations
Ethical clearance was obtained from the institutional ethical review board of the College of Medicine and health sciences. An official support letter was given to WCUNEMMCSH. Oral and written informed consent was obtained from each study participant. Each participating HCW was informed about the purpose of the study. No personal identification of the study participant was recorded to ensure confidentiality.
Socio-demographic characteristics of study participants
From the total of 379 study participants, 366 healthcare workers returned the research questionnaires with a response rate of 96.5%. The mean age of the participants was 29.5 ±4.5 years. The majority of the participants (51.6%) were found between the ages of 27 and 31 years. Nearly half of the respondents, 193 (52.7%), had BSc degree holders. Most of the study participants 246(67.2%) had five years and blow work experience. Concerning the average monthly income of respondents, 142 (38.8) % of study participants would have earned less than or equal to 6,200 Ethiopian birrs (Table 2).
|
Variables |
Category |
Frequency(N) |
Percent (%) |
|
Sex |
Male |
250 |
68.3 |
|
Female |
116 |
31.7 |
|
|
Age |
22-26 years |
104 |
28.4 |
|
27-31 years |
189 |
51.6 |
|
|
32-36 years |
38 |
10.4 |
|
|
≥ 37 Years |
35 |
9.6 |
|
|
Marital status |
Single |
175 |
47.8 |
|
Married |
191 |
52.2 |
|
|
Profession |
Nurses |
142 |
38.8 |
|
Midwife |
28 |
7.7 |
|
|
Physician |
114 |
31.1 |
|
|
Laboratory |
38 |
10.4 |
|
|
Anesthetists |
12 |
3.3 |
|
|
Health officers |
12 |
3.3 |
|
|
Other professionals |
20 |
5.5 |
|
|
Educational status |
Diploma |
17 |
4.6 |
|
BSc degree |
193 |
52.7 |
|
|
Medical doctors |
111 |
30.3 |
|
|
MSc/MPH |
45 |
12.3 |
|
|
Work experience |
Less than or equal to 5 years |
246 |
67.2 |
|
Greater than 5 years |
120 |
32.8 |
|
|
Working units |
Emergency |
47 |
12.8 |
|
Pediatrics wards |
27 |
7.4 |
|
|
Medical wards |
35 |
9.6 |
|
|
Surgical wards |
33 |
9 |
|
|
Operation room |
45 |
12.3 |
|
|
NICU |
20 |
5.5 |
|
|
ICU |
26 |
7.1 |
|
|
OPD |
24 |
6.6 |
|
|
MCH |
43 |
11.7 |
|
|
Laboratory department |
37 |
10.1 |
|
|
Other units |
29 |
7.9 |
|
|
Average monthly income |
≤ 6200 |
142 |
38.8 |
|
6201-8017 |
85 |
23.2 |
|
|
>8018 |
139 |
38 |
Table 2 Socio-demographic characteristics of healthcare workers who working at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
Organizational Factors for infection prevention
Of the total study participants, 45.1% of respondents said that their institution had an accessible with soap and water. However, only 16.7% of HCWs respond that a consistent water supply is accessible daily in their institution. Concerning infection prevention training, 36.1 % of HCWs get in-service trained hand-washing stationing. Most of the study participants (66.4%) were aware of infection prevention and control guidelines that exist in their institution, however, 45.4% of study participants had access to documents (Table 3).
|
Organization Related Questions |
Frequency(N) |
Percent (%) |
||
|
Hand washing station with running water and soap |
No |
201 |
54.9 |
|
|
Yes |
165 |
45.1 |
||
|
Consistent water supply daily |
No |
305 |
83.3 |
|
|
Yes |
61 |
16.7 |
||
|
In-service training/ workshop related to infection prevention and control? |
No |
234 |
63.9 |
|
|
Yes |
132 |
36.1 |
||
|
How long ago did you take infection prevention training?
|
≤ 6 month |
26 |
7.1 |
|
|
6 months – 1 year |
23 |
6.3 |
||
|
Greater than 1years |
83 |
22.7 |
||
|
Staff adherence to infection prevention practices is monitored by infection prevention committees |
No |
155 |
42.3 |
|
|
Yes |
211 |
57.7 |
||
|
Adequate supplies of resources (sterile needles and syringes, gloves, sharp containers, disinfectants, hand sanitizers, etc.) to work within your department |
No |
221 |
60.4 |
|
|
Yes |
145 |
39.6 |
||
|
Personal protective equipment accessible |
No |
218 |
59.6 |
|
|
Yes |
148 |
40.4 |
||
|
Be aware of the existence of infection prevention and control guidelines in your institution. |
No |
123 |
33.6 |
|
|
Yes |
243 |
66.4 |
||
|
Do you have access to the document/guideline |
No |
78 |
21.3 |
|
|
Yes |
166 |
45.4 |
||
|
I am not able to follow standard precautions frequently due to |
High |
202 |
55.2 |
|
|
workloads |
||||
|
don’t have |
132 |
36.1 |
||
|
enough time |
||||
|
Forgetfulness |
107 |
29.2 |
||
|
Others |
45 |
12.3 |
||
|
I am vaccinated against the Hepatitis B virus |
No |
115 |
31.4 |
|
|
Yes |
251 |
68.6 |
||
|
The reason for not being vaccinated against the hepatitis B virus |
The facility did not provide an opportunity |
73 |
19.9 |
|
|
Refuse to take |
30 |
8.2 |
||
|
vaccination |
||||
|
|
12 |
3.3 |
||
Table 3 Organization-related factors infection prevention practices among healthcare workers working at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
Knowledge of health care workers towards infection prevention
There was 18 knowledge measuring questions concerning infection prevention which were computed to determine healthcare workers’ knowledge of infection prevention. Then HCW knowledge of infection prevention was classified by using a mean score (12.7) of study participants. The mean and standard deviation of HCW knowledge on infection prevention were found to be 12.7 ± 2.66 respectively. As a result, 60.1% (95% CI: 55.0%, 65.1%) of HCWs had adequate knowledge of infection prevention (Figure 2).

Figure 2 Knowledge of infection prevention among healthcare workers who work at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022.
The attitude of healthcare workers toward infection prevention
Nearly half of the respondents 174(47.5%) agree with nosocomial infections pose a serious outcome and also
180(49.2%) of the study participants respond they could transmit nosocomial infections. Concerning compliance with the recommended guidelines, 224(61.2%) of respondents agree with the opinion of being more compliant with the recommended guidelines for reducing the transmission of a nosocomial infection when training new workers. Only 14(3.8%) of respondents strongly disagree with the opinion of healthcare workers should be rewarded for compliance with protocols (Table 4).
|
Attitude related questions |
Strongly disagree |
Disagree |
Neutral |
Agree |
Strongly agree |
|
In my opinion, nosocomial infections pose a serious outcome |
9(2.5%) |
20(5.5%) |
15(4.1%) |
174(47.5%) |
148(40.4%) |
|
In my opinion, I could transmit nosocomial infections. |
19(5.2%) |
29(7.9%) |
15(4.1%) |
180(49.2%) |
123(33.6%) |
|
In my opinion, HCWs respond negatively when a colleague is non-compliant with the recommended guidelines for patient safety. |
21(5.7%) |
21(5.7%) |
29(7.9%) |
233(63.7%) |
62(16.9%) |
|
I am more compliant with the recommended guidelines for reducing the transmission of a nosocomial infection when training new workers. |
12(3.3%) |
18(4.9%) |
17(4.6%) |
224(61.2%) |
95(26.0%) |
|
I serve as a role model in demonstrating adherence to recommended practices for hand hygiene. |
4(1.1%) |
17(4.6%) |
20(5.5%) |
233(63.7%) |
92(25.1%) |
|
It is unrealistic to expect healthcare workers to clean their hands after every contact with the patient. |
41(11.2%) |
29(7.9%) |
24(6.6%) |
218(59.6%) |
54(14.8%) |
|
In my opinion, healthcare workers should be legitimate for non-compliance with protocols for reducing transmission of nosocomial infections |
23(6.3%) |
58(15.8%) |
50(13.7%) |
145(39.6%) |
90(24.6%) |
|
In my opinion, healthcare workers should be rewarded for compliance with protocols aimed at reducing the transmission of nosocomial infections. |
14(3.8%) |
22(6.0%) |
36(9.8%) |
149(40.7%) |
145(39.6%) |
Table 4 The Health Care Workers’ responses to each attitude measuring question towards infection prevention at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
There were 8 attitude-measuring questions concerning infection prevention which were computed to determine healthcare workers’ attitudes toward infection prevention. Then HCW attitude toward infection prevention was classified by using a mean score of study participants. The mean and standard deviation of HCW attitude towards infection prevention were found to be 6.4 ±1.57 respectively. As a result, 209 (57.1%) with (95% CI: 52.0%-62.2%) of HCWs had a positive attitude toward infection prevention (Figure-3).
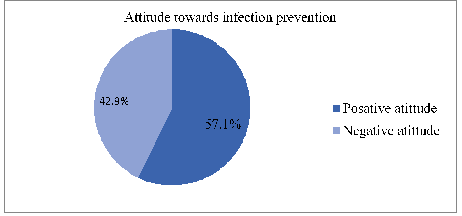
Figure 3 Attitude towards infection prevention among healthcare workers who working at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022.
Infection prevention practice
From the totals of study participants, 38.3% of HCWs washed their hands with soap under running water in the working units, however only 29.0% of HHCWs removed their rings, watches, or bracelets before beginning hand hygiene. Despite the majority of research participants (74.9%) disposing of sharp materials in a safety box, only 42.9% of respondents recap needles before disposal and about 38.0% of HCWs use the same waste container for infectious waste and non-infectious waste (Table 5).
|
No |
Practice measuring questions |
Yes |
No |
|
1 |
I always wash my hands with soap under running water in my unit. |
140(38.3%) |
226(61.7%) |
|
2 |
On removal of gloves, I always wash my hands after contact with a patient or body fluid. |
185(50.5%) |
181(49.5%) |
|
3 |
Disposable items (like gloves) are used once and discarded in my unit. |
218(59.6%) |
148(40.4%) |
|
4 |
I follow recommended guidelines for the use of alcohol-based solutions or other antiseptics before and after helping the patient to move, or lifting I transfer the patient in and out of bed |
212(57.9%) |
154(42.1%) |
|
5 |
I wash my hands before and after invasive procedures. |
227(62.0%) |
139(38.0%) |
|
6 |
I remove my ring(17), watch, or bracelet before beginning hand hygiene |
106(29.0%) |
260(71.0%) |
|
7 |
I discard sharp materials in a safety box |
274(74.9%) |
92(25.1%) |
|
8 |
I recap needles before disposal |
157(42.9%) |
209(57.1%) |
|
9 |
I wear goggles and a mask when performing invasive and body fluid procedures |
189(51.6%) |
177(48.4%) |
|
10 |
I cover wounds and cuts on my skin before I start my work |
204(55.7%) |
162(44.3%) |
|
11 |
I carry out disinfection often in the working area and ensure that all instruments are decontaminated after each use |
203(55.5%) |
163(44.5%) |
|
12 |
I use the same waste bin for infectious waste and non-infectious waste |
139(38.0%) |
227(62.0%) |
Table 5 The HCW responses to each question regarding infection prevention practices at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
There were 12 infection prevention measuring questions that were computed to determine HCW infection prevention practices. Then the mean score (6.4) of study participants was used to classify HCW infection prevention practices. As a result, 168(45.9%) of HCWs (95% CI: 40.7%-51.0%) had good infection prevention practices (Figure 4).
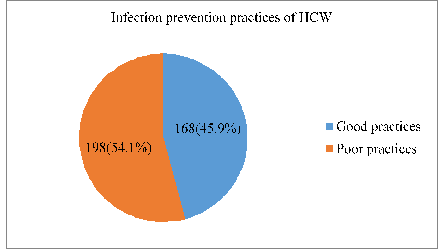
Figure 4 Infection prevention practices among healthcare workers who work at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
Factors associated with infection prevention practices
Bivariate logistic regression analysis was used to evaluate various variables. Thus, the age of respondents, marital status, work experiences, in-service training on infection prevention, presence of a hand washing station, consistent water supply, adequate material supplies, awareness of the existence of IP guidelines in the institution, availability of personal protective equipment and attitude towards infection prevention were all variables with P values less than 0.25 were fitted into the multivariable logistic regression model. However, on multivariable analysis, work experiences, in-service training on infection prevention, and awareness of the existence of IP guidelines in the institution were significantly associated with good infection prevention practices.
The odds of having good infection prevention practices were 4.48 times higher for HCWs who had more than 5 years of work experience when compared with counterparts (AOR: 4.48, 2.45-8.16). The odds of having good infection prevention practices were 2.17 times higher for HCWs who had in-service training about IP when compared with counterparts (AOR: 2.17, 1.30-3.63). The odds of having good infection prevention practices were 5.59 times higher for HCWs who had awareness of the existence of IP guidelines in their institution when compared with counterparts (AOR: 5.59, 3.14-9.92) (Table 6).
|
No |
List of the independent variable |
IP practices |
COR (95%CI) |
AOR (95%CI) |
P value |
||
|
Good |
Poor |
||||||
|
1
|
Age of respondents |
22-26 years |
42 |
62 |
1 |
1 |
|
|
27-31 years |
78 |
111 |
1.03(0.63-1.68) |
0.61(0.33-1.10) |
0.1 |
||
|
32-36 years |
21 |
17 |
1.82(0.86-3.86) |
1.08(0.43-2.73) |
0.86 |
||
|
≥ 37 years Unmarried |
27 73 |
8 102 |
4.98(2.06-12.0) |
2.09(0.76-5.73) |
0.15 |
||
|
2 |
Marital status |
|
1.38(0.91-2.9) |
1.01(0.60-1.67) |
0.97 |
||
|
Married |
95 |
96 |
1 |
1 |
|||
|
3 |
Work experiences |
≤ 5 years |
87 |
159 |
1 |
1 |
|
|
3.79(2.38-6.03) |
4.48(2.45-8.16) |
0.00* |
|||||
|
4 |
In-services training on IP |
> 5 Years |
81 |
39 |
1 |
1 |
|
|
No |
95 |
139 |
|||||
|
Yes |
73 |
59 |
|||||
|
1.81(1.17-2.78) |
2.17(1.30-3.63) |
0.00* |
|||||
|
5 |
Presence of a hand washing station with soap and water |
No |
81 |
120 |
1 |
1 |
|
|
Yes |
87 |
78 |
1.65(1.09-2.50) |
1.02(0.51-2.03) |
0.93 |
||
|
6 |
Consistent water supply |
No |
135 |
170 |
1 |
1 |
|
|
Yes |
33 |
28 |
1.48(0.85-2.57) |
1.01(0.48-2.12) |
0.98 |
||
|
7 |
Adequate material supplies for IP |
No |
92 |
129 |
1 |
1 |
|
|
Yes |
76 |
69 |
1.54(1.01-2.35) |
1.27(0.64-2.50) |
0.48 |
||
|
8 |
Awareness of the existence of IP guideline |
No |
28 |
95 |
1 |
1 |
|
|
Yes |
140 |
103 |
4.61(2.81-7.54) |
5.59(3.14-9.92) |
0.00* |
||
|
9 |
Availability of PPE |
No |
86 |
132 |
1 |
1 |
|
|
Yes |
82 |
66 |
1.90(1.24-2.91) |
1.58(0.95-2.63) |
0.07 |
||
|
10 |
Attitude toward infection prevention |
Negative |
59 |
98 |
1 |
1 |
|
|
Positive |
109 |
100 |
1.81(1.18-2.76) |
1.34(0.81-2.21) |
0.24 |
||
Table 6 Logistic regression analysis of factors associated with infection prevention practices among healthcare workers working at WCUNEMMCSH, Hadiya zone Southern, Ethiopia 2022
Note* Indicate significant variables, IP = Infection Prevention, PPE = Personal Protective Equipment
In this study, the proportion of HCWs who had good practices was found to be 45.9% which is comparable with previous similar and related studies conducted in, Nigeria 50.8%,18 Ghana 45.1%,19 Ethiopia 42.9%.20 However, this study finding was higher than in many similar and related studies conducted in Bangladesh 36%21 and Iran 34%.9 The discrepancy might be due to differences in sample size, study period, and study subject. Iran study, practices level was classified under three categories like fair, moderate, and good practices towards infection prevention, and the study was conducted on only nurses.
On the other hand, the finding of this study was lower than studies conducted in Rivers State at 59%,22 Kosovo at 76.2%,23 Rwanda at 64.5%,24 Lesotho at 63.6%,25 Ethiopia at 57.4%,26 57.3%,27 60.5%28 and 65%,29 55.0%30 and 66.1%.12 The discrepancy might be due to differences in sample size, study period, and study participants and area. As compared to Kosovo, Ethiopia was a low-income country so poor practice of HCW towards infection prevention due to lack of training on infection prevention, lack of adequate supplies of materials and hand washing stations, and other infrastructure problems could be possible explanations.
When compared to HCWs with work experience of 5 years or less, those with more experience were more likely to follow good infection prevention practices. This finding is in line with the study done in Bahir Dari,10 Ethiopia, however, this finding is inconsistent with the study done in Mekele Ethiopia.31 The fact that those HCWs with high work experience had greater compliance to standard precaution practices due to their participation in a greater number of seminars, conferences, and training which include standard precaution practices which not only encouraged safer work practices but also improved concordance with policy and procedures.29
The odds of having good infection prevention practices were higher among HCWs who take in-service training about IP when compared to HCWs who did not take part in in-service training about it. This study's findings were supported by the study conducted in Debre Markos Ethiopia.27 This association may be explained by the fact that healthcare professionals who receive training in infection control techniques have a great opportunity to understand the benefits of infection control and may have learned essential information that enables them to use infection control techniques with potentially available materials to avoid the negative effects of infectious diseases on the healthcare system and patients. In addition, having current knowledge and proficiency in infection prevention may give HCWs more confidence to follow suggested standards. The odds of having good infection prevention practices among HCWs who had awareness of the existence of IP guidelines in their institution were more likely compare with HCWs who hadn’t awareness of the existence of IP guidelines. This finding is consistent with a study conducted in West Arsi (Ethiopia) and North Ethiopia.20,32 The ability of WCH who are aware of the IP guideline to obtain the material enhances their knowledge of preventing infection.
Limitation
Social desirability bias might be introduced due to self-reporting practices measuring tools and attitudes towards infection prevention studied quantitatively by using the Likert scale which might doesn’t explore adequate attitude concern towards infection prevention.
According to the findings, nearly half of the healthcare workers had good infection prevention practices. Having more than five years of work experience, taking in-service training on infection prevention and awareness of the existence of IP guidelines in the institution were all significant factors associated with good infection prevention practices.
The implication of the study
Education and training resulting in practice are important for all Health care workers in infection prevention. This is particularly important for critically ill patients where care activities are performed for susceptible patients. This research shows that healthcare workers who had training and a higher level of education have a good performance in Infection prevention. Strengthening supportive training and exposure to Infection prevention control can have an effect on health policy, change practice, and safe patient care as a whole.
None.
The authors declare no conflict of interest.

©2023 Tumdado, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.