MOJ
eISSN: 2381-179X


Case Report Volume 13 Issue 4
1St. George’s University School of Medicine, United States
2Psychiatry Unit, Elmhurst Hospital United States
3Research Center of the Hospital Center of the University of Montreal, Canada
4Public Health School of the University of Montreal, Canada
Correspondence: Khayreddine Bouabida, Research Center of the Hospital Center of the University of Montreal, Montreal, QC H2X 0A9, Canada
Received: December 10, 2023 | Published: December 21, 2023
Citation: Jagram N, Dar K, Bouabida K. Neurocysticercosis infection presenting with psychotic features: case report. MOJ Med Clin Case Rep. 2023;13(4):93-96. DOI: 10.15406/mojcr.2023.13.00447
Neurocysticercosis is a rare parasitic central nervous system infection caused by ingesting Taenia Solium eggs. Diagnosing neurocysticercosis can be challenging, as the symptoms can mimic other neurological and psychiatric conditions. In this paper, we present a rare case of a 25-year-old male with Neurocysticercosis, and we highlight certain clinical aspects of the patient's presentation. We discuss the importance of a comprehensive medical evaluation and a multidisciplinary approach using the guidelines of the Neurocysticercosis diagnostic framework when assessing patients with Neurocysticercosis who present with psychiatric symptoms. Through this paper, we raise awareness of Neurocysticercosis and encourage clinicians to collaborate closely and to promote research in this context.
Keywords: neurocysticercosis, infection, psychosis, emergency, neurocysticercosis diagnostic guidelines
Neurocysticercosis is a parasitic infection of the central nervous system caused by ingesting Taenia Solium eggs.1-6 The Taenia Solium is frequently acquired from ingesting the larval stage tapeworm, frequently found from pork in endemic countries where access to sanitation might be challenging, such as in Latin America, India, Africa, and China1-6 (See figure 1).7 Another important factor influencing higher infection rates is improper hygiene practices in certain slaughterhouse services, thus, consuming undercooked pork in these endemic countries increases the risk of transmission to humans.4 The parasitic infection itself has many effects on the CNS, with the most common presentation being epilepsy. Albeit epilepsy is the most common sign of infection with this parasite, there are a spectrum of manifestations including neuropsychiatric symptoms. Some other common symptoms include focal neurological deficits, headache due to increased intracranial pressure, and cognitive decline.5,6 Importantly, it should be noted that depending where the lesions are in the brain will determine the signs and symptoms of the disease. Due to neurologic symptoms being the most common manifestation, Neurocysticercosis is often considered in patients who have a supporting history, but it has not been commonly considered in psychiatric conditions. A variety of mental health problems may be induced by this infection such as delirium, anxiety, depression, psychotic episodes, personality changes, dementia, and cognitive decline. It has been stated that before the emergence of modern neuroimaging patients were brought to psychiatric hospitals and the diagnosis of neurocysticercosis was not reached in these patients until they developed the common neurological symptoms such as seizures.6 Thus, psychiatric manifestations may be the initial presentation in these patients in which their cases may likely be underreported and underdiagnosed.1-6
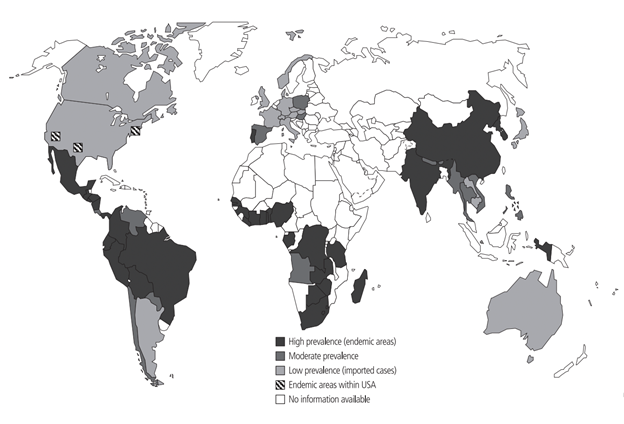
Figure 1 Map showing areas where neurocysticercosis is endemic. (Scientific Figure from ResearchGate).7
Diagnosing neurocysticercosis can be challenging, as the symptoms can mimic other neurological conditions. Imaging techniques such as MRI or CT scans are essential to visualize the cysts in the brain or spinal cord. Serological tests may also be used to detect antibodies against the parasite. Therefore, the diagnosis shouldn't rely on psychiatric features alone and imaging investigations should be combined with the psychiatric assessment with diligence, especially when dealing with psychiatric features in patients from endemic areas of neurocysticercosis.8 Treatment for neurocysticercosis typically involves a combination of medication and, in some cases, surgical intervention.1,5,6,8 Anthelmintic drugs, such as albendazole or praziquantel, are prescribed to neutralize the cysticerci. Steroids may also be given to reduce inflammation caused by the dying parasites.4-6,8 In severe cases where resistance to pharmacological treatment is present and or cysts are large, causing significant neurological problems, surgical removal of cysts may be necessary.4-6,8 In terms of preventing neurocysticercosis, this involves improving sanitation and hygiene, ensuring proper cooking practices of pork to eliminate any potential cysts, and avoiding ingesting contaminated food or water. It is crucial to seek medical attention promptly if there are any signs or symptoms suggestive of neurocysticercosis, especially in areas where the disease is prevalent.2,4-6,8
A 25-year-old male immigrating from Ecuador was brought into the emergency department by EMS activated by his father for aggression at home and changes in his behavior. The patient had arrived from Ecuador in January 2023 and the family stated that since then he had stopped showering, stopped eating regular meals, and has lost about 30 pounds. The patient had no known past medical history, no known past psychiatric history, or inpatient psychiatric admissions. However, he did have a history of mandibular fracture repair in 2022 after suffering a TBI during an assault in Ecuador. During his hospitalization, the patient was noted to have marked tangentiality in his speech and was evasive to interview questions, often providing vague answers. It was noted that the patient was disheveled, had poor hygiene, and refused to shower. At the time it was seen that he was inappropriately laughing and smiling. Later, during his stay in the inpatient facility, he endorsed that he had been planning to move back to Ecuador. However, on the day of admission, he saw multiple black cars outside of his home and felt that people were waiting for him to come out. During his stay in the inpatient unit, it was observed that he was guarded and suspicious, often facing the window during mealtime, not engaging with peers, and continued to exhibit poor hygiene. He denied any active mood symptoms concerning depression or mania. Throughout his stay, he appeared to be internally preoccupied. As stated previously his past medical and psychiatric history were negligible, but he did have a history of using cannabis. Overall, throughout the patient's 30-day stay in inpatient, his vitals were stable. The patient's psychosis was treated with risperidone, and towards his discharge he was switched to the long-acting injectable antipsychotic, paliperidone. As his stay in the hospital progressed, the patient's psychotic symptoms, such as paranoia and delusions, mildly improved, but his baseline continued to be guarded and avoidant of other patients until his discharge day. Lab workup included CBC, CMP, and toxicology screen. CBC showed a slightly low range but insignificant values of hemoglobin, hematocrit, and white blood cell count. The CMP showed no electrolyte abnormalities, revealing an elevated ALT, AST, and ALP. The urine toxicology screening revealed he was negative for opioids, cocaine, amphetamines, PCP, THC, barbiturates, and benzodiazepines. Non-contrast head CT imaging was obtained, and this demonstrated punctate dystrophic calcifications in the right ambient cistern and the third ventricle (See Figure 2 and Figure 3). These lesions as shown in Figures 2 and 3 were interpreted to be possibly caused by neurocysticercosis. Serology performed with an Enzyme-linked Immuno-Electro Transfer Blot (EITB) assay confirmed that the lesions are definitively caused by Taenia Solium. As a management plan, the antipsychotic treatment has been stopped, and antiparasitic albendazole has been considered in the treatment for active neurocysticercosis and its neuropsychiatric manifestations.
As the first impression, the medical team in the emergency department leaned towards a psychiatric disorder as a first differential rather than an infectious disease. From the patient's history, we learn that the patient also had a TBI which brings up degenerative disease secondary to traumatic event as a secondary potential differential making the suspicion of neurocysticercosis as the top differential low. What makes neurocysticercosis diagnosis complicated in early investigation is the fact that it has an acute to chronic timeline where multiple events can happen in between the exposure to the pathogen until the onset of signs and symptoms are manifested. We consider that this is a flagrant example of a disease presentation where life events can remarkably affect the incidence of schizophrenia spectrum disorder secondary to neurocysticercosis. The diagnosis of neurocysticercosis can be tricky and challenging. The physicians in the emergency department should proceed with a holistic approach and start with a thorough history, considering a collateral history especially from the patient's family since the information given by the family in case of neuro-psychiatric disorders and emergencies can be extremely accurate and helpful. The investigation should also promptly focus on blood work and neuroimaging techniques, such as MRI or CT scans, essential to visualize the cysts in the brain or spinal cord. Ultimately antibody serology test for Taenia Solium should be performed as a diagnostic confirmatory testing. Considering the non-contrast head CT images (Figure 2 and Figure 3) in our case, it showed calcified lesions which have been shown to be a sign of chronic cerebral cysticercosis. However, these calcified lesions which are secondary to granulomatous reactions can be considered a nonspecific sign because they can be seen in other illnesses such as previous toxoplasmosis. Thus, we highly recommend the rigorous use of guidelines for the clinical management of patients with neurocysticercosis (NCC) developed by a panel of the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH).9 These guidelines can be very helpful in the diagnosis process intended for infectious disease specialists, psychiatrists, neurologists, neurological surgeons, internists, pediatricians, and family practitioners. The neurocysticercosis-induced psychotic disorder is considered a rare disease, but many experts consider this due to it going unrecognized and thus underreported.8-12 Therefore, these guidelines are indeed a supportive framework for neurocysticercosis diagnosis, which might be very supportive in the diagnosis of neurocysticercosis challenging clinical presentations, as in the case we have seen in this paper. This framework has been developed to be followed in the diagnostic process in which clear and comprehensive standards are provided and demonstrated and which are founded on a multidisciplinary clinical approach. Using these guidelines can help not only the clinicians in the investigation but also prevent complications and progression of symptoms and, eventually, patient suffering.8-12
Through this paper, we also call for and encourage further research on the association between neurocysticercosis infection and psychotic features for education purposes in emergency settings. This should be created collaboratively between the clinicians, investigators, and experts in psychiatry and infectious disease. We also encourage clinicians in primary care and emergency units to be mindful and give special consideration to patients with a history of living in or coming from an endemic area of neurocysticercosis when presenting with any neuropsychiatric symptoms. Furthermore, physicians should consider neurocysticercosis in the differentials when encountering a patient with new onset altered mental status, especially if the patient has had any link to an endemic area. Physicians should also be familiar with some clinical criteria and specificities that may distinguish neurocysticercosis infection from psychiatric disorders. We emphasize that clinicians to be mindful when using the antipsychotics because the emergence of severe refractory psychosis during treatment with antipsychotics can be seen in patients with neurocysticercosis.8-12 It is estimated that 8% of patients with neurocysticercosis infection initially present with psychiatric disturbances such as signs and symptoms of schizophrenia, dementia, and other manifestations.8-12 Infectious causes must be considered in the workup and investigated by the physician before initiating any antipsychotic treatment to avoid severe refractory psychosis during treatment. In summary, consideration of neurocysticercosis in patients with psychotic symptoms coming from endemic regions is essential to ensure accurate and prompt diagnosis and appropriate treatment. Clinicians in the emergency department should emphasize the importance of a comprehensive medical assessment and a multidisciplinary approach using the guidelines when evaluating patients with neuropsychiatric symptoms.
Differentiating between primary psychiatric disorders and neurological conditions can be challenging in in the emergency settings because the clinical presentation of neurocysticercosis can resemble that of schizophrenia, bipolar disorder, or other mental illnesses. Therefore, clinicians need to be mindful of the possibility of neurocysticercosis and consider it in the differential diagnosis, especially in patients coming from endemic regions. Neurocysticercosis can often be successfully treated with antiparasitic medications and, in some cases, surgical intervention to remove cysts. Suppose a patient with neurocysticercosis is misdiagnosed with a primary psychiatric disorder and treated with antipsychotic medications alone. In that case, it may not address the underlying medical issue and could exacerbate the patient's presentation and lead to severe refractory psychosis, which is potentially harmful. Finally, from a public health perspective, we believe that identifying and treating neurocysticercosis is important not only for the patient but also to contain the public health burden that may result from misdiagnosis. Proper diagnostic guidelines adoption and treatment that rely on a collaborative and evidence-based framework can help the investigation and diagnosis of neurocysticercosis and prevent further exacerbation.
KB devised and oriented the paper and set up the main conceptual ideas; NJ and KD created the case, collected the relevant case data from the clinical settings and the literature and bibliographic sources and processed the writing and editing of the manuscript; KB reviewed and reinforced the paper overview. All authors have read and agreed to the published version of the manuscript.
The data presented in this paper are available on request from the corresponding author.
None.
The authors declare no conflict of interest.

©2023 Jagram, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.