MOJ
eISSN: 2374-6912


Conceptual Paper Volume 3 Issue 4
Department of Molecular Medicine and Biology, Jaslok Hospital & Research Centre, India
Correspondence: Pravin D Potdar, Department of Molecular Medicine & Biology, Jaslok Hospital & Research Centre, Maharashtra, India, Tel 912266573445; 919820833530, Fax 912223520508
Received: July 22, 2016 | Published: August 4, 2016
Citation: Potdar P, Chaudhary S. Cancer immunotherapy: new technology to target cancer cells. MOJ Cell Sci Rep. 2016;3(4):111-112. DOI: 10.15406/mojcsr.2016.03.00065
Immunotherapy is a highly personalized cancer therapy which involves infusion of immune cells having anticancer activity into cancer-bearing host cells. The initial conception of this therapy stems from the work of Dr. Coley back in the 1890s who theorized that the infection of cancer patient with streptococcal infection leads to reduction in tumor size.1 This observed antitumor activity was thought to occur as the tumor cells get caught in the crossfire of attack between the pathogen and the immune system. This notion that immune cells possess the antitumor activity is also supported by the fact that immunosuppressed patient are three times more prone to sarcomas than the general population.2 The fact that immune cells can be manipulated to direct against cancer has revolutionized the field of cancer therapy. Treating cancer with high dose of interleukin (IL)-2 has been the subject of investigation in clinical trials for many years3 and showed promising results both in metastatic melanoma and renal cell carcinoma.4 However, according to the recent studies conducted on metastatic patient of different etiology, patient has shown the unlikely relapse and toxicity after IL-2 treatment.4,5 Nevertheless, IL-2 still serves as one of the important adjunct in the therapy of various cancers as shown in Figure 1. The programmed cell death receptor (PD-1) is present on T cells while its ligand PD-L1 is expressed by variety of tumor cells to dampen the immune response. This evasion of tumor cells from immunosurveillance is reported in 19% to 92% of tumor cells and often associated with poor prognosis.6 Targeting the immune checkpoint PD-1 using inhibitors therefore represents a novel therapy to prevent the immune dampening response by advanced cancers as shown in Figure 1. In phase I clinical trial study conducted on metastatic melanoma patient, the anti-PD1-1 pembrolizumab has demonstrated significant long lasting activity and increase in the survival rate.7 Another FDA approved drug called atezolizumab works by inhibiting the PD-1/PD-L1 interaction and has shown to drastically reduce the tumor size in patient suffering from advanced bladder cancer.8 Another super family of immune checkpoint called CTLA-4, a protein expressed on the surface of killer T cells and blocks the ability of T cells to kill cancers as shown in Figure 1. In 2011 FDA approved the drug called Ipilimumab (CTLA-4 inhibitor) for the treatment of metastatic melanoma and the results were very promising.9
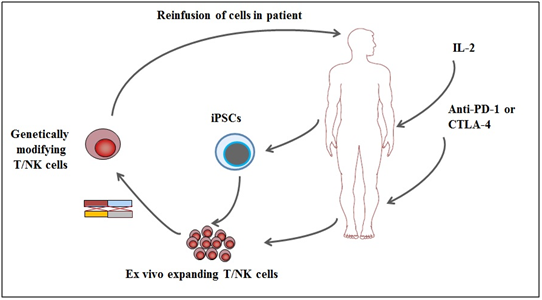
Figure 1Schematic representation of cancer immunotherapies used in current trial. Administration of IL-2, anti-PD-1 and anti-CTLA-4 has been the active area of research in cancer therapy. Besides, T/NK-cells based targeted therapy has also been the main area of investigation for cancer therapy. Induced pluripotent stem cells (iPSCs) can also provide the source of generating T/NK-cells for cancer immunotherapy.
Chimeric antigen receptor (CAR) represents a new wave of targeted cancer therapy and has gained a lot of attention in medical community. The inception of CARs was pioneered by Gross and colleagues.10 CARs can provide recognition of cancer cells antigens via the non-MHC-restricted pathway and can be expressed into T cells using recombinant viral vectors. These genetically modified T cells on further adoptive transfer in host leads to the launching of strong immune attack against cancer.11 In one of the clinical trial study, CD19-directed CAR T cells in patient with high-risk chronic lymphocytic leukemia demonstrated highly significant anti-tumor response and 2 patients with long term complete remission (CR).12 Similar results were obtained with patients suffering from acute lymphocytic leukemia with the average CR of 70% to 90%.13 In some of the patient that has underwent CAR T cell therapy, leukemia relapsed and some researcher have hypothesized that targeting the leukemia stem cells population expressing CD33/CD123/CD44 can reduce the incidence of relapse.14 If this therapy will become more successful, our future generation will definitely think how barbaric chemo/radiotherapy was to treat cancer.
Natural killer cells have also emerged as one of the key player within the context of haploidentical SCT having strong anti-tumor potential. Many researchers have already harness the potential of NK cells by developing immuno ligands that target NKG2D via its cognate ligand (ULBP2) and bind to the target cells via an antibody derived single chain, which is specific for a tumour-associated antigen.15,16 These immuno ligands have demonstrated anti-tumour activity both in vitro and in vivo. In phase I clinical trial study conducted on advanced digestive cancer patient, NK cells infusion was well tolerated by all patients with no adverse events.17 However, there was no clinical response was reported but nevertheless, there is still an area of improvement within the context of genetic modification for developing NK-cells based effective cancer immunotherapies as shown in Figure 1. Although the field of immunotherapy is improving and currently not been able to help all cancer patients, it is still considered as one of the holy grail of 21st century to fight against cancer. Scientists have a huge hope on the success of immunotherapy because of the improvement in gene expression profiling using the next generation sequencing technology, sophistication in the design of clinical trials and increased in the awareness of clinical trials. The advent of Induced pluripotent stem cells (iPSCs) will provide the renewable source for T/NK cells which will broaden the immunotherapeutic applications as shown in Figure 1. The field of immunotherapy will definitely accelerate the field of scientific research in finding therapy for cancer which will be less toxic and more effective to cure most of cancers even at advanced stage.
None.
The author declares no conflict of interest.

©2016 Potdar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.