MOJ
eISSN: 2381-179X


Case Report Volume 4 Issue 5
Internal Medicine Department, Cairo University, Egypt
Correspondence: Shaimaa Elkholy, Internal Medicine Department, Cairo University, Egypt
Received: August 11, 2016 | Published: August 31, 2016
Citation: Elkholy S, Albitar A, Elfadl SA, et al. Diffuse nodular lymphoidhyperplasia with selective IgA deficiency syndrome presenting with intestinal lymphoma. MOJ Clin Med Case Rep. 2016;4(5):116-118 DOI: 10.15406/mojcr.2016.04.00105
Diffuse nodular lymphoid hyperplasia (DNLH) is a benign rare condition of unknown etiology characterized microscopically by diffuse hyperplasia of the lymphoid follicles of the gastrointestinal tract (GIT). It is grossly seen during endoscopy as numerous visible mucosal nodules measuring <0.5cm in diameter. It can involve any part of the GIT, mainly the small intestine, but it may also involve the colon and rarely the stomach. It may have diffuse pattern which is the most common former focal pattern which is much less common. The disease is usually associated with immunodeficiency syndromes such as common variable immunodeficiency or selective IgA deficiency syndrome. Its prognosis is usually benign but it carries the risk of malignant transformation characteristically to lymphoma. This case is a young male patient with DNLH with underlying selective IgA syndrome presented with intestinal lymphoma. This case was diagnosed retrospectively which presented a rare complication to a rare disease.
Keywords: diffuse nodular lymphoid hyperplasia, intestinal lymphoma, selective IgA deficiency syndrome
A 24-years old male presenting with chronic diarrhea that started 2years ago, it was associated with significant weight loss in the last 6months for which he sought medical advice, C.T. abdomen & pelvis was done and showed amass related to the small intestine for which abdominal exploration was done and the mass was excised which was about 25cm of the ileum and surrounding lymphnodes. Histopathology of the mass showed extra-nodal diffuse large B-cell lymphoma, also cervical lymph node was biopsied showed reactive hyperplasia and bone marrow biopsy was completely normal. Then he was diagnosed as primary intestinal lymphoma and six sessions of CHOP chemotherapy were given and patient’s manifestations resolved and he was completely free. Later on, the patient started to develop the same attacks of diarrhea again but with less frequency (about 4-5times per day) and no weight loss. Extensive work up was done and recurrence of lymphoma was completely excluded. The oncology department referred the patient to the internal medicine department for the diagnosis of the cause of persistent diarrhea.
Thorough history taking was performed which revealed that before his recent diagnosis with intestinal lymphoma, the patient had a long history of intermittent diarrhea and this was since childhood as confirmed by his mother. He sought medical advice several times quinolones or metronidazole were prescribed to him but only with partial improvement of his condition, yet with no attempts of endoscopic intervention. Physical examination of the patient was unremarkable apart from bilateral cervical lymphadenopathy previously biopsied. Laboratory work up was done in the form of complete blood count, liver profile, renal profile, electrolytes, stool analysis & C&S (repeatedly), ESR, B2 microglobulins, virology (HIV, HBsAg, antiHCVab) and all were completely normal.
Abdominal ultrasound showed uniform circumferential mural thickening of the small bowel loops, so we proceeded to C.T Enterography. As shown in Figure 1, there is diffuse uniform thickening of the small bowel loops mainly involving the ileum with no focal thickening or masses. Then upper endoscopy and colonoscopy were performed to the patient and they showed multiple tiny rounded nodules at the terminal ileum that were biopsied and revealed non-specific inflammation free of granuloma or malignancy. Then we proceeded to double balloon enteroscopy which was done by an over tube double balloon Fuji series endoscopy, which proceeded to about 200cm from the duodenal bulb. Double balloon endoscopy as shown in Figure 2, showed numerous visible mucosal nodules measuring few millimeters in diameter involving the whole part of the small intestine examined which were biopsied. Histopathology revealed chronic inflammatory enteritis with foci of lymphoid aggregates with no atypia or malignancy (Table 1).



Figure 1 C.T. Enterography of the patient that showed diffuse uniform thickening of the small bowel loops mainly involving the ileum with no focal thickening or masses.
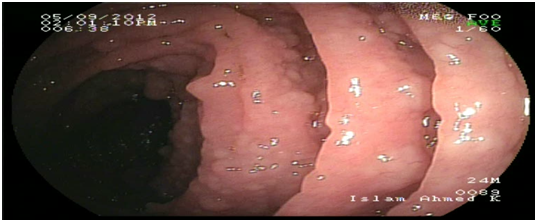
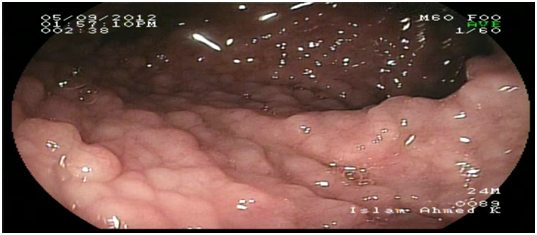
Figure 2 Diffuse small nodules scattered through the whole small intestine by double ballonenteroscopy.
Result |
Normal |
|
Ig A |
0.4 |
o.7 – 4.0g/l |
Ig M |
0.5 |
0.4 – 2.3g/l |
Table 1 Immunoglobulin assay
Then immunoglobulin assay and electrophoresis were done to the patient that showed selective deficiency of IgA.
DLNH is a rare benign condition of unknown etiology that may occur in any age group.1 It usually regresses in children and it was thought to be associated with delayed type of food hypersensitivity. In adults, it’s usually associated with immunodeficiency syndromes e.g. Selective IgA deficiency syndrome and Common variable immunodeficiency.2 DNLH is lymphoproliferative disease that is characterized by a stimulation of the B cell compartment of the lymphoid follicles that results in abnormal proliferation of these follicles.2–7 Many theories had been implemented for the underlying pathogenesis. One of the theories is the stimulation of a local immune reaction in response to certain antigens in the GIT, but yet no antigen has been identified. Another theory that it may be related to plasma cell precursors due to a maturational defect in the development of B-lymphocytes in order to compensate for functionally inadequate GITtissue.3–7
Some reports had described DNLH in adult patients without immunodeficiency and it was thought to be associated with chronic GIT infections such as Giardiasis or Helicobacter pylori infection.4,8,10 Nodular lymphoid hyperplasia generally presents as an asymptomatic disease, but it may cause gastrointestinal symptoms like abdominal pain, chronic diarrhea, malabsorbtion syndrome, bleeding or very rarely intestinal obstruction.5 One of the most important issues likely to be raised is the differential diagnosis of this condition. Due to its characteristic appearance during endoscopy which appears as innumerable small nodules involving mainly the small intestine as shown in Figure 2 limits the differential diagnosis. Familial adenomatous polyposis (FAP) and intestinal lymphoma should be taken into consideration. GIT is considered the largest lymphoid system in the body, so intestinal diseases are not surprisingly associated with the immunodeficiency syndromes. Common variable immune deficiency is defined as deficiency of immunoglobulins mainly IgG associated with IgA, IgM or both.6 Selective IgA deficiency syndrome (SIgAD) is the most common primary immunoglobulin deficiency and is defined as the isolated deficiency of serum IgA (ie, in the setting of normal serum levels of IgG and IgM) in a patient whom other causes of hypogammaglobulinemia have been excluded.6–9 About 10 -15 % of the patients with SIgAD have symptoms of recurrent sinopulmonary infections, autoimmune disorders, gastrointestinal infections, anaphylactic transfusion reactions, Food allergies and respiratory allergies are prominent.6–9 There is an increased risk of malignancy in patients with DNLH and a coexisting hypogammaglobulinemia, especially the risk of lymphoma and gastric carcinoma. This is the typical scenario of our patient that was diagnosed after his presentation with intestinal lymphoma.11 DNLH with no complications usually does not require any special treatment. However, the patients should undergo the prophylactic examinations. For patients with chronic diarrhea repeated courses of antibiotics such as quinolones or metronidazole had been reported. Also eradication of Helicobacter pylori had significant reduction in the number and size of the nodules in some studies.4–12 This causes controversy when deciding the treatment options. Following up patients without any treatment may lead to malignant progression, while surgical treatment may result in justified radical resections.
In this article we would like to highlight the extent of changes that could affect the GIT as a result of immunodeficiency syndromes. It could be simple benign lesions such as DNLH, but it also may progress to malignancy which is the worst case scenario. DNLH needs a close follow up and surveillance especially when associated with an immunodeficiency.
None.
The author declares no conflict of interest.

©2016 Elkholy, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.