MOJ
eISSN: 2381-179X


Case Report Volume 13 Issue 4
Hospital Professor Doutor Fernando Fonseca, EPE, Portugal
Correspondence: Rita Vale Martins, Hospital Professor Doutor Fernando Fonseca, EPE, Amadora, Portugal
Received: November 09, 2023 | Published: November 29, 2023
Citation: Martins RV, Almeida F, Matias R, et al. Peptic ulcer penetrating a hepatic cyst: an unusual case and a literature review. MOJ Clin Med Case Rep. 2023;13(4):80-82. DOI: 10.15406/mojcr.2023.13.00444
Introduction: The 30-day mortality associated with complicated PUD is estimated at 8.6% for hemorrhage and 23.5% in case of perforation. Occasionally ulcer penetration to adjacent viscera without free perforation occurs, the most frequent being to the pancreas, lesser omentum, biliary tract, and greater omentum.
Case presentation: A 72-year-old male with a previous diagnosis of peptic ulcer disease presented in the ER due to hematochezia and lightheadedness. The blood work revealed new onset anemia and elevated inflammatory parameters. Upper gastrointestinal endoscopy and CT scan suggested a peptic ulcer complicated by hepatic cyst penetration and fistula. Proton pump inhibitors and empiric broad-spectrum antibiotic were initiated. On the 10th day post-presentation, the patient underwent a subtotal gastrectomy with Billroth II reconstruction and hepatic cyst fenestration and drainage.
Discussion/Conclusion: Nowadays, ulcer penetration is a rare complication of peptic ulcer disease. Therapeutic options include conservative management with PPI, antibiotics, and percutaneous/endoscopic drainage or surgical therapy, depending on the extension/location of the ulcer and abscess and the patient's characteristics.
Keywords: peptic ulcer, hepatic cyst, gastric ulcer
Peptic Ulcer Disease (PUD) consists of gastric or duodenal mucosal disruption with exposure of the submucosa to gastric acid.1 PUD-associated mortality has declined since the 19th century, primarily due to improvements in basic sanitation (with reduced infection rates by Helicobacter pylori-HP), HP infection treatment with antibiotics, and anti-secretory drugs.1 Despite PUD's relatively low incidence in developed countries (0.1-0.3% per year), it has a considerable burden when complicated (which occurs in 20% of the patients).1 The most frequent complications are bleeding (with an incidence of 19.4 to 57.0 cases per 100,000 individuals in Europe) and perforation (with an incidence of 3.77 to 14 cases per 100,000 individuals in Europe),2 as acute complications, and gastric outlet syndrome,1 as chronic. The 30-day mortality associated with complicated PUD is estimated at 8.6% for hemorrhage and 23.5% in case of perforation.2 Occasionally ulcer penetration to adjacent viscera without free perforation occurs, the most frequent being to the pancreas, lesser omentum, biliary tract, and greater omentum. The authors present an unusual case of a patient with a pyloric ulcer penetrating a hepatic cyst and review the published literature.
A 72-year-old male with a previous diagnosis of peptic ulcer disease but not taking medication presented in the
E.R. due to hematochezia (first episode) and lightheadedness. The patient also referred asthenia and anorexia in the previous week. He denied abdominal pain, vomiting, as well as other symptoms. At observation, the patient was normotensive, normocardic, apyretic, and had pale skin. The abdominal exam was normal, and active hemorrhage was not detected on rectal examination. The blood work revealed a new onset microcytic anemia (78 MCV) with 5.8 g/dL of hemoglobin (8 months previously, the patient had 15g/dL), elevated inflammatory parameters (CRP 16mg/dL and 15,000 leucocytes), and normal kidney and liver function. A nasogastric tube was placed without hemorrhage evidence, proton-bomb inhibitors were administrated (pantoprazole perfusion), and transfusion of 2 red blood cell concentrates as well as supportive care was initiated.
Upper gastrointestinal endoscopy revealed a grade B peptic esophagitis, abundant biliary content in the gastric corpus and fundus, and an extensive ulcer involving the pylorus at the level of the gastric incisura. Endoscopic progression beyond the pylorus was not possible due to patient intolerance. Ulcer biopsies were collected and compatible with inflammatory infiltration without neoplastic cells.
Due to the findings, a C.T. scan was requested (shown in Figure 1 and Figure 2). Several biliary hepatic cysts with varying dimensions were noted, but no hepatic solid lesions were detected. The liver segments IV and V presented with an 11.5 x 9.7 cm non-pure liquid collection, with gastric communication, evidenced by multiple air bubbles and oral contrast. Periceliac and perigastric ganglia were noted. No relevant findings were detected in the thoracic study or the remaining abdomen and pelvis.
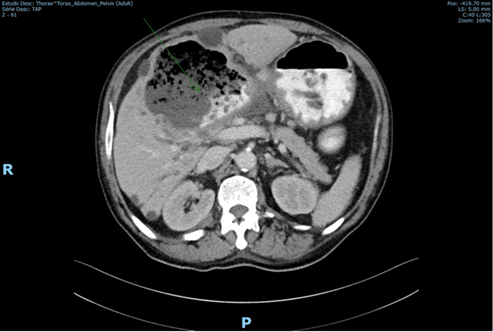
Figure 1 CT scan with oral contrast administration showing a hepatic collection containing air and oral contrast.
The patient was maintained under PPIs, and an empiric broad-spectrum antibiotic (Meropenem) was initiated, remaining stable. Surgery was scheduled on the 10th-day post-presentation after a multidisciplinary case discussion. Intra-operatively the hepatic collection described in the C.T. scan matched a hepatic cyst penetrated by a peptic ulcer. The ulcer surface was 2 cm, involving the antrum and proximal duodenum. No macroscopic signs of neoplasia were found. Partial gastrectomy with Billroth II reconstruction and fenestration and drainage of the hepatic cyst were performed.
The post-operative was complicated by a minor biliary leak, repaired after reintervention, where the obliteration of the cyst surface was performed. The pathological analysis revealed chronic and atrophic gastritis with intestinal metaplasia in the gastric antrum without evidence of dysplastic neoplastic cells. The ganglia were reactive. H.P. was not detected. The hepatic piece did not present with neoplastic cells either.
We present a rare case of PUD complicated hepatic cyst penetration. Ulcer penetration occurs in order of decreasing frequency into the pancreas (52.6%), lesser omentum, biliary tract (18.4%), greater omentum (10.7%), liver (6.2%), mesocolon, colon (1.5%) and vascular structures.2-4 Depending on the affected viscera, the penetration of peptic ulcers can be complicated by fistula, abscess, or hemorrhage.4
In this case, the ulcer penetrated a liver cystic lesion creating a well-tolerated and slowly evolving cysto-gastric fistula and hepatic cyst abscess. Simple hepatic cysts affect 1 to 2.5% of the general population and rarely complicate.5 Apart from the PUD, the constant mechanical friction between the cyst and the visceral wall, with the latter's erosion, contributes to fistula formation.6
Contrary to perforation, characterized by sudden and intense symptoms, ulcer penetration is usually more indolent and characterized by subtle symptom changes.2 The main symptom in this patient was gastrointestinal bleeding, which according to Somi M et al. (2007), is a common inaugural symptom in ulcer penetration to hepatic parenchyma. The clinical picture is also indolent, with unspecific complaints of asthenia and/or epigastric dull pain, usually in patients with previous PUD history (as in our case).3
The diagnosis can be obtained by: upper gastrointestinal endoscopy with confirmation of hepatic parenchyma on ulcer biopsies; abdominal ultrasound, revealing the presence of a hepatic abscess with the passage of air bubbles and liquid content between the stomach and the cavity; or CT-scan.4
Endoscopic exams or CT scans cannot exclude malignancy and should indeed be suspected. It can present findings similar to PUD (especially if the biopsy misses tumoral cells) and is a more frequent cause of penetrated gastric ulcers. Due to the extensive inflammatory process, ulcer dimensions, the impossibility of excluding malignancy and relapse risk, percutaneous abscess drainage, and primary repair of the antrum defect were not considered suitable options, and a partial gastrectomy with intra-operative abscess drainage was preferred.
In some cases, with reduced ulcer and liver abscess/cyst size, conservative management (with H2 receptor antagonists and PPIs, percutaneous or endoscopic drainage, parenteral nutrition, and antibiotics) is possible. It could be considered if the patient has important comorbidities or the risk of free perforation is low.3,4,7,8 In this case, Helicobacter pylori infection was not detected, either in endoscopic biopsies or in the subtotal gastrectomy piece evaluation, so no eradication was necessary.
Table 1 summarizes peptic ulcers complicated by hepatic parenchyma and cyst penetration - most cases presented with gastrointestinal bleeding or epigastric pain. When a surgical treatment was carried the most frequent was a partial gastrectomy with a Billroth II reconstruction, complemented with PPI (proton-pump- inhibitors) or H2A.
|
Author |
Age (years)/ Gender |
Presentation |
Location |
Treatment |
Outcome |
|
*Kayacetin et al.7 |
61/ M |
GI bleeding |
Anterior wall of gastric antrum |
PPI |
Survival |
|
*Park et al.10 |
52/M |
GI bleeding |
Lesser curve of Antrum |
H2A |
Survival |
|
*Venkatesh et al.9 |
81/F |
Epigastric pain |
Lesser curve of Stomach |
PII + percutaneous drainage |
Survival |
|
*Goldman et al.11 |
65/M |
Nausea, anemia |
Lesser curve of Stomach |
BII |
Survival |
|
*Brullet et al.12 |
89/F |
GI bleeding |
Anterior wall of gastric antrum |
Surgical NE |
Death |
|
*Novacek et al.13 |
33/F |
GI bleeding |
Posterior wall of duodenal bulb |
PPI + Feinney-type duodenoplasty |
Survival |
|
*Guerrieri et al.14 |
53/M |
GI bleeding |
Lesser curve of Antrum |
Antiacids + BII |
- |
|
*Castellano et al.15 |
77/M |
GI bleeding |
Posterior wall of duodenal bulb |
BII |
Survival |
|
*Castellano et al.15 |
70/M |
GI bleeding |
Posterior wall of Antrum |
BII |
Not related death |
|
*Matsuoka et al.16 |
53/M |
GI bleeding |
Lesser curve of Corpus |
H2A + BI |
Survival |
|
*Sommi et al.3 |
60/M |
Anemia, weight loss |
Anterior wall of duodenal bulb |
Medical NE + Surgical NE |
Survival |
|
*Oka et al.4 |
75/M |
Epigastric pain, anemia |
Proximal duodenum |
H2A |
Survival |
|
*Mall et al.17 |
57/F |
GI bleeding |
Posterior wall of duodenum bulb |
PPI |
Survival |
|
*Akyildiz et al.18 |
21/F |
GI bleeding |
Anterior wall of duodenal bulb |
PPI |
Not related death |
|
*Kypraios et al.19 |
55/F |
Epigastric pain |
Anterior wall of gastric body |
Surgery NE |
Survival |
|
*Lesquereux-Martínez et al.20 |
66/M |
GI bleeding |
Anterior wall of gastric antrum |
Medical NE |
Survival |
|
#Jung et al.6 |
70/F |
GI bleeding and pain |
Anterior wall of the duodenal bulb |
PII+endoscopic drainage |
Survival |
|
#Ono et al.5 |
88/F |
Epigastric pain |
Anterior wall of the duodenal bulb |
PII+endoscopic drainage |
Survival |
Table 1 Case reports of of peptic ulcer complicated with hepatic parenchyma and cyst penetration
M, male; F, female; GI, gastrointestinal; NE, not specified; PPI, proton-pump-inhibitors; H2A, histaminergic receptors antagonists; BI, Billroth I; BII, Billroth II (with subtotal gastrectomy); *, hepatic parenchyma abscess; #, hepatic cyst abscess
(histaminergic receptor antagonists), the treatment options are similar whether the penetration is into the parenchyma or to the cyst. Amongst the referred cases, three deaths were recorded, one due to meningoencephalitis, one due to pulmonary embolism, and one related to the PUD complication. Due to the inability to access the information or the fact that malignant pathology was involved, some cases referred to in previous papers were not considered in this analysis.
Herein it is described the case of a patient who exhibited perforation of a pyloric ulcer into a hepatic cyst complicated by the abscess. Nowadays, ulcer penetration is a rare complication of peptic ulcer disease. It is most frequent in the pancreas (52.6%), lesser omentum, biliary tract (18.4%), greater omentum (10.7%), liver (6.2%), mesocolon, colon (1.5%), and vascular structures. The diagnosis can be obtained by imaging (ultrasound or CT scan) or upper endoscopy and is suspected in the presence of previous hepatic cysts. Therapeutic options include conservative management with PPI, antibiotics, and percutaneous/endoscopic drainage or surgical therapy, depending on the extension/location of the ulcer and abscess and the patient's characteristics. These options are similar for hepatic parenchyma and cyst abscess. Testing for H. P. is critical for optimal therapy.
Written informed consent was obtained at the time of surgery from participants for publication of the details of their medical case and any accompanying images.
R.V.M and F.A. conceived of the presented idea., R.M. reviewed the literature and the clinical case, F.A., R.M. and P.M. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
The data that support the findings of this study are openly available through the References.
None.
The authors have no conflicts of interest to declare.

©2023 Martins, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.