MOJ
eISSN: 2381-179X


Case Report Volume 5 Issue 1
1Central Military Hospital, National Defense Secretary, Mexico
2General Surgery Department, General Zone Hospital, Mexico
3General Surgery Department, Military School for Sanity Graduated, Mexico
4General Surgery Department, General Regional Hospital, Mexico
5Endoscopy Department, GEA Gonzalez Hospital, Mexico
6General Surgery Department, Ecatepec General Hospital, Mexico
7National Medical Center Antonio Fraga Mouret La Raza, Mexico
Correspondence: Luis Angel Medina Andrade, General Surgery Department, General Regional Hospital #30, IMSS, México, Tel 52 9981114201
Received: October 14, 2016 | Published: October 31, 2016
Citation: Lomelí MAC, Andrade LAM, Chavarría EJ, et al. Synchronus ameboma in vater ampulla and colon, first case reported in literature. MOJ Clin Med Case Rep. 2016;5(1):163-165. DOI: 10.15406/mojcr.2016.05.00117
Aim: An inflammatory and proliferative response to amibiasis infection is known as ameboma, a pseudotumoral lesion; the ascendant colon is the most frequent location.
Case report: A male of 65years-old referring diarrhea and epigastric pain comes to emergency room. At physical exam with tachycardia, tachypnea, abdominal pain located in epigastrium, right iliac fossae and rebound sign. Laboratories report leukocytosis, neutrophilia and eosinophilia. Abdominal ultrasound reports a paracecal abscess, probably secondary to acute appendicitis. Laparotomy was performed finding an infiltrating tumoral lesion in ascendant colon, with perforation and abscess extended to the duodenum, and another tumoral lesion in Vater ampulla. A right extended hemicolectomy was performed with oncological approach and, after 48hours in the Intensive Care Unit, Whipple procedure was completed. Patient developed amebic colitis with sigmoidal perforation and a subtotal colectomy was completed. After medical treatment, patient presents multiple organic failures and died at 9thday. Histopathological exam reports Vater ampulla ameboma with extension to pancreas, right colon ameboma, and ulcerative amibiasis in colon.
Conclusion: At our knowledge this is the first reported case of Vater ampulla ameboma in literature. The diagnosis of this lesions are difficult inclusive after CT scan, but it can be treated medically. It must be considered in the differential diagnosis of colonic tumors and, in case of suspect in an acute abdomen scenario, the source must be treated and resection avoided if possible.
Keywords: ameboma, vater ampulla tumor, colonic tumor
A granulomatous and proliferative lession, usually affecting ascendent colon, secondary to invasive amibiasis infection is known as ameboma. Globally it represents about 1.5 to 8.4% of all invasive amibiasis and usually appears in patients without treatment or with unefective treatments manyyears after a dysentery.1 It usually presents as an unique lession, and only in a few cases with a synchronous lession. In fact, there is no previous reports about an ameboma in Vater ampulla.
A 65years-old man without pathological background comes to emergency room by abdominal pain and diarrhea the last 20days. He comes from a rural population, with zoonosis and poor dietary and hygienic habits. An abdominal epigastric pain of 3months of evolution and diarrhea the last 20days was referred, with pain increasing the last 72hours. At physical exam he was dehydrated, with facies of pain, tachycardia with 120 beats per minute, tachypnea of 27 breaths per minute, globose abdomen, without peristalsis, with palpable mass in the right iliac fossa and acute abdomen signs. Laboratories report leucocytes 21,000 neutrophilia and eosinophilia, Creatinine 1.9mg/dL, bilirubin and hepatic function test without alterations. Arterial blood gas analysis shows metabolic acidosis and respiratory alkalosis pH 7.22, HCO3 13mEq/L, PaCO2 25 mmHg, BEecf -15mmol/L, SO2 89%. An abscess in right iliac fossa probably secondary to appendicitis was suggested by abdominal ultrasound report. By the previous mentioned reasons an exploratory laparotomy was performed founding a tumoral lesion in right colon (Figure 1), with wall infiltration and presence of necrotic patches with drilling contained, affecting retroperitoneum and duodenum in their first and second portion, both of them with necrotic lesions too and another tumoral mass in Vater ampulla (Figure 2), mesenteric adenopathy of 1cm.
The other sections of colon showed hyperemia in the serosa, without ischemic changes or palpable tumors. Consequently, an extended right hemicolectomy with oncological approach, terminal ileostomy, duodenorrhaphy and pyloric exclusion was completed in the first surgery, with ICU management for the next 48 hours to improve general conditions and performing Whipple procedure after that, without evidence of duodenal drilling from first surgery. Back in the ICU "patients" present septic shock in the second day, with feculent drainage drains and, in the consequent laparotomy, a subtotal colectomy was completed secondary to perforated colitis in sigmoid colon.
The histopathology report of the first surgery refers a right colon ameboma with infiltration to duodenum and Vater ampulla (Figures 1) (Figure 2), and in consequence treatment with Albendazol was administered with poor response, developing multiple organic failure and death at 9thday. Ameboma in Vater ampulla, pancreas infiltration with Histolytic Entamoeba (Figure 3) and ulcerative amibiasis in left colon was reported in the definitive histopathology exam.
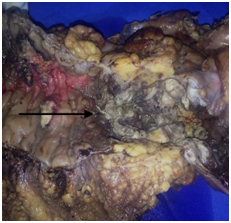
Figure 1 Ascendent colon with an indurated and gray lession of 4x5cm (Black arrow), and an intense periferic inflammatory reaction.
Parasitic diseases constitute one of the most important morbidity causes worldwide, reflecting the health deficiencies characteristic of poor areas, with overcrowding and inadequate management of water and excreta. Amibiasis represent an important public health problem, especially in Mexico as an endemic zone. This is the third most important parasitic disease in the world.2,3 The prevalence is about 10%, reaching 50-80% in developing countries and tropical zones. The lethality associated with complications is estimated between 0.1 and 0.25%. Invasive amibiasis is focused in a few countries including México, south of America, south of Asia, east and west Africa.2,3 Although diarrheic diseases have presented a decrease in Mexico, and the incidence of this pathology have diminished in the last 20years, it stills between the first twenty causes of morbidity, actually in the sixth place.2 According to geographic location in the country, south and southeast states have the highest incidence in México. Amibiasis affects colon, but liver is the most frequently extra-intestinal organ affected. Infections include a wide variety of presentations like asymptomatic carrier state, colitis, and abscess formation or perforation. It has been demonstrated that the Histolytic Entamoeba trofozoitos travels from colon to liver through the portal venous system, and are responsible for the invasive disease. The intestinal invasion is characterized by “shirt button” ulcers in the mucous surface.4,5 Rarely, patients with a long disease evolution develop exophytic, inflammatory and scared lesions known as “amebomas” or granulomas, with an incidence of 1.5 to 8.4%.5–7 Necrotic tissue during amebian colitis is replaced by an extensive inflammatory reaction and pseudotumoral lesion, probably secondary to a synchronous bacterial infection. Amebomas could be unique or multiple, usually presented in males between 20 to 60years. The most frequent location is in cecum, cecal appendix and rectum-sigmoidal union in this order. Other reported sites include hepatic flexure, transverse colon and splenic flexure.8 In our review of literature, we have not identified any previous report of pancreatic or Vater ampulla ameboma. In the present case it was not suspected by imaging studies and because presentation was without jaundice although lesion infiltrate Vater ampulla, making more difficult to suspect, with surgical remotion by Whipple procedure but without a consensus on management by the rarity of the case. Differential diagnosis includes ileocecal tumor like tuberculoma, lymphoma, adenocarcinoma, Crohn disease, atypical fungal disease, arterial-venous malformations and diverticulitis.9,10 Histologically it could be observed flask look like ulcers extending to submucosa layer, associated with a necrotic and inflammatory extensive exudate. Often the adjacent mucous layer is normal and there is not granulomas.10
Preoperative diagnosis seems to be very difficult and generally missed barium enema revealed multiple changes in a patient with amebian colitis presence of stenosis or a tumor look like image can confuse us for the final report.11 Ultrasound and contrasted computed tomography could detect a colon lesion indistinguishable from cancer and cannot allow us to suspect an invasive amibiasis, and for this purpose a colonoscopy would be required, preferably with indocianina green light and direct image, plus the histopathological exam.12 In an emergency scenario with acute abdomen presentation, like in this case, ameboma diagnosis suspicion is not essential and according to surgical findings it would be resolved, with posterior histopathologic analysis if lesion was identified and resected.13 In México Rodea and cols analyzed 25,840 urgent abdominal surgeries from 1970 to 2007, with 129 cases with colonic complications secondary to amibiasis. From the previous, only six ameboma cases were reported, all of them in right colon, presented with acute abdomen or intestinal obstruction signs, only diagnosed after surgery by histopathological exam.14 In the presented case, by the presence of a probably malignant right colon tumor complicated with perforation, an extended hemicolectomy with oncologic criteria was justified. The amebomas must be included in the differential diagnosis of colonic unsuspected tumors, furthermore it does not require resection, justifying no resection in case of incidental finding until complementary studies, unless complication like massive bleeding, obstruction or perforation.15
Frequently amebomas could be treated medically with good outcomes. However, in complicated cases like colonic perforation poor response could be presented and surgery must be the only option.16 Recommended medical treatment include 5 to 10days of metronidazole orally (750mg every 8hours), plus an intraluminal anti-amibian drug like Furoato of Diloxanida or Paromicina.17 After four months of treatment a colonoscopy must be performed to visualize improvements, and total remission at eight months.18,19
As a consequence of invasive amibiasis the ameboma would appear, with a very low incidence, but a little more in developing countries where the incidence of Entamoeba histolytica infection is high, especially in the asymptomatic carrier state. By the previous mentioned facts, is a disease with high risk of systemic complications like liver abscess and, in rare cases, Ameboma. Actually this is the first reported case of Ameboma in Vater ampulla and pancreas at our knowledge, a very unusual case mimicking an oncologic entity that involve a complex surgical treatment, even more in the case of intestinal perforation. For this experience we recommend to realize a serologic study and colonoscopy with biopsy in stable patients from endemic areas of amibiasis with chronic abdominal pain and colon tumor, without acute abdomen signs, to begin with antibiotic treatment and avoid the high morbidity and mortality associated with an unnecessary surgical resection.
None.
The author declares no conflict of interest.

©2016 Lomelí, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.