MOJ
eISSN: 2574-8130


Research Article Volume 1 Issue 3
1Departamento de Medicina Preventiva, Universidade Federal de São Paulo – UNIFESP/EPM, Brazil
2Departamento de Medicina Preventiva, pela London University, Unifesp-EPM, Brazil
3Department of Odontology, City University of Sao Paulo (UNICID), Brazil
Correspondence: Tania e SP Lacerda, Department of Odontology, City University of Sao Paulo (UNICID), Brazil
Received: October 28, 2016 | Published: April 11, 2017
Citation: Tiberio D, Silva RS, Ramos LR, et al. Factors associated with the presence of dental plaque in an Urban cohort of elderly (Epidoso). MOJ Gerontol Ger. 2017;1(3):68-72. DOI: 10.15406/mojgg.2017.01.00014
Until the 60s, the elderly rarely received preventive care on caries and periodontal diseases. Thus, older individuals do not have dental preventive culture, constituting a group that does not attend the dental office frequently and when they do, the reason is usually pain or a damaged prosthesis. (NIDH_1990)1 Oral health is related to the socioeconomic and cultural conditions of the population. According to Pertesen (2005), oral health is directly related to conditions of food, housing, employment, income, environment, transport, leisure, freedom, access to health services and information. In this sense, the struggle for oral health is fundamentally linked to the improvement of social, political and economic determinants.2
However, the number of individuals fully edentulous has decreased significantly over the years. Data from the US Department of Health show that 46% of individuals between 67 and 74 were edentulous in the 70’s. This rate fell to 29% in the 90’s. Although these data do not reflect the Brazilian reality, it is clear that the preventive care implemented in recent decades allowed more people to preserve their teeth.3
Although the aging process, by itself, causes few triggering effects for impairment and disability in the oral cavity, a significant number of studies show that elderly generally have a poor oral health status.4‒7
The total loss of teeth, edentulism, is still accepted by society as normal and natural with advancing age, and not as a result of the lack of preventive health policies for adults to preserve their teeth in their later years.8
Estimates based on epidemiological data indicate that edentulism decreased 10% each decade lived in the last 30 years, increasing the risk of gingival problems.9 Given that more prevalent periodontal diseases demand dental scaling and polishing, followed by intensification of oral health care by the elderly.10
Results of a survey, published in 2004 by SABE Project (Health, Wellness and aging of the Pan American Health Organization) revealed a situation similar to the study of the 80’s. The Brazilian CPOD index (the sum of decayed, missing and filled teeth due to caries in an individual) aged from 65 to 74 years old reached 27.79 and the great majority derived from edentulism (92%). In addition, only 10% of the elderly have retained at least twenty teeth.11
In 2000, the Convention of the Federation Dentaire International with focus on oral health called for the reduction of tooth loss by 25% in individuals aged 65 years old and over. This goal was not achieved in Brazil, neither was the goal of having 50% of individuals within this age range with at least 20 retained teeth.12
At reaching the goal of retaining at least 20 teeth in the oral cavity, the concerns about dental plaque will be raised, since it is the extrinsic etiologic factor of caries and periodontal disease – and the second biggest cause of dental pathology in the world’s population.13
Dental plaque is a result of microorganisms that remain on surface of teeth and, mainly, in the gingival sulcus where the salivary flow, tongue and food and lip abrasion do not provide effective natural hygiene.14
Although in the last years there have been new effective chemical substances that can reduce or eliminate plaque, like toothpaste with medication and mouthwash, dental plaque removal that leads to prevention and treatment of oral diseases should be done mechanically, mainly by brushing and flossing.14 For efficient results in tooth brushing, it has to be done daily and it requires one’s time, motivation, ability and awareness. This is why some patients, especially elderly, have poor oral hygiene.15‒17
The aim of this study was to detect the factors associated with dental plaque accumulation, measured by the Plaque Index– PI (O’Leary method)18 modified by Duarte (Duarte, 1994)19 in a group of elderly from Epidoso Project.
This work derives from a study of cohort where 600 elderly people were examined during the years 2008-2010, with the goal of evaluating the effects of motivation and efficiency of tooth brushing. The data discussed refer to the baseline information.
A subsample of men and women was created under the criteria: presence of at least 5 teeth that were not indicated for extraction, literate and with no cognitive impairment, good eyesight and hearing, preserved motor skills (data from the Comprehensive Geriatric Assessment - CGA) to assess the distribution of PI.
A single dentist performed all the PI related examinations. Sterilized flat dental mirrors were used and the standards of biosecurity were followed. Previous to gathering, pre-test calibration exercises were conducted in the pilot study with 30 elderly people that were not included in the sample. Duplicate exams were carried on in ten percent of the sample using the Kappa statistic for the calculation of reproducibility, taking the tooth as the unit of analysis for gauging the reliability of diagnosis, following the method previously described by Perez et al in 2001.20
The elderly arrived at Unifesp’s Center for Aging Studies (Centro de Estudos do Envelhecimento - CEE), answered to CGA (Comprehensive Geriatric Assessment) and after evaluation by trained geriatricians were referred to the various sectors, including geriatric dentistry.
After signing a Statement of Informed Consent (IC), the Plaque Index was registered (PI).This controlled clinical trial was approved by the Ethics Committee of Universidade Federal de São Paulo, under protocol number 0678/08.
O’Leary Plaque Index (PI) 18 was evaluated by mouth rinsing with 10ml of EVIFORM for 30 seconds, which revealed the tooth surfaces which had dental plaque. The counting of the stained surfaces were multiplied by 100 and divided by the number of teeth divided by 4 (surfaces of the tooth), thus revealing the percentage of surfaces compromised by plaque, being 10% considered satisfactory by the author.
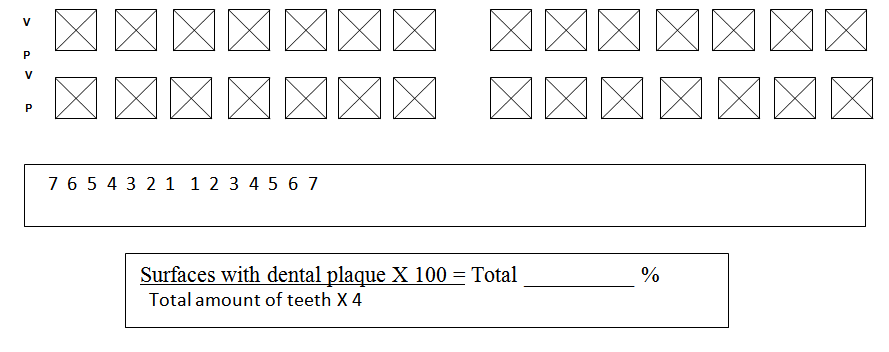
Pigozzo 21 evaluated the main indexes to measure buccal health, getting to the conclusion that O’Leary Index (1972) is the most accurate, since it does not depend on the clinical judgment of the examiner and it is not influenced by subjective factors. It determines the presence or absence of plaque taking into account the faces of the teeth along the gum margins.18
It is an efficient test with fast acquisition, preferred by researchers when using a non populational sample. It has 10% as a satisfactory value; however, this value is very low and almost impossible to be achieved. Therefore, Duarte19 in 1994 referred 48 patients to an oral hygiene motivation program, trying to determine the average dental plaque index at the end of the experiment. O’Leary et al plaque index, Löe&Silness gingival index and Greene-Vermilion oral hygiene index were used for this experiment. The goal was to make a comparative analysis of the three indexes, aiming to determine the highest acceptable O’Leary index to acknowledge good oral hygiene. The O’Leary index presented a statistically positive regression with index teeth, making it possible to conclude that the highest acceptable index was 27.18%.19
This method was chosen due to its precision, efficiency and its speed. Also because it is recommended for non-populational studies considering 27.18% of PI as acceptable.
For univariate analyzes we used the chi-square test to verify the existence of an association between PI - high or not - and other qualitative variables. On the other hand, in case of continuous variables, the F test was used - equivalent to Student's T test, in this case - to check the equality of mean between the two groups of PI.
Logistic regression was used for the multiple analyses. In the complete or initial model all independent variables were addressed. In the next steps non-significant variables were taken out one by one so that only the variables that altogether could represent statistical significance would remain in the final/reduced model. Second-order interactions were tested, but they were not significant. A significance level of 0.05(p<0.05) was used in all analyses.
All elderly presented high PI without significant variations, but presented some differences. It was possible to observe that older women presented lower PI when compared to men who were 70 or older (75% and 87.67% respectively), despite values being beyond the expected as satisfactory (Table 1).
Regarding education level and the fact of living with a partner or not, the differences are very small when evaluating satisfactory PI or not (Table 1).
It was perceived that when income is evaluated a smaller PI percentage (11.11%) is found in the elderly who have satisfactory index and belong to a group that earns less than R$800.00.
The number of teeth in the oral cavity did not show statistical difference, regarding PI with cutoff of 27.18%, as it can be observed in Table 2. However, there is significant difference when the daily frequency of tooth brushing is evaluated in the group of elderly.
Table 3 shows the complete model for logistic regression of variables associated to PI. The final model is presented in Table 4 and it is possible to observe that each tooth brushing doubles the chance of having a satisfactory PI, below 27.18%.
Variables |
Elderly people with PI < 27.18 |
Elderly people with PI > 27.18 |
Total of elderly people |
χ2 Pearson n |
|
Age |
60 to 69 (%) |
13 (21.67) |
47 (78.33) |
60 (100) |
0.48 |
Over 70 years old (%) |
10 (16.67) |
50 (83.33) |
60 (100) |
||
Total (%) |
23 (19.16) |
97 (80.84) |
120 (100) |
||
Gender |
Female (%) |
15 (25) |
45 (75) |
60 (100) |
0.104 |
Male (%) |
8 (13.33) |
52 (87.67) |
60 (100) |
||
Total (%) |
23 (19.17) |
97 (80.83) |
120 (100) |
||
Income |
≥1.5 minimum wage (%) |
21 (20.58) |
81 (79.42) |
102 (100) |
0.34 |
<R$800.00 (%) |
2 (11.11) |
16 (88.89) |
18 (100) |
||
Total (%) |
23 (19.17) |
97 (80.83) |
120 (100) |
||
High school |
Yes (%) |
4 (16.67) |
20 (83.34) |
24 (100) |
0.726 |
No (%) |
19 (19.79) |
77 (80.20) |
96 (100) |
||
Total (%) |
23 (19.17) |
97 (80.83) |
120 (100) |
||
Living with a partner |
Yes (%) |
9 (19.14) |
38 (80.86) |
47 (100) |
0.997 |
No (%) |
14 (19.17) |
59 (80.82) |
73 (100) |
||
Total (%) |
23 (19.17) |
97 (80.84) |
120 (100) |
Table 1 Distribution of the sample according to the PI by age, gender, income, education level, living with a partner.
Variables |
Elderly people with |
Elderly people with |
Total of elderly people |
χ2 |
|
PI < 27.18 |
PI > 27.18 |
Pearson |
|||
Teeth present |
Mean |
15.06 |
15.96 |
14.85 |
0.461 |
(DP) |
(±6.46) |
(±6.99) |
(±6.35) |
||
Daily frequency of tooth brushing |
Mean (DP) |
2.72 (0.80) |
3.13 (0.75) |
2.62(0.79) |
0.007* |
Table 2 Distribution of the sample according to PI relating to the presence of teeth and daily frequency of tooth brushing, with mean and standard deviation.
VARIABLES |
ϐ |
OR |
Significance |
Age |
-0.06 |
0.942 |
0.171 |
Gender |
-0.784 |
0.457 |
0.206 |
Living with a partner |
0.521 |
1.684 |
0.395 |
Frequency of daily tooth brushing |
0.692 |
1.998 |
0.039* |
Education level |
-0,216 |
0,806 |
0,751 |
Income |
0.752 |
2.121 |
0.348 |
Teeth present |
0.1 |
1.01 |
0.432 |
Table 3 Complete model for logistic regression of variables associated to PI.
VARIABLES |
B |
OR |
Significance |
Constant |
-3.461 |
0.031 |
0 |
Number of times tooth brushing was carried on |
0.709 |
2.032 |
0.18 |
Table 4 Reduced Model of logistic regression for PI *
Epidemiological surveys carried out in Brazil and abroad have demonstrated the serious oral health problems that affect people in different countries. The socio-economic and cultural factors of our population have been the cause of numerous problems related to oral health. Dental caries and periodontal disease are closely related to these conditions, presenting high prevalence, therefore being a serious health problem.
Until the 90s Dentistry in Brazil was limited to eliminating pain, that is, its aim was to cure only. Over the years, this kind of thinking gave way to a philosophy of work which did not aim only at pain elimination but also at its cause. It is then Preventive Dentistry for which the principle is based on the prevention of oral diseases through control of its etiology, which in case of dental caries and periodontal disease, it is known as biofilm or plaque. This control can be done by mechanical or chemical agents or through a combination of both.
The mechanical means, which include tooth brushing and flossing can be performed both by the professional or by the patient according to Fischman,22 and they should be the chosen method as they are the safest and the most efficient ones. The myth that aging leads to loss of all teeth added to the lack of initiatives aimed at controlling plaque in the elderly can influence the elderly to neglect plaque control measures.
The PI value found in this study is very worrying as only around 20% of the evaluated individuals presented PI with satisfactory indexes; these values were lower than the ones found in literature23,24 However, it should be emphasized that such studies came to these values through different methodologies from the one of the present study. The current study found an average of 15 teeth present, similar to the 2009 study,17 but with slight higher values than in literature.25,26
Regarding dental plaque, 80.82% of elderly presented Plaque Indexes higher than the maximum considered satisfactory (its value is 27.18%), which can harm the respiratory system.27 In a study with young people, there was an association of unsatisfactory PI to ow socio-economic situation28 which was not concluded in our study, maybe for having a sample constituted of elderly.
Queiroz29 states that although age is not synonymous with disease, old age increases the risk of the functional capacity impairment, with the consequent loss of autonomy and independence. Perhaps this information justifies why this index is more prevalent in elderly aged older than 70.
Mini-Mental State Examination (MMSE)30 is a test in which results below 25 lead to suspect cognitive impairment. Studies show association of functional disability with cognitive deficit,31 creating the expectation of finding unsatisfactory PI values for the elderly with MMSE below 25. This result was not found as elderly with MMSE below 25 were not included in the sample.
The results of the study point to the fact that brushing more than twice a day is a protective factor for the deposit of plaque, similar to the studies in 200232in which 62 dentistry students brushed their teeth in the usual way for three consecutive times, the results indicated that the plaque reduction was significant after each of the three brushings, suggesting that with only two the level of dental plaque has reached the expected results for effective brushing. One has to reflect that this study evaluated young people and consecutive brushings, in contrast to our study, but it seems that older people do not have the same frequency of brushing as the young.
The comparison to other works related to satisfactory values of PI should be cautious, since the PI in the literature is assessed in different ways and with different satisfactory values. More studies evaluating the plaque index in the elderly are required.
High prevalence of unsatisfactory PI in the studied sample points to the need of developing interventions that aim at motivating oral hygiene among the elderly. Considering that as the number of daily tooth brushing decreases in 18% at each increment unit – varying from 1 to 5, a first step could be stimulating more frequency in daily tooth brushing.
None.
Author declares there is no conflict of interest in publishing the article.

©2017 Tiberio, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.