MOJ
eISSN: 2471-139X


Case Report Volume 8 Issue 1
1Plastic Surgery Resident, Plastic Surgery and Microsurgery Service, Hospital Pasteur, Uruguay
2Plastic Surgeon, Plastic Surgery and Microsurgery Service, Hospital Pasteur, Uruguay
Correspondence: María Victoria Machado, Plastic Surgery Resident, Plastic Surgery and Microsurgery Service, Hospital Pasteur, 11600 Montevideo, Urugua, Tel +59897573751
Received: February 03, 2021 | Published: February 23, 2021
Citation: Victoria MM, Eugenia T, Guzmán R, et al. Posterior dislocation of the metacarpophalangeal joint of the thumb: case report and review of literature. MOJ Anat Physiol. 2021;8(1):15-18. DOI: 10.15406/mojap.2021.08.00315
Posterior dislocations of the metacarpophalangeal joint of the thumb are due to hyperextension trauma and relatively rare. We present the case of a patient in whom closed reduction was not achieved, requiring open reduction and anchoring of the palmar plate with transosseous pull out technique. A literature review focused on treatment was carried out. All authors agree that closed reduction should be the first therapeutic gesture. If this is not achieved, open reduction should be performed through a dorsal or volar approach, and there is no consensus on which is more effective, nor in terms of management of periarticular soft tissues. Reduction in this case was followed by 2-4 weeks immobilization. Results were generally good, restoring a stable and painless joint, although there might be some degree of joint stiffness.
Keywords: posterior, dislocation, hyperextension injury, metacarpophalangeal joint, thumb
Posterior dislocation of the metacarpophalangeal (MCP) joint of the thumb is rare,1–3 generally occurring in young, active patients. It is caused by hyperextension trauma; and can be classified as simple (reducible with closed techniques) or complex (irreducible with closed techniques).1,4,5
We reported a case of this pathology and a literature review of the proposed treatments. Number of patients, acute or chronic dislocation, treatment, immobilization, and obtained results were analyzed.
30-year-old male, right-handed, construction worker suffered from a thumb hyperextension trauma 3 days prior to the consultation. He presented with pain, dysfunction, edema, a shortening of the thumb, posterior displacement of the proximal phalanx and palmar palpation of the head of the first metacarpal (MC) bone (Figure 1).
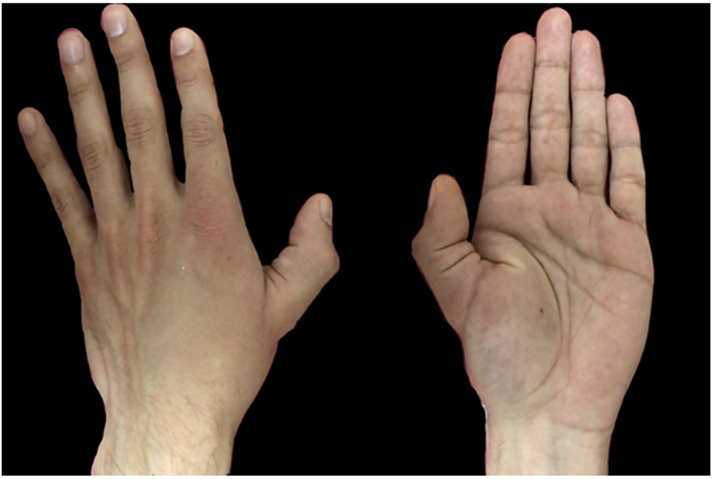
Figure 1 Shortened thumb, posterior displacement of the proximal phalanx and palmar visibility oh the metacarpal head.
Radiographs showed a posterior dislocation of the MCP joint of the thumb, with the volar aspect of the base of the proximal phalanx in contact with the back of the head of the 1st metacarpal bone (Figure 2).
Initially, the maneuver described by Mc Laughlin6 was performed under local anesthesia, not achieving closed reduction. In operation room, under axillary block anesthesia closed reduction was not achieved, so an open reduction was performed, by palmar approach (Table 1).
|
Author year |
Number of cases |
Reduction C/O |
Immovization |
Results |
|
Dutton13 |
1 |
C → O dorsal |
Cast 12 days |
Asymptomatic, mobility and stability equal to contralateral |
|
Ishizuki25 |
26 (2 completas, 14 complicadas, 12 fractura de sesamoideos) |
C → O palmar. If dorsal inestability, PP reinsertion pull out technique |
Cast 4 weeks |
Minimal extension loss |
|
Patel5 |
9 acute 1 delayed |
C → 2 C → A palmar 8 |
K 4 weeks and/or cast 2-4 weeks |
|
|
Takami18 |
8 acute 1 delayed |
1→ O palmar (7 days) 8→C (less tan 4 days) |
Cast 1 week in C, 2 weeks in O |
Complete mobility and function |
|
Sodha19 |
4 |
C→ Percutaneous dorsal |
No mention |
complete mobility and function |
|
Hirata20 |
1 |
C + cast→ O palmar at 4 month surgery for Q for removal of |
Cast 3 weeks |
20o extension loss compared to contralateral (pre surgery). |
|
Ip4 |
1 |
C→ O: palmar + dorsal. PP suture to periosteum. |
Cast 3 weeks |
At 2-month follow-up, full range of motion was restored and pinch force was comparable to t uninjured hand. |
|
Izadpanah21 |
1 delayed, 2 month |
O, dorsal, |
Cast |
No mention |
|
Kim24 |
11 delayed (more than 6 month) |
O, palmar. PP minianchor suture |
Cast + K 4 weeks + 2 weeks cast |
It is the only one that describes how assessment is performed: modification of the classification system proposed by Glickel et al. + DASH and MHQ + Rx to assess degenerative changes. |
|
Baral22 |
3 pediatrics (1 incomplete, 1 complet, 1 complex) |
C incomplete y complete. O dorsal complex |
Cast 3 weeks |
No dolor ni inestabilidad residual |
|
Teo23 |
1 pediátrica |
C → O dorsal. Avulsion LCC (transosseous) |
Cast 4 weeks |
Stable MCP |
|
Total |
58 (13 delayed) |
1 percutaneous |
Cast 2- 4 weeks |
|
|
4 dorsal |
||||
|
4 palmar |
||||
|
1 dorsal + palmar |
Table 1 Number of cases with results
C, closed; →, impossible, changes to .., O, open; DASH, disabilities of the arm shoulder and hand; MHQ, michigan hand outcomes questionnaire; MCP, metacarpophalangeal joint
The collateral neurovascular bundles and the flexor pollicis longus tendon were medially displaced. The metacarpal head was found in an eyelet between the adductor pollicis and the flexor pollicis longus muscles. The palmar plate (PP) was avulsed from the metacarpal bone and interposed between both articular surfaces (Figure 3). Reduction was obtained by releasing the trapped PP; once achieved, anteroposterior and lateral joint stability was assessed. Given that he presented a notorious dorsal instability, PP was anchored with a pull out technique with nylon 2.0 and a dorsal button (Figure 4), thus restoring joint stability. The patient was placed into a thumb spica splint for 3 weeks and the pull out was maintained for 4 weeks.
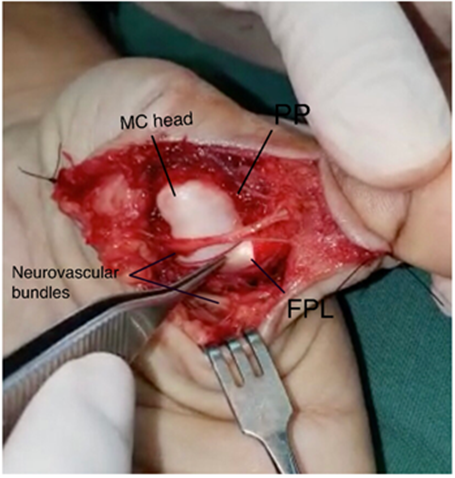
Figure 3 Intraoperative finding (MC: metacarpal; PP: palmar plate; FLP: flexor pollicis longus tendon).
There were no infectious complications or decubitus ulcer at the site of the dorsal button. After two postoperative months, the patient presented without pain or joint instability, with almost normal range of articular mobility.
The MCP joint of the thumb is a condylar joint with three degrees of freedom: flexion-extension, abduction-adduction, and a limited degree of rotation. These movements are limited by the periarticular soft tissues: side stability by the radial and ulnar collateral ligaments and the PP that prevents hyperextension.7–9
Dorsal dislocation generally occurs when there is a forced hyperextension trauma; the proximal phalanx moves dorsally to the metacarpal head, the PP detaches from its proximal insertion and is pulled into the joint. The metacarpal head generally passes between the tendons of the adductor pollicis and the flexor pollicis brevis muscles, and displaces the flexor pollicis longus medially or laterally. The collateral ligaments compress the palmar plate over the metacarpal head, which can remain interposed, preventing closed reduction.9–12 Collateral ligaments, palmar plate and joint capsule injury may be associated.
Irreducible dorsal dislocation of the MCP joint of the thumb is generally caused by interposition of the PP, but can be also due to interposition of sesamoids, flexor tendons and adductor muscle.13
Clinically, it presents as a thumb hyperextension deformity, metacarpal adduction and palpable metacarpal head in the palm. Confirmation is radiological, and must include standard anteroposterior and lateral approach. Radiograph allows diagnosis of the type of dislocation and evaluates the presence of fracture.14 It shows an enlarged joint space and frequently the presence of a sesamoid bone within the joint space.15
Farabeuf 16 classified the MCP displacements into three types. Incomplete dislocations with intact collateral ligaments; simple complete when the PP is not interposed between the displaced bones associated with rupture of collateral ligaments; and complex complete, those in which the PP is displaced and interposed within the joint space, which may require open reduction.
McLaughlin6 explained that for a successful closed reduction, the joint must be hyperextended, and the base of the proximal phalanx must be pushed over the head of the metacarpal and slowly brought into flexion. If not done correctly, a simple dislocation can turn into a complex one.
Eleven articles were analyzed including a total of 58 dislocations, in 13 of these diagnosis and treatment was delayed. In cases of acute dislocations, all the authors agree in trying closed reduction under local or regional anesthesia; if irreducible, they propose different options.
Sodha14 proposes a percutaneous reduction using a minimal dorsal incision with an 11 blade and longitudinal section of the PP. The rest of the authors performed open reduction, using volar and/or dorsal approaches. The volar approach presents a higher risk of neurovascular injury but allows direct access to the lesion, anatomical restoration of the joint and repair of the volar plate, decreasing the risk of late instability.17 With a dorsal approach the entrapped PP is easily identified, can be divided longitudinally, and reduced. It allows excellent visualization of the dorsally trapped PP and a better management of osteochondral fractures, with no risk of damage to the digital nerves or vessels. The main disadvantage is that it requires vertical division of the PP for reduction, which can decrease long-term joint stability; and it does not allow repair of the PP.
When articular stability is archived by closed reduction, early mobilization can be considered;6 otherwise, all articles agree on cast immobilization4,5,18–23 and / or K nails24 in 25 degrees of MCP flexion for 2-4 weeks. If the joint remains unstable after open reduction, surgical stabilization of the capsuloligamentous complex may be necessary.
If the PP of the thumb does not heal in proper position, prehensile function is lost and causes considerable functional impairment, which can progress to osteoarthritis.24 Chronic instability of PP with persistent symptoms despite nonsurgical treatment requires surgery. Several techniques have been described: capsulodesis, sesamoid arthrodesis, and repair of PP with removable sutures or sutures in situ, with local tissue or tendon grafts. Removable suture techniques (pull out)25 involve risks of infection and irritation of soft tissues; alternatively, anchors24 can be used. Results were evaluated in many different ways by the different authors, but in general good results were reported with almost complete range of joint mobility and adequate joint stability.
Dislocation of the metacarpophalangeal joint of the thumb is a relatively rare condition. Regarding treatment, all authors agree that closed reduction with the maneuver described by McLaughlin should be the first therapeutic gesture. When it is irreducible, the PP is the most common element interposed between the articular surfaces. There is no consensus with regard to the use of a dorsal or volar approach, nor in the management of periarticular soft tissues. After reduction, most authors immobilize the joint in 20 to 30 degrees of flexion for 2-4 weeks. Results are generally good, restoring a stable and painless joint, although there may be some degree of joint stiffness.
None.
The authors declare there are no conflicts of interest.
None.

©2021 Victoria, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.