MOJ
eISSN: 2471-139X


Case Report Volume 4 Issue 3
Pediatric Pulmonary Division, University of California, USA
Correspondence: James Brock, Pediatric Pulmonary Division, Miller Children's Hospital, University of California, Graduate Medical Education, Attention: Angel Arvizu, 2801 Atlantic Ave, Long Beach, CA 90806, Irvine, USA, Tel 5629338749, Fax 5629338744
Received: June 20, 2017 | Published: October 13, 2017
Citation: Brock J, Nussbaum E, Randhawa I. Pleuropulmonary blastoma, type 1r. MOJ Anat Physiol. 2017;4(3):315–317. DOI: 10.15406/mojap.2017.04.00138
A 5year old female admitted for pneumonia was found to have CXR concerning for right-sided congenital emphysematous lung lesion. She was initially treated with antimicrobials and pediatric pulmonology was consulted regarding abnormal CXR.
Physical examination revealed right chest diminished air exchange with increased anteroposterior diameter. Flexible fiber optic bronchoscopy demonstrated mucoid impaction of the right main stem bronchus causing ball-valve mechanism leading to air trapping with herniation of the right lung to left. There was also diffuse inflammation of her tracheobronchial tree, distal tracheobronchomalacia, and bronchomalacia of RML and RUL bronchi. Airway clearance was added. CTA revealed severe hyper expansion of the RML with multiple cysts that occupied the majority of her right hemithorax and left mediastinal shift. Lung V/Q scan showed minimal contribution by the right lung of only 11.3% with minimal perfusion.
Pediatric general surgery recommended outpatient surgical resection. Two months later she underwent right thoracoscopy, thoracotomy with RML resection and chest tube placement. Operative findings significant for multiple adhesions from the RML to pleura, grossly distended RML which was emphysematous throughout. The patient had resolution of the right pneumothorax within a week postoperatively.
Histopathologic diagnosis of the RML lobectomy and supplying bronchus resulted pleuropulmonary blastoma, regressed type 1r. Given the rarity of this lesion, the case and pathologic specimens were sent for review at the international pleuropulmonary blastoma registry in Minnesota, USA with diagnostic consensus.
Postoperatively, pleuropulmonary blastoma tissue diagnosis raised concern for DICER1 syndrome. Medical genetics recommended DICER1 testing which revealed no identified mutations.
Her care transferred to pediatric oncology. Abdominal and thyroid ultrasonography was negative for tumors, cysts or other abnormalities. The patient was safely discharged home following her postoperative recovery. At follow up CTA revealed no tumors and CXR normalized. Outpatient PFT demonstrated mild obstructive pulmonary defect with reversibility to bronchodilators but did not reveal restriction.
CXR, chest radiography; RUL, right upper lobe; RML, right middle lobe; CTA, CT with angiography; V/Q, ventilation-perfusion; RLL, right lower lobe; CPAM, congenital pulmonary airway malformation; PFT, pulmonary function testing; PIE, localized pulmonary interstitial emphysema; CDH, congenital diaphragmatic hernia
A previously healthy 5 year old female admitted to the Miller Children’s Hospital for right-sided pneumonia was found to have chest radiography (CXR) concerning for right-sided congenital emphysematous lung lesion [1-3]. Her presenting symptoms included shortness of breath with activity limitation and dyspnea with associated generalized abdominal pain. Her only significant past medical history included tonsilloadenoidectomy for obstructive sleep apnea. Her parents also reported a single emergency room visit at one year of age for wheezing, although she was not formally diagnosed with asthma or on controller therapy. She was initially treated with antimicrobials and pediatric pulmonology was consulted regarding her abnormal CXR (Figure 1-7).
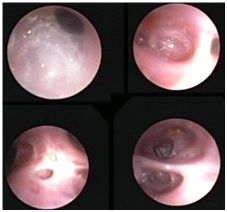
Figure 2 Diffuse inflammation of the tracheobronchial tree.
Flexible fiberoptic bronchoscopy with bronchoalveolar lavage: Mucoid impaction of the right main stem bronchus, causing ball-valve mechanism leading to air trapping with herniation of the right lung to the left. Mucoid impaction within right upper lobe bronchus, and right middle lobe bronchus. Tracheobronchomalacia, particularly with the posterior distal trachea, and bronchomalacia of the right middle lobe bronchus and right upper lobe bronchus.
Physical examination was notable for tachypnea with a maximal respiratory rate of 48 breaths per minute, tachycardia, pulse oximetry (SpO2) of 92%, diminished air exchange at right chest with asymmetric barrel chest (right > left) including increased anteroposterior diameter. Flexible fiberoptic bronchoscopy with bronchoalveolar lavage (FFB BAL) demonstrated mucoid impaction of the right mainstem bronchus causing ball-valve mechanism leading to air trapping with herniation of the right lung to the left. There was mucoid impaction within the right upper lobe (RUL) and right middle lobe (RML) bronchi, tracheobronchomalacia, particularly with the posterior distal trachea, and bronchomalacia of the right middle lobe bronchus and RUL bronchus. The mucosa of the tracheobronchial tree had diffuse inflammation. Airway clearance including beta-2 agonist were added to her inpatient treatment regimen, and further imaging obtained including chest CT with angiography (CTA) and ventilation-perfusion (V/Q) scan. The CTA revealed severe hyper expansion of the RML with multiple cysts that occupied the majority of her right hemithorax. The hyper expanded lobe was compressing atelectatic but otherwise normal appearing RUL and right lower lobe (RLL) parenchyma with severe mediastinal shift to the left. Lung V/Q scan showed minimal contribution by the right lung of only 11.3% with limited-to-no perfusion.
Pediatric general surgery was consulted and was in agreement with highest suspicion of our differential diagnosis of type I congenital pulmonary airway malformation (CPAM). Given the patient was symptomatic with her suspected CPAM, outpatient surgical resection was recommended (lobectomy versus segmental resection, while pneumonectomy is considered in patients with extensive multilobar involvement) following resolution of the acute illness present at initial hospitalization. The patient returned two months post-discharge and underwent right thoracoscopy, thoracotomy with right middle lobe resection with right-sided chest tube placement postoperatively. Operative findings were significant for multiple adhesions from the right middle lobe to the pleura, consistent with chronic inflammation or prior infection, grossly distended right middle lobe which was emphysematous throughout. The patient had resolution of the right pneumothorax within a week of the operation.
Histopathologic diagnosis of the RML lobectomy and supplying bronchus resulted pleuropulmonary blastoma, regressed type 1r. Given the rarity of this lesion (less than 400 cases identified), the entire case and pathologic specimens were sent and gained diagnostic agreement with the international pleuropulmonary blastoma registry in Minnesota, USA.
Postoperatively, the finding of pleuropulmonary blastoma raised concern for DICER1 syndrome, also known as Pleuropulmonary Blastoma Familial Predisposition syndrome. Medical genetics was consulted and the patient underwent DICER1 testing which revealed no identified mutations.
Pleuropulmonary blastoma is a de novo tumor most commonly arising in early childhood. With tissue diagnosis, the patient was transferred to the pediatric oncology service was who performed additional imaging to rule out neoplasms in other organ systems including renal and thyroid ultrasonography. No tumors, cysts or other abnormalities were identified and the patient was safely discharged home following her postoperative recovery.
At follow up, CTA has revealed no tumors and CXR has essentially normalized. Outpatient complete pulmonary function testing (PFT) has demonstrated mild obstructive pulmonary defect with air trapping and reversibility to bronchodilators with FVC 91 FEV1 73 FEF25-75% 44 (% predicted), with post bronchodilator FEV1 +17% and FEF25-75% +57% change. Body plethesmography did not reveal restriction SVC 93 TLC 118 RV 187 (% predicted) RV/TLC 171%. Diffusion capacity showed no alveolar diffusion deficit DLCO 97 VA 92.
Currently, she maintains stable lung function (FEV1 73% predicted) and is controlled with medium-dose inhaled corticosteroids twice daily.
Congenital lobar emphysema
None.
Author declares that there is no conflict of interest.

©2017 Brock, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.