MOJ
eISSN: 2381-179X


Case Report Volume 11 Issue 5
Registrar in Emergency Medicine, National Hospital of Sri Lanka, Srilanka
Correspondence: Ishan N Perera, Registrar in Emergency Medicine, National Hospital of Sri Lanka, Srilanka
Received: August 22, 2021 | Published: September 10, 2021
Citation: Perera IN. A difficult airway made worse by apprehension: an obese young male with COVID 19. MOJ Clin Med Case Rep. 2021;11(5):129-134. DOI: 10.15406/mojcr.2021.11.00398
Intubation of a critically ill patient in the emergency department is always considered a difficult airway. Timing, patient factors which are not optimized, and intubation done by infrequent intubators. Add to this the complications and demands of Covid 19 pandemic which make crash intubations a thing feared for personal safety as well as successful completion of intubation without complications. If the patient has intrinsic comorbid conditions contributing to a difficult airway, worse the procedure would be. Furthermore, Covid pneumonia presents its own challenges in preoxygenation, timing of the intubation, ventilation of the patient and transport as well. This is a patient I came across during the third wave of covid19 pandemic in Sri Lanka, working in the Emergency department night shift. He came in acute respiratory distress and required intubation and ventilation.
A 50 years old male patient was brought in by emergency service ambulance after being notified by the public health inspector who had quarantined 50 men in a hostel when most of them tested positive for Covid following an exposure at work. This gentleman was one of the confirmed PCR positives. He was obese with a body weight of 140kg. he gradually became dyspneic over the last 2 days, logistical issues delayed admission to hospital till 7pm on the third day when he was finally brought to the emergency department in severe respiratory distress. His background was obtained by contacting the spouse who informed that he was snoring for as long as they’ve been married but had no poor sleep, daytime somnolence nor morning fatigue and that his exercise tolerance was good. He was never screened for diabetes, hypertension nor hyperlipidemia as he was active and well. He had a family history of ischemic heart disease and diabetes from the paternal side. He had no known allergies. No past surgical history. He had never smoked according to his wife and partaken alcohol in social gathering.
The patient was able to maintain his airway. He was in severe respiratory distress, with a respiratory rate of 34 -38 breaths per minute but only achieving 68% peripheral saturation while on a Hudson mask with 10L of oxygen. He was able to speak in words. Auscultation of the lungs revealed widespread crepitations with equal breath sounds on both lung fields. Percussion note was equal on both sides of the chest. His heart rate was 124 beats per minute, regular, good volume. Blood pressure was 145/89mmHg. His sensorium was normal. He had a temperature of 1010 F. there were no rashes of lymphadenopathy.
He didn’t have a beard or external facial deformities. His mouth opening was good, inter incisor distance 3 patient finger breaths, hyo-mental distance was 3 patient finger breaths and thyro- hyoid distance was less than 2 patient finger breaths. Due to increased exposure risk Mallampati score was not assessed. Neck mobility was reduced due to subcutaneous tissue around the neck and back but there was no pain on movement.
Diagnostic focus and assessment
On admission capillary blood sugar (CBS) and venous blood gas (VBG) was obtained at intravenous canulation. CBS was 144mg/dL. The VBG reports shown below showed type 2 respiratory failure. An inward Chest Xray request was made. Full blood count, renal functions, liver functions with serum albumin level, C-reactive protein, Blood culture was sent (Figure 1,2) (Table 1).
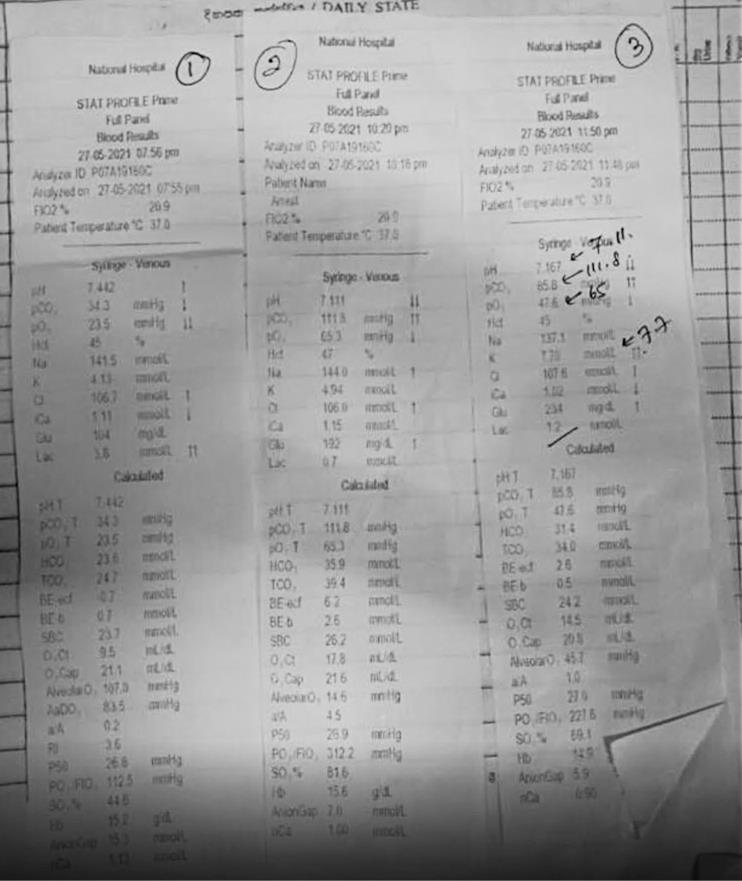
Figure 1 Full blood count, renal functions, liver functions with serum albumin level, C-reactive protein, Blood culture.
|
Parameter |
VBG 1 – admission |
VBG 2 – admission + 2H |
VBG 3 – admission + 3H |
|
pH |
7.442 |
7.111 |
7.167 |
|
pCO2 |
34.3 |
111.8 |
85.8 |
|
pO2 |
23.5 |
65.3 |
47.6 |
|
Na |
141.5 |
144.0 |
137.8 |
|
K |
4.13 |
4.94 |
7.7 |
|
Glucose |
104 |
192 |
234 |
|
Lactate |
3.8 |
0.7 |
1.2 |
|
Ca |
1.11 |
1.15 |
1.02 |
|
HCO3 |
23.6 |
35.9 |
31.4 |
Table 1
Therapeutic focus and assessment
The patient was taken to a resuscitation bed on arrival by the waiting covid19 resuscitation team already in full personal protective gear, propped up, connected to the monitor and as he was able to maintain his airway on his own, 15L/minute oxygen via a non-re breathing mask was applied. The saturation picked up to 75% to 78%. Respiratory rate and heart rate remained same.
Two 18G canulae were inserted on both arms and blood taken for investigations from one side while a maintenance fluid, 0.9%NaCl solution was provided at 100ml/hour rate on the other. Capillary blood sugar was 144mg/dL. Venous blood gas showed type one respiratory failure with respiratory alkalosis and adequate metabolic compensation. Serum Lactate was 3.8mmol/L.
His breathing was immediately supported with non-invasive ventilation, a tight fitting non vented mask connected to a viral filter and then to the expiration port was used. Continuous air way pressure at 10 cmH2O.
Paracetamol 1g IV for fever, IV ceftriaxone 1g and Deep vein thrombosis prophylaxis with Subcutaneous Enoxaparin 40mg stat was administered.
Patient was kept under observation. He improved his oxygenation up to 86–90% with vital signs staying same. A urinary catheter was inserted, and he produced 350ml of dark urine. A 500ml 0.9% NaCl bolus was administered followed by 100ml/h maintenance. At end of 2 hours repeat VBG was done to see the progression.
The respiratory compensation and positive supports had failed, and he was going into type two respiratory failure. Immediately the covid19 intensive care team and medical teams were informed regarding the deteriorating patient and that he needs invasive ventilation. The respiratory supports were escalated to bi-level positive pressure support inspiratory pressure (IPAP) of 16cm H2O and expiratory pressure (EPAP) of 10 cmH2O with 25L/minute O2. While an ICU bed was allocated, an intubation plan was made.
On call anesthesia team was informed regarding the patient and the possibility of a difficult airway coming up, to be on standby if escalation is needed.
The team was one airway doctor with airway nurse and circulation nurse near the patient. One running nurse on standby. The patient would be intubated in the ETU and stabilized on the transport ventilator prior to transfer.
The intubation plan was agreed upon by the team, plan A would be traditional laryngoscopy with number 4 blade, bougie and size 8mm tracheal tube with 7.5mm as back up. Plan B would be to use a size 4 Laryngeal mask airway (LMA) size 3 as back up. Plan C would be Bag and mask ventilation with early front of neck airway with size 6 tracheal tube.
Induction agent would be Ketamine 1.5mg/Kg, 200mg. fentanyl 100micg to blunt intubation response. Full dose of Suxamethonium at 1.5mg/kg, 200mg. atropine 0.6mg/ml solution and adrenaline 1:10000 0.01mg/ml solution as push dose pressor kept at the ready. With these the plan was ready.
The patient was informed of his critical state and gave consent for the proposed course of treatment. His spouse who was at home in Kurunegala was contacted over the phone and informed regarding the patient’s current condition and planned course of treatment (Figure 3,4).
He was stabilized on Bilevel NIV and SpO2 was at 80%. An arterial blood gas was obtained. It showed that his hypoxia had worsened despite acidosis and CO2 levels improving. As a new finding the potassium had gone up to 7.7mmols and glucose was 234mg/dl. Intravenous 10% calcium gluconate 10ml bolus was given and a soluble insulin 10 units in 25% dextrose 25ml infusion started to infuse over 10minutes. Repeat VBG in 15minutes showed a potassium of 5.1mmols/L.
He was placed in the ramp position. Suction handle checked and kept at the ready. While patient on BiPAP induction started. Fentanyl first, then Ketamine and once patient is sedated Suxamethonium was injected. Once 1 minute had passed with fasciculations disappearing the NIV mask was removed and oral cavity sucked out. The laryngoscopic view was Cormack and Lehane 1. Successful intubation with the size 8mm tracheal tube achieved under direct vision and cuff passed 2cm distal to the vocal cords. Lip level was 20cm’s. Cuff inflated to 25mmH2O and connected to viral filter then to the capnogram then the ambu bag. As the ambu ventilation started chest rise was symmetrical and misting of the tube noted. capnography reading came swiftly with a good wave form at 55mmHg. The patient was connected to the transport ventilator and given IV Atracurium 0.2mg/kg (28mg) bolus for continued paralysis.
The Ventilator settings:
Mode: SIMV (Synchronized Intermittent Mandatory Ventilation) VC (Volume Controlled) ventilation
TV – 6ml/Kg ideal body weight (80Kg)=480ml PEEP: 10cmH2O
PIP: 15cmH2O
Pplat: 30cmH2O I:E : 1:2
Rate set at 30 (patient’s own rate pre intubation) FiO2: 100%
Sedation started with IV Midazolam 3mg bolus then 1mg/h infusion. Morphine 1mg per hour infusion continued for pain relief.
Bolus atracurium 14mg every 30 minutes for muscle paralysis till transfer. Post intubation vitals were;
HR–118 regular good volume BP – 139/85mmHg
MAP–103mmHg
SpO2–80% at FiO2 100%.
A nasogastric tube was inserted. Urinary output was 120ml for last 3 hours. After assessing his IVC which showed a collapsibility index of more than 50%.4 Another 250ml 0.9% NaCl bolus was administered. Maintenance fluids were continued then on.
Patient transferred to Covid19 ICU for further care with these conditions.
Follow up and out comes
The patient deteriorated over time with worsening oxygenation despite increasing supports. He succumbed to the illness the following day.
Covid19 is a world pandemic that has claimed many lives. This is caused by a Single strand RNA corona virus, who is the newest member of the SARS, MERS family of corona viruses.1
It causes a respiratory tract infection. 80% of infected are either asymptomatic or develop very subtle upper respiratory tract symptoms. 15% will have fever and lower respiratory tract infection and 5% will go on to develop severe disease which starts as a severe respiratory tract infection rapidly progressing to acute respiratory distress syndrome and associated multi organ dysfunction.1
Our index case fell into this severe disease category.
In managing this severe pneumonia, the Sri Lanka College of Anesthesiologist and Sri Lanka college of physicians’ guideline was use as a guide.2 (Table 2)
|
Presentation |
Disease Category |
|
PositiveCOVID-19/SARS-CoV-2diagnosticvirologictest Has signs and symptoms of COVID-19/SARS-CoV-2 but do not have shortness of breath, is not dyspnoeic and chest imaging is normal |
Asymptomatic individuals |
|
Has symptoms and signs of COVID-19/SARS-CoV-2 pneumonia (fever, cough, dyspnoea, respiratory rate upto30/min, crepitations, etc), with low SpO2¿94% on roomair*. But does not have features of severe pneumonia (See below).Chest imaging will show evidence of COVID related changes.”Lower SpO ›needs to be considered in patients with chronic respiratory diseases. |
Moderate disease |
|
Has features of severeCOVID-19/SARS-CoV-2pneumoniasuggested by; 1) SpO2<90%with maximum oxygen supplement as standalone criteria OR 2) SpO2<94%with0t Supplement AND Evidence of severity assessed by the following criteria • Respiratory rate>30/min, excessive use of accessory muscles, and thoraco-abdominal dis-synchrony • Radiographicinfiltrates->S0%multi-lobarinfiltrationsP/Fratio<300(PartialpressureofOxygen/FractionofOt • S/Fratio<23S(Saturation/Fraction of Ot) • Haemodynamic instability; • Heart rate>120/min • SBP<90mmHg • Lactate>2mmol/L |
Severe disease |
Table 2
According to their classification our index case fell into the severe disease category.
This severe disease is brought on by the dysregulated immune response and microvascular thrombosis within the pulmonary alveolar capillaries giving rise to acute respiratory distress syndrome.3 This is worsened by secondary bacterial infections and increased thrombogenicity.3
This is the reason behind our initial medication for the index case, intravenous Ceftriaxone for possible secondary bacterial infections, intravenous dexamethasone for the blunting of immune over activity and enoxaparin for increased thrombogenicity as prophylaxis for deep vein thrombosis.1,2,3
He was in respiratory distress as he came in and saturation was 64% on Hudson mask with 10L of oxygen. The increasing non-invasive supports failed to achieve the recommended 94%. His S/F ratio was 80% SpO2 while on 0.7 FiO2, 133. He was upgraded to CPAP following the second VBG finding of type one failure to improve oxygenation. Eventually he became exhausted while an ICU bed was being organized, which became apparent with the presence of type two respiratory failure in the 3rd VBG. As a temporizing measure Bilevel non-invasive ventilation with a non-vented mask plus viral filter before expiratory port and this was continued till the intubation to maintain optimal oxygenation.1,2,5
The induction agent of choice was ketamine with its inherent hemodynamic stability because the index case being critically ill.2,5 Response to intubation minimized with fentanyl and after correction of the potassium level Suxamethonium was chosen as paralytic agent, as it provides the best intubating conditions rapidly. The dose was full dose as recommended.2,5 The index case having hyperkalemia on the third VBG which was treated with IV soluble insulin 10 units over 10 minutes.
Only three members were there for the intubation in full personal protective gear, airway doctor, airway nurse and circulation nurse.5
The vortex approach was used to plan for the difficult intubation as the patient was obese, had a history of snoring, his thyro-hyoid distance was less than two finger breaths and had limited neck extension.5,6
Plan A was cuffed endotracheal tube internal diameter 8mm and size 4 Macintosh blade with back up sizes. Plan B was laryngeal mask airway size 4 and back up sizes. Plan C was bag mask ventilation with V&E hold until early front of neck airway creation.2,5,6 Even though the recommendation was to use video laryngoscopy as the initial tool, this was not available for our index case. It is recommended by the Difficult airway society guidelines to follow a vortex approach during transition from one plan to the other and at each attempt, taken as an experienced airway operator inserting the laryngoscope blade into the mouth, optimization of positioning, suctioning and instruments must be done.7
To minimize the exposure and aerosolization of the virus the most experienced person must attempt the intubation, so during our index case it was the registrar in emergency medicine and clearly verbalized plan, with vortex approach. We didn’t use apnoeic oxygenation also due to risk of disease spread, recommended by local and difficult airway guidelines.2,5 (Figure 5)
The ramp position is known to improve laryngoscopic view in the obese patients. The patient will be propped up on pillows to elevate the head and ramp the back to get the patients tragus in line with the sternum and face parallel with the ceiling. The reverse Trendelenburg position would have helped more but the bed our index case was place didn’t have tilt function. The bed position was elevated to the optimal height for the operator. Adequate suctioning was kept at the ready.
Induction agents needed to be selected that will not hemodynamically compromise this critically ill patient and ketamine was the choice. 280mg of Ketamine (2mg/Kg dose was taken to the syringe and the circulation nurse was advised to only administer 200mg and look for the response. Suxamethonium on the other hand needed to be administered in full dose to maximize paralysis in the shortest time.
Once the intubation plan was in place the transport ventilator was checked and pre-set with recommended settings for ‘type 2’ or ARDS type Covid pneumonia. The reason was the index case had tachypnoea, severe respiratory distress, widespread B lines on lung ultrasound, diffuse infiltrative opacities on both lung fields in the chest x ray and he improved with application of positive pressure support placing him in type 2.2
A PEEP of 10 (10-20) with low tidal volume 6ml/Kg ideal body weight (4-6ml/Kg) approach was taken. The respiratory rate was kept high to match patient’s native rate. The driving pressure has to be 15cmH2O to minimize volutrauma and barotrauma, so this had to checked once ventilation was established.
The team members were fully dressed in PPE and after positioning of the patient, rapid sequence induction was done. We were able to pass a size 8mm tracheal tube in the first pass with cuff inserted approximately 2cm beyond the vocal cords. Lip Level was 20cm. then the cuff inflated to 25cmH2O (25 – 35cmH2O recommendation)2,5 a Viral filter attached to the tracheal tube then capno gram and then to the amu bag and ventilated. The tube was seen to mist. Capnogram reading was 55mmHg with a good wave form. The tube placement couldn’t be checked by auscultation due to PPE gear.
The patient was stabilized on the transport ventilator. The driving pressure was 15cmH2O within recommended levels. Peak inspiratory pressure was 25cmH2O. Plateau pressure was checked, it was 26cmH2O.
When connected to the ventilator the saturation remained at 80% then slowly rose to 88% with FiO2 of 1.0.
Sedation was maintained with intravenous midazolam 3mg bolus then 1mg/hour infusion with morphine 1mg/hour infusion for pain relief. To prevent patient ventilator asynchrony and minimize ventilator induced lung injury. The muscle paralysis is very important as well to minimize exhausting the patient and stop bucking. In Atracurium 28mg injected and will be repeated every 30 minutes.
Continuous monitoring of the vital signs was carried out to observe for any hemodynamic collapse following the paralysis and sedation. Once ventilated the increased thorasic pressure can impede venous return and cause hypotension. There for these vital signs monitoring is essential.
Then the covid19 intensive care team came and took over the patient and transported him to the ICU. When he is transferred from the transport ventilator to the ICU ventilator the ventilator will be stopped, endotracheal tube clamped and then connected to the new ventilator and released to minimize aerosolization of virus.
None.
None.
There is no conflict of interest in this case report.
Informed consent was taken from the spouse of the index case for publication of this case report.

©2021 Perera. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.