MOJ
eISSN: 2381-179X


Mycobacterium tuberculosis meningitis (TBM) is a severe manifestation of extra-pulmonary tuberculosis.TBM, which is a medical emergency, remains a major cause of serious illness in many parts of the world, although the exact incidence rates and prevalence are unknown. TBM is difficult to diagnose because of broad clinical spectrum and may be non-specific, thus hindering early diagnosis.1 Nevertheless, delayed treatment is strongly associated with death and empirical anti-tuberculosis therapy should be started promptly in all patients for whom, the diagnosis of TBM is suspected. We describe a case of tuberculous meningitis that appeared as feverish pure form for which the use of Gene Xpert MTB / RIF test enabled us to obtain an etiologic diagnosis thus anticipating the bacterial culture results.
A 41 years old Filipino man who had been living in Italy for 19years and had not visited his country of origin in previous 12months for whom there was no history of comorbidity. Hospitalization in June 2016 for intermittent fever (39-40°C), which occurred in a period of approximately 15days, and a right frontal headache. No other apparent organ localizations. Upon entering the ward, the general and neurological objectivity were negative. No abnormalities were noted in any blood tests, inflammatory markers were normal, and a whole body CT was negative. Quantiferon test positive and Mantoux weakly positive, negative HIV serology. On the sixth day in hospital, 21days after the onset of fever, double vision, ptosis and anisocoria of the left eye were observed in the patient. MRI with medium contrast showed initial dilation of the supratentorial ventricular cavity (Figure 1), leptomeningeal impregnation tank prepontine, perimesencefalic, sovrasellare and silviane fissures and subtle leptomeningeal enhancement even at the level of the optic tracts and chiasm (Figure 2).
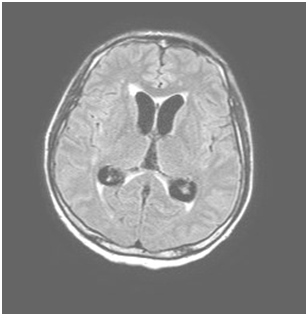
Figure 2 MRI with contrast showed leptomeningeal impregnation tank prepontine, perimesencefalic, sovrasellare and silviane fissures and subtle leptomeningeal enhancement even at the level of the optic tracts and chiasm.
A CSF showed marked hypoglycorrhachia (18mg/dl), high protein level (324mg/dl) and 760white/mmc blood cells (90% lymphocytes). Direct examination with Zielh-Neelsen staining was negative as well as PCR performed with Strand displacement amplification method (BDProbeTec ET MTC). Nonetheless, TB meningitis was suspected and treatment was started with four drugs isoniazid, rifampin, ethambutol and pyrazinamide, enhanced by the addition of both 750mg levofloxacin and 20mg dexamethasone daily.
Due to the appearance of hypertensive hydrocephalus, an external CSF shunt was positioned, which enabled us to collect a second sample of liquor seven days after the start of treatment. The second sample was negative for BAAR direct microscopic examination, but weakly positive for MTB-DNA, detected with the Gene Xpert MTB/RIF molecular method. The test, which exploits a rapid PCR patented by Cepheid, is also able to check whether the tuberculosis bacillus strain is or is not resistant to the most common drug used for the treatment of tuberculosis, Rifampin (rpoBgene for rifampin resistance). The World Health Organization has recommended use of the Xpert MTB/RIF assay as an initial test for diagnosing tuberculous meningitis. In a systematic review and meta-analysis including 18 studies, the sensitivity and specificity for the Xpert MTB/RIF assay in cerebrospinal fluid (compared with culture) were 81 and 98 percent, respectively. Fever and headache disappeared seven days after starting the specific TB therapy and following the placement of CSF external shunt with progressive clinical improvement.
The patient is currently in good health, all his blood tests are normal and ptosis and anisocoria of left eye have completely disappeared.
The patient does not present any neurological deficit. High-resolution images show a good clinical picture, including the most recent MRI brain scan performed. The strain, grown from the first CSF, proved to be resistant to isoniazid and streptomycin. After the first two months, the patient continued TB treatment with rifampin, ethambutol, with the addition of levofloxacin. It is important to note that the patient comes from the Philippines, which is considered to be a highly endemic country for all types of tuberculosis. The World Health Organization estimated an incidence of more than 300 cases per 100.000 inhabitants per year with a percentage of 3-6% of MDR-TB strains among new cases. The patient will continue anti-tuberculosis therapy for an additional 10months.
Tuberculous meningitis (TBM) is the most severe form of secondary tuberculosis and represents <3% of extrapulmonary forms. Clinical symptoms include fever lasting a median of 14days, headache, double vision, impaired sensorium, meningeal signs, cranial nerve involvement, papilledema. The CSF is usually clear, with elevated protein and lowered glucose concentrations and mononuclear pleocytosis (>30% lymphocytes). The main imaging criteria for diagnosis are based on detection of: hydrocephalus, basal exudate, tuberculoma, heart attack, arachnoiditis opto-chiasmatic.
The surety of the diagnosis, as determined by a recent Consensus,2 was carried out by performing of alcohol- acid fast bacilli (sensitivity 37%) or by culturing positive for BK (sensitivity 52%) or with MTB-DNA positivity to rapid molecular amplification tests. The clinical case described is one of the first examples of pure febrile forms, late onset of neurological symptoms and constant normal inflammatory markers. By using the recent more specific and sensitive molecular marker tests such as the Gene Xpert MTB/RIF, it was possible to confirm the etiologic diagnosis of tuberculous meningitis, already made on the basis of clinical evidence, as early as seven days from the start of the antituberculous chemotherapy as well as the sensitivity of the strain to rifampin. Next-generation molecular diagnosis may prove to be essential for early diagnosis of tuberculosis, especially the extrapulmonary forms that are on the rise globally.3–5
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.