MOJ
eISSN: 2381-179X


Case Report Volume 12 Issue 2
1Departamento de Cirugía, Hospital de Especialidades “Bernardo Sepúlveda Gutiérrez” Centro Médico Nacional Siglo XXI, IMSS, Mexico
2Departamento de Cirugía, Hospital General de Zona No. 1-A “Dr. Rodolfo Antonio de Muchas Macías”, Mexico
Correspondence: Dr. Guerrero Gómez Alan, Departamento de Cirugía General, Hospital de Especialidades “Bernardo Sepúlveda Gutiérrez” Centro Médico Nacional Siglo XXI, IMSS, Av. Cuauhtémoc 330, Doctores, Cuauhtémoc, 06720 Ciudad de México, Tel 5540302706
Received: September 17, 2022 | Published: September 27, 2022
Citation: Guerrero-Gómez A, López-Alvarado MI, Arroyo-González MA, et al. Duodenal metastasis of breast cancer, a rare entity: case report. MOJ Clin Med Case Rep. 2022;12(2):33-36. DOI: 10.15406/mojcr.2022.12.00415
Breast cancer currently remains the most frequent malignant tumor in women in our country as well as worldwide. The first place of most frequent distant dissemination reported by frequency is the bone (51%), followed by the lung (17%), brain (16%) and liver (6%), multiple disseminations with 10%. Gastrointestinal metastases are rare entities, so we present a case of a 54-year-old female with a diagnosis of lobular breast cancer diagnosed 2 years ago and treated with left radical mastectomy and hormone therapy, in her evolution with discovery of metastasis bone and gastrointestinal at the duodenal level that determines an occlusion of 60%. Finally treated with palliative purpose through Braun anastomosis. There is a shortage in the literature on the gastrointestinal involvement of breast cancer, and in our country even more so we present a case report on this type of metastasis in order to help opportuned recognition of the symptoms with which it can occur and thereby give effective management.
Keywords: lobular breast cancer, duodenal metastasis, intestinal obstruction
Breast cancer is the most frequent malignant tumor in women worldwide. In Mexico, it is reported that 97 323 people died of malignant tumors in 2020. Of these, 7,880 were due to malignant breast tumors, which is equivalent to 8% of this total, with a high rate of deaths in women aged 60 years or older (49.08 per 100,000 women in this age group).1 The first most frequent site of distant dissemination reported by frequency is the bone (51%), followed by the lung (17%), brain (16%) and liver (6%). Multiple dissemination is reported in 10%.2
Histologic studies have revealed that lobular carcinoma metastasizes to the same metastatic sites as ductal carcinoma; however, lobular carcinoma frequently metastasizes to unusual sites such as the gastrointestinal tract, peritoneum, and adnexa.3 Gastrointestinal tract metastases of mammary origin are considered rare; occurrence in autopsy series ranged from 8% to 35%.4 The most frequent site of metastases was the peritoneum at 46%, followed by the stomach (17%), colon (15%), and small bowel (15%).3 There is a scarcity in the literature on the gastrointestinal involvement of breast cancer, and in our country even more so, so we present a case report on this type of metastasis in order to help the timely recognition of the symptomatology with which it can present and thus provide effective management.
54 year old female patient with diagnoses of: Early Endometrial Cancer 2000 treated with Total Abdominal Hysterectomy + Left Lobular Breast Cancer 2020 treated with Left Radical Mastectomy + Hormonal Therapy currently with antrasol + Vertebral metastases L4-L7, costal arches, right femur , left shoulder, iliac bone in treatment with bisphosphonates and gastroesophageal Reflux + Esophagitis Grade A of Los Angeles. Hiatal hernia type 1.
The patient was admitted in 19.03.22 with a condition characterized by oral intolerance, nausea, vomiting of gastroalimentary content, increasing in frequency and number, epigastric pain 6/10 VAS, gas channeling, without bowel movements. On admission to the surgical floor, he refers 2 emetic episodes of bloody characteristics. She reported not tolerating the oral route for 5 days and not having had a bowel movement for 2 days. The patient had already been in outpatient follow-up with general surgery who requested esophagogastroduodenal series and subsequent panendoscopy for her episodes of oral intolerance, which she reports:
Esophagogastroduodenal series (30.09.2021): Gastroesophageal reflux GII, hiatal hernia type 1, gastric inflammatory process (Figure 1).
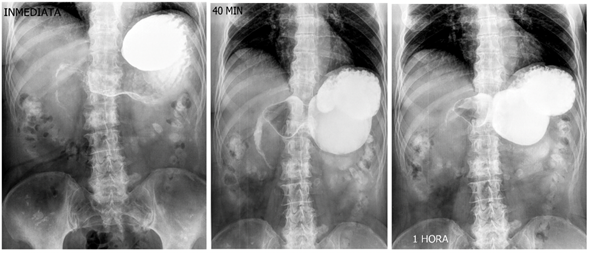
Figure 1 Esophago-gastro-duodenal series: Gastroesophageal reflux GII, duodenal stenosis, gastric inflammatory process, expiration of the ileocecal valve three hours after the start of the study.
Panendoscopy (09/23/2022): Esophagitis A de los Angeles, Hiatal hernia type 1 (3cm), Hill's type II diaphragmatic opening, chemical pangastropatia, 60% frankable stenosis at duodenal bulb level at the expense of pseudopolyps of origin to be determined, duodenogastric reflux (Figure 2).

Figure 2 Panendoscopy: Los Angeles grade B esophagitis, hiatal hernia type 1 of 3 cm, chronic reactive gastropathy in body and antrum, retentive stomach secondary to duodenal stenosis, moderate acute erosive gastropathy in body and antrum. Stenotic duodenal tumor, probably metastatic. A biopsy of the duodenal tumor was taken.
On her first day, the patient presented decreased pain at the epigastric level, she had a nasogastric tuve that reported an output of 300cc with no characteristic of gastro alimentary or intestinal debris, clear liquid with slight hematic debris was observed. Laboratories: Potassium 4.5, Sodium 145, Chloride 105.2, Leukocytes 16, Creatinine 1.6. An abdominal tomography was performed, reporting blastic lesions in vertebral bodies and iliac bone, thickening of the duodenal arch and part of the jejunum, the rest of the intestine without evident data of alterations + diverticulosis without data of complication (Figure 3).
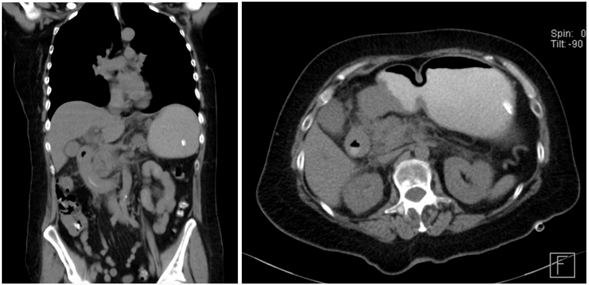
Figure 3 Computed tomography: blastic lesions in vertebral bodies and iliac bone, thickening of the duodenal arcade and part of the jejunum, rest of intestine without evident data of alterations.
At the clinical level with persistence of emetic episodes, intestinal transit is performed which reports filiform passage of contrast at the duodenal level, 3 hours to pass to the rest of the intestine. Her labs 4 days later with normal parameters Leukocytes 9.5, Hemoglobine 12.1, Creatinine 0.5, Potassium 3.8, Sodium 144, Urea 42.4. She was consulted with the Endoscopy service who supported us for the placement of a nasojejunal tube, which was successfully placed, an elemental diet of 900 cc every 8 hours via nasojejunal tube was started, referring vomiting after that, however in its second well tolerated application, a control X-ray was performed to review the placement in which it was observed to be in the stomach.
Medical Oncology was consulted with the suggestion of palliative surgical treatment, out of systemic treatment because it was stage IV. The Oncosurgery service performed a Braun's omega gastrojejunoanastomosis with the finding of a tumor infiltrating the entire duodenum from the 2nd portion to the angle of Treitz with bleeding of 50 cc. Pathology report: Metastatic breast carcinoma in the region of the duodenal bulb. Immunohistochemistry: CK7: POSITIVE, CDX2 NEGATIVE, GATA 3: POSITIVE.
Approximately 25% of all breast cancer metastases occur within the first 5 years of diagnosis of early stage disease.3 The most common site affected by breast cancer metastases at the gastroduodenal level is the stomach presenting as lymphoplasmacytic lymphitis, with an incidence of approximately 15% in autopsies.6 At the small bowel level, as already mentioned, the presentation is uncommon; the most frequent are primary malignant neoplasms, and as a consequence of metastasis, melanoma, colon cancer, cervix, etc.
In breast cancer it has been reported that the metastatic patterns of lobular and ductal carcinoma differ considerably. Most series report a higher propensity of lobular carcinoma to metastasize to the gastrointestinal tract, gynecological organs or peritoneum.5
The difference could be due to cell size or shape with physical properties that favor certain areas with a microanatomy more conducive to arresting this cell type. Another possibility is that the ovarian or peritoneal microenvironment provides growth and survival factors that favor lobular carcinoma cells over those of the ductal subtype. Other molecular or biological differences could explain this peculiar pattern of metastasis. It has been shown that loss of expression of the cell adhesion molecule E-cadherin in invasive lobular carcinoma may decrease cell adhesiveness and facilitate this type of infiltration.7
The symptoms that occur after gastrointestinal involvement are not well clarified and may behave as a primary symptom. Among those reported in the literature are early satiety, gastrointestinal tract bleeding, intestinal obstruction, anemia and weight loss.8
Diagnostic imaging is rarely specific. It is also well known that benign or second primary processes are more common than gastrointestinal metastases in patients with a history of previous breast cancer. Upper gastrointestinal endoscopy with biopsy is the recommended option for the diagnosis of this type of entity.9 Our patient presented with data of upper intestinal occlusion without having metastasis of her primary as a first suspicion, in addition to the fact that metastases often present after 5 years as mentioned, in our case only 2 years had passed, it was only after imaging and biopsy studies that we were able to confirm the metastasis.
With this case we want to demonstrate the clinical presentation of a rare entity in the clinical setting, how it was approached and treated since the evidence in the literature is very little. There are few cases reported worldwide, and the objective is to help in the timely identification of this type of metastasis in patients with breast cancer.
To the personnel who collaborated in the preparation of this report.
The authors declare that they have no conflict of interest.

©2022 Guerrero-Gómez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.