MOJ
eISSN: 2379-6383


Mini Review Volume 5 Issue 3
Department of Medical Laboratory Sciences, School of Allied Health Sciences, University of Cape Coast, Ghana
Correspondence: David Larbi Simpong, Department of Medical Laboratory Sciences, School of Allied Health Sciences, University of Cape Coast, Ghana
Received: September 30, 2016 | Published: March 7, 2017
Citation: Adu P, Simpong DL. Addressing the challenge of iodine deficiency in developing countries. MOJ Public Health. 2017;5(3):89–91. DOI: 10.15406/mojph.2017.05.00129
Iodine deficiency causes stunted physical and mental growth as well as infertility, lethargy and cognitive impairment. Although iodine deficiency is endemic in most countries and is therefore a public health issue, it is preventable through adequate intake of iodine in diet. Recent global data estimated that 1.88billion people are at risk of iodine deficiency with 241 million children taking inadequate iodine in diet. Majority of these children with inadequate dietary iodine intake lives in Africa and South/South-East Asia. Gains have been made towards the eradication of iodine deficiency disorders (IDDs) through the universal salt iodisation (USI) programme which has ensured greater coverage of iodine intake throughout the world. In developing countries however, the perennial problem of weaker institutions means that much needs to be done if the goal of eradicating IDDs are to be realized. This mini-review looks at what steps could be undertaken to maximize the odds of eradicating IDD through food fortification, strengthening of regulatory institutions, empowering small-scale salt manufacturers and conscientization of the populace to patronise not only iodized salt but also iodine-fortified foods.
Keywords: iodine deficiency disorder, universal salt iodisation programme, cretinism, thyroxin
USI, universal salt iodisation; IDD, iodine deficiency disorder; RTK, rapid test kit; T3, triiodothyronine; T4, thyroxin
Iodine is an essential micro-nutrient necessary for the formation of thyroid hormones [T3 (triiodothyronine) and T4 (thyroxin)]. As thyroid hormones regulate proper neuronal development, deficiency of iodine can have grave consequences especially when it occurs during pregnancy as it negatively affects foetal and subsequent neonatal life leading to irreversible cognitive impairment.1–3 Primarily, iodine deficiency is caused by inadequate dietary supply. The plethoras of disorders caused by iodine deficiency are collectively called iodine deficiency disorder (IDD), the most prominent of which are goitre and cretinism. In line with these devastating and irreversible adverse health implications of iodine deficiency, the WHO recommended the adoption of the universal salt iodisation (USI) programme4 to help eliminate this nutritional deficiency. In addition to this, most countries have adopted fortification of foods such as oils either as alternative iodine source or to augment the USI initiative.5,6 However, the salt fortification programme has many advantages as salt is used by almost everybody and therefore overcome the issue of logistics required for the dissemination of other forms of iodine supplementation approaches. Not surprisingly, most developing countries mainly rely on the USI programme to meet iodine needs of the populace. Although empirical evidence shows that effective implementation of the USI programme offers undisputed prospect towards eliminating iodine deficiency, IDD is still prevalent in most developing countries. For example, the WHO Global database on iodine deficiency show that in some parts of Cote d'ivoire, Egypt, Nigeria, and Ghana, prevalence of iodine insufficiency could be as high as33.8%, 31.2%, 42% and 71.3% respectively.7 Furthermore, the WHO recently estimated the regional averages of household consumption of adequately iodized salt to be 50%, 59%, 65, and 69, for least developed countries, Sub-Saharan Africa, West and Central Africa, and South Asia respectively (Figure 1).8
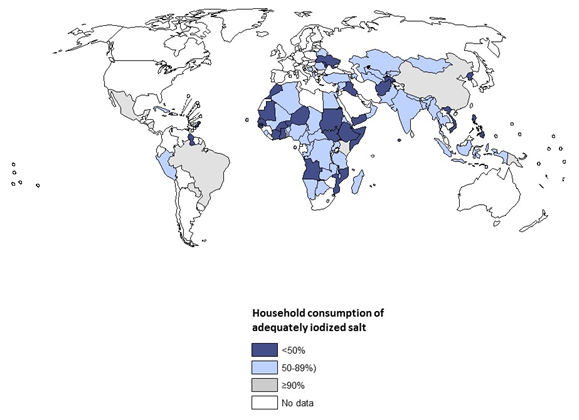
Figure 1 Global picture of the household consumption of adequately iodized salt. (Source: Iodized Salt Consumption SOWC; UNICEF (http:// data.unicef.org/nutrition/iodine.html; Accessed October 2014.
This calls for some serious consideration for the evaluation and monitoring of the implementation of the USI programme in these developing countries. Most of these countries have weak institutions with inadequate infrastructures necessary for effectively assessing the iodine levels in the supposedly iodized salts on offer. To our knowledge, ensuring adequacy of salt iodisation may be the critical component in the chain of measures necessary to actualise the goals of the USI programme. This salt iodisation and subsequent storage conditions may need some critical evaluation to ensure that any gains made in the USI initiative are not derailed. Authorities in these developing countries must invest in their respective regulatory agencies tasked with ensuring that quality standards are met by salt producers before these iodized salts are released onto their respective markets. Based on the daily iodine requirement, estimated average salt intake of 10g/day, as well as estimated iodine losses during production and consumption,9 the WHO recommends the incorporation of 20 to 40 parts per million (ppm) of iodine to salt at the point of production.10 Thus the existing regulatory agencies must be empowered to ensure that the salts on their respective markets meet these basic quality standards. Rapid test kits (RTKs) have revolutionized the diagnosis and management of malaria even in remote communities. Although RTKs have also been developed for quantitative iodine measurements,11,12 there is urgent need for optimization of iodine RTKs13 to provide accurate quantitative estimates of iodine in salts that would empower regional and district level regulatory agencies to properly monitor the USI programme. It must be pointed out that these monitoring and evaluation processes should be periodic so as to ensure that iodine levels are consistently maintained within safe and optimal limits.
Way forward
Public education through radio, television, whatsapp and other social network platforms must be given priority so as to properly sensitize the populace with regards to the adverse health implications of IDDs. Such public educational campaigns have previously shown successful in countries.14 Any such educational programmes should also conscientize the populace about the proper storage conditions and use of these iodized salts. In our experience, the iodized salts sold in most developing countries are in polythene bags where consumers cut openings to ease salt dispensation (Simpong & Adu, unpublished observations). As these openings are never closed, it is a feasible supposition that the high ambient temperature and humidity/moisture prevailing in these tropical countries may cause iodine levels in the salts to wane with the passage of time.15,16 These unfortunate practices on the part of consumers inadvertently negate any investment made by the iodized salt manufacturers. This could be prevented by encouraging salt manufacturers to package their products in easy to reseal cartons and/or re-sealable plastic containments. Additionally, there may also be the need to include community health nurses and disease control officers to drive these community-based educational programmes. The successes enjoyed by the Global Polio eradication Initiative17,18 where these health professionals routinely canvas the cooperation of even the remotest communities should be ample evidence that their inclusion in any IDD eradication campaigns may guarantee some meaningful gains. In spite of the many years that has passed since the introduction of the USI programme, many published data indicates that a considerable number of people are not using iodised salt.19,20 Much as these data are helpful, most of them offer only snapshots of iodine status of segments of the population at different geographic locations in these IDD regions. Interestingly, Juan et al.,21 demonstrated that to obtain a reliable estimate of iodine status of any population, consideration should be given to the dietary iodine intake from all food sources in addition to the UIC measurements.21 It is imperative for governments and heads of state of these IDD regions to demonstrate commitment to the IDD eradication by annually devoting portions of national health budgets for continuous surveillance and monitoring of the USI programme. Such funds should be used purposely to encourage a concerted research to provide regional and ultimately national iodine status estimates to inform intervention strategy formulation. These population-based research/surveillance studies could effectively use the UIC22 to provide credible data on present iodine status to inform intervention strategies as well as attract funding from the WHO and other international agencies (e.g. UNICEF, UNDP, Swedish International Development Authority-SIDA and USAID) to complement local governmental efforts. Even though serum thyroid stimulating hormone, serum thymoglobulin and serum T4 measurements offer alternative ways of assessing iodine status, these alternative approaches are invasive, not feasible in population scale monitoring studies and their usefulness in certain population groups have been questioned.23,24
Example of such fruitful governmental-international body partnership is the GAIN (Global Alliance for Improved Nutrition)-UNICEF USI Partnership Project in Indonesia that aims to make iodized salt readily available to Indonesians.25 Moreover, Ecuador provides a clear argument for the effectiveness of joint enterprise between governments and international partners in the fight against IDDs. Although Ecuador had a high prevalence of goitre and cretinism in the 1950s, it has practically eliminated these disorders through such vibrant partnership between the Ecuadorian and Belgian governments.14 Additionally, portion of these nationally devoted budgets must also be used to build the capacity of small scale salt manufacturers who produce cheap non-iodized salt alternatives especially in countries such as India, Ghana, and Indonesia.25–27 As these small-scale salt producers do not have the capacity to iodize their salt, these funds should aim to build their infrastructural capacity so as to realise the goal of universal iodisation of all salts on the markets. A recent study in Ghana and Sierra Leone respectively found that 33% and 20% households were not using iodized salt.19,20 Taking measures to prevent availability of non-iodised salt on the market is crucial as a recent adjusted logistic regression analysis demonstrated a 3% higher odd of stunted growth with non-availability of iodized salt.28 Empowering the small-scale salt producers in this way would help obviate the lack of adherence to the ban on non-iodized salt usage in certain countries like India.26,29 Moreover, food fortification programmes must also be given serious consideration by these developing countries to increase the odds of eliminating iodine deficiency scourge. Bread, cooking oils, and rice are staple foods in most of these communities have been successfully iodized in certain countries.14,30 Countries like Australia and New Zealand have implemented mandatory food fortification with iodine that have significantly improved the iodine levels of people in these countries.31 In the United States also, cow milk,32 and chicken eggs33 contain iodine that may supplement what may be ingested through iodized salt. Therefore, efforts must be made to iodize foods such as bread, cooking oils, rice and even water in these developing countries to offer a multi-faceted approach so as to maximize the chances of eliminating IDDs. A recent study demonstrated that fortification of vegetable oil with other micronutrient such as vitamin A and iron improved the nutritional status in the study participants.34 An additional advantage offered by fortification of these other vehicles is the prevention of hypertension associated with increased salt intake.
Eradication of IDD the USI initiative is attainable only through a concerted effort by governments, international funding bodies, and salt producers coupled with sustained education of consumers to motivate them to utilize these iodized salts.
None.
The author declares no conflict of interest.

©2017 Adu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.