MOJ
eISSN: 2574-8130


Case Report Volume 5 Issue 5
Department of Neurosurgery-Neurology, UNIFESP - São Paulo Federal University, Brazil
Correspondence: Isaque Hyung Tong Kim, Department of Neurosurgery-Neurology, UNIFESP - São Paulo Federal University, Brazil, Tel +5511961948239, Tel +55119995520197
Received: September 14, 2020 | Published: September 29, 2020
Citation: Kim IHT, Onishi FJ, Cavalheiro S, et al. Tips for diagnosing subdural collections in the elderly. Case report and literature review. MOJ Gerontol Ger. 2020;5(5):157?158. DOI: 10.15406/mojgg.2020.05.00249
Cerebral atrophy is a natural phenomenon of aging. However, the subdural space of the elderly is usually affected by different diseases. Treatment can vary, from a clinical segment with the observation of spontaneous absorption of the subdural collection, to the need for urgent surgical treatment by a neurosurgeon. The cerebral atrophy situation can present itself as a differential diagnosis of lesions with a mass effect on the cerebral parenchyma. The combination of clinical and radiological findings allows us to increase the accuracy of the correct diagnosis. We present a clinical case followed by a brief discussion on tips that can assist in the differential diagnosis.
A 71-yo male has referred to our institution after a history of fall from his height 2 months ago. His medical history revealed hypercholesterolemia regularly treated with a statin and urinary incontinence. He reported an important headache and progressive weakness of the right arm and leg, associated with behavior change, spatial disorientation, and memory loss complaint. He denied fever symptoms.
Clinical examination showed a confused patient, Glasgow Coma Scale 14, isochoric pupils, muscular strength grade 5on the left side, and grade 3 onthe right arm and leg, without signs of meningeal irritation. His laboratory blood tests did not show any changes, including coagulation tests. He was referred for a CT scan exam (Figure 1) (Figure 2).
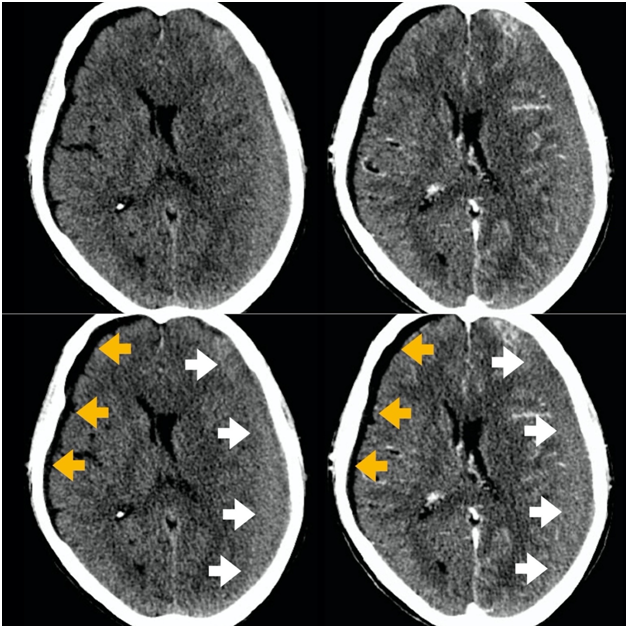
Figure 1 ACT scan without and with intravenous contrast - axial view. A bilateral subdural lesion was diagnosed. A hypodense subdural hygroma on the right side (orange arrows). On the left side,we can see an isodense chronic subdural hematoma (white arrows). Note the midline shift due to the chronic subdural hematoma mass effect.
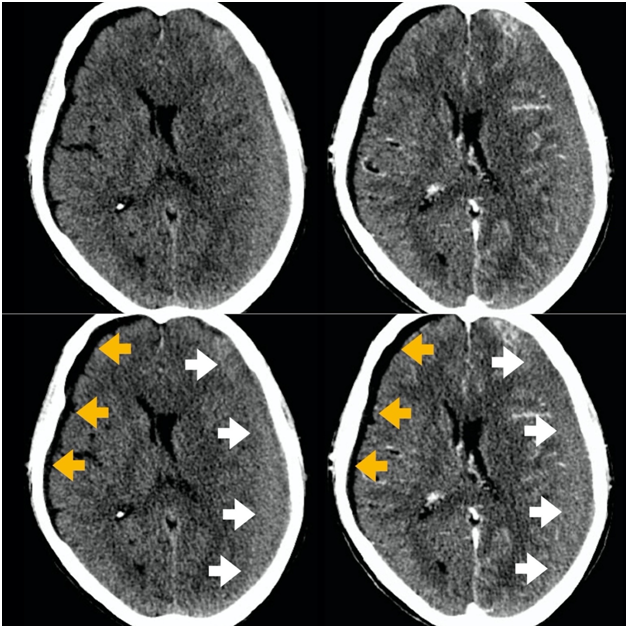
Figure 2 CT scan without and with intravenous contrast, axial view. On the right side of the patient, we can see the spared cerebral sulci and no cortical veins inside the hygroma(orange arrows). On the left side, the sulci are compressed by the chronic subdural hematoma (white arrows).
The patient was promptly submitted to the surgical treatment of the left side subdural hematoma and had recovery from neurological symptoms uneventfully.
Due to the effects of cerebral age atrophy, the subdural space is usually enlarged in the elderly. In addition to analyzing the subdural collection itself, we need to be aware of the adjacent cortical grooves and eventually use intravenous contrast injection to better characterize such lesions. CT scan brings enough information to allow the diagnosis but in some cases the MRI can also bring important data that help in the differential diagnosis, detailing better compressive effects on cortical grooves or possible cortical atrophy, found in some dementia.
The cortical vein sign is useful to differentiate cortical atrophy from other diseases. It refers to the presence of superficial cortical veins seen on MRI and CT (particularly with contrast injection) traversing an enlarged subarachnoid space, differentiating it from the similar radiological appearance of a subdural hygroma.
Subdural empyema and isointense hematomas can be more easily diagnosed using contrast.
Clinical data should be extensively explored, looking primarily at neurological symptoms such as headache and focal signs. Fever can be associated with a subdural collection and may suggest empyema in neurologically more affected patients. Seizures are not uncommon. Empyemas may result from a complication of mastoiditis and sinusitis. Insidious alteration of cognitive functions may be present in subdural hematomas, but dementia should also be investigated.1–4 Table 1 summarizes some differential diagnoses of collections or enlargement of subdural space.
|
Appearanceon CT scan |
Previous trauma history |
Contrastenhancement |
Compression of adjacent cerebral sulci |
Midline shift |
Enlargement of sulci and ventricles |
Chronic subdural hematoma |
Hypo/ Isodense |
+ |
+ |
+ |
+/- |
- |
Subdural hygroma |
Hypodense (CSF like) |
+/- |
- |
Rare |
Veryrare |
+ |
Subdural empyema |
Hypo/ Isodense |
- |
++ (surroundingmembrane) |
+ |
+/- |
- |
Pickdisea e (dementia) |
Hypodense (CSF like) |
- |
- |
- |
- |
+* |
Table 1 Some differential diagnosis of chronic subdural hematomas
• Mainly in frontal and temporal lobes
The prevalence of subdural collections in the elderly is high. Treatment is specific to each situation, ranging from conservative management to more invasive surgical procedures. Knowing the radiological characteristics of the lesions, associated with their clinical symptoms, we can make a more accurate diagnosis.
None.
The authors declare that there are no conflicts of interests in this present research.

©2020 Kim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.