Journal of
eISSN: 2475-5540


Research Article Volume 6 Issue 1
1European Wellness Centres International, Germany
2European Wellness Academy, Malaysia
3European Wellness Villa Medica Centre of Regenerative Medicine, Thailand
Correspondence: Dr. Dmytro Klokol, MD, PhD, European Wellness Centres International (EU, Asia-Pac), Klosterstrasse 205, Edenkoben, Germany
Received: January 22, 2020 | Published: January 28, 2020
Citation: Klokol D, Nallenthiran L, Nalapko Y, et al. Treatment strategies in management of chronic kidney disease from perspective of biological regenerative medicine. J Stem Cell Res Ther. 2020;6(1):1?9. DOI: 10.15406/jsrt.2020.06.00135
Chronic kidney disease (CKD) is characterized by a gradual loss of kidney function that happens over time and from the point of view of modern conventional medicine is considered to be an incurable and irreversible disease. The main risk factors attributing to CKR are diabetes mellitus, hypertension, glomerulonephritis, renal artery stenosis and family history of kidney disease. Affecting approximately 1 in 10 people of a Global population CKD imposes a significant threat to individuals’ lives and carries a major financial burden to patients and healthcare systems. CKD is the cause of at least 1 million deaths per year globally and consume nearly 6% of all medical expenses. In this article we discuss possibilities of disease control and reversal from the perspective of Biological Regenerative Medicine.
Keywords: chronic kidney disease, renal failure, biological regenerative medicine, stem cells, cell therapy, precursor cells, progenitor cells, tissue regeneration
“Kidney disease is a low-profile,
unglamorous problem, a disease
that disproportionately strikes minorities and the poor.”
Virginia Postrel
Well, let us face the fact – kidney disease is an insidious enemy that is out there ready to strike anyone should the opportunity arise. The kidneys serve as vital organs to filter out waste products from the blood and retain the important ones. These are carried out by the basic functional units of the kidneys called nephrons. Progressive loss of the number of functional nephrons leads to chronic kidney disease (CKD) and eventually end stage renal failure (ESRF), requiring renal replacement therapy. Numerous etiological factors have been attributed to the pathogenesis of CKD, leading the list would be the non-communicable diseases namely hypertension and diabetes mellitus. Other common causes include obstructive uropathies such as nephrolithiasis, glomerulopathies, autoimmune conditions such as lupus nephritis, renal vasculopathies mainly renal artery stenosis, polycystic kidney disease and recurrent pyelonephritis.1‒4
Renal embryology
The organogenesis of kidneys starts as early as fourth week of gestation, cranio-caudally with the formation of pronephros from the mesoderm, a non-functional vestigial structure from which the mesonephros is formed. The mesonephros is made up of primitive nephrons that are connected to the pair of mesonephric (Wolffian) ducts. Metanephros is formed when the ureteric bud, a localized outgrowth of the nephric duct, invades the metanephric mesenchyme, and undergoes morphogenesis to create a complex ductal network. The ureteric bud further develops into ureter, pelvis, calyces and collecting ducts while the pool of stem cells of the metanephric mesenchyme differentiates to form other renal structures, from collecting tubules to glomerulus. The metanephros develops fully by the 10th week of gestation while the whole kidney continues to develop till 32nd to 36th week of gestation (Figure 1).5‒8

Figure 1 Renal organogenesis: stages of kidney development through pronephros, mesonephros and metanephros.
Kidney injury and regeneration
The kidney is made up of different types of cells including glomerular podocytes, tubular epithelial cells, endothelial cells, pericytes, interstitial fibroblasts, dendritic cells etc. On average, an adult human kidney consists over thousands of nephrons, the functional units of kidneys. Given the natural history, various kidney cells exhibit different turnover period with an overall cell turnover significantly lower than that of other organs.10‒12
There are several adaptation mechanisms of the cells of the kidneys towards various insults. These include compensatory renal hypertrophy, cell proliferation, reprogramming of endogenous renal cells, renal progenitor cell differentiation, mesangial cell proliferation and migration, migration of bone-marrow cells into the kidney, and neoangiogenesis. Certain cells such as the mesenchymal cell possess the ability to differentiate into epithelial cells while some renal epithelial cells have the ability to differentiate to further proliferate, migrate and differentiate into the necessary type of cells. Bone-marrow-derived cells can migrate to the kidney, inhibit apoptosis and enhance renal cell proliferation. To a certain extent, renal progenitor cells have some potential to differentiate and promote kidney regeneration. However, by and large, by the 36th week of gestation, the universal renal progenitor stem cells pool is exhausted. This renders a dire situation of halted regeneration. This warrants an alternative pathway of replenishing the progenitors and enabling regeneration. Stem cell therapy is a promising avenue.13‒16
It is estimated that 1 in every 10 people suffer from CKD and this disease burden is expected to increase significantly, owing to the increasing rates of non-communicable diseases. An avowed “silent killer”, CKD is often gone unnoticed as early stages of this condition don’t exert much symptoms. Failing to halt the progression of the said diseases lead to end stage renal failure, some progressive and some sudden.1,4,17,18 The Global Burden of Diseases study done in 2015 summed that around 1.2 million people died from kidney failure. In 2010, an estimated 2.3–7.1 million people with ESRF died without access to chronic dialysis. Some geographic locations have even higher prevalence of CKD, reaching 11.9% in adults and 37.2% in elderly population.19 The CKD and particularly ESRF pose significant global economic burden with raising morbidity rates. The costs incurred in haemodialysis and related care is on rising trend, leaving aside the associated complications. That aside, renal transplant waiting list, donor rates and associated comorbidities are a different set of issues all together. It is estimated that 6% of total global medical expenses are being spent on CKD and related conditions.1,2,4
Despite the cutting edge medical discoveries at hand, it is devastating that the antidote for reversal of ESRF still stays at a dead end. It is important to mention that rigorous researches are being carried out to mark an end to this saddening situation which is yet to be fruitful.20‒26 One of the recent studies involving treatment and follow up of patients with hypertensive CKD has demonstrated that disease control is possible in less than 3% of the patients over the extended time period – a twelve year term.27 By any stretch of imagination such prognosis of the disease cannot and should not be considered to be even close to satisfactory. The urge for an antidote has pointed to a promising treatment modality, the stem cell therapy which has shown to revive the nephrons.9,23,24,28
Current status of therapeutic strategies for kidney regeneration
The medical frontiers have reached the necessity for an alternative treatment modality for CKD, stem cell therapy being a promising one. The cutting edge research targeting endogenous kidney regeneration has not produced effective outcomes. Hence, the current stem cell therapy employed in chronic kidney disease is of exogenous origin.
Types of stem cells used in CKD
While convincing clinical data and animal models with induced acute kidney injuries, either by ischemia or toxins, have exhibited intrinsic mechanisms of recovery enhanced by paracrine mechanisms of MSCs, repeated kidney injury and chronic damage to the nephrons exhausts all available intrinsic pathways as well as therapeutic modalities of kidney regeneration. Limited regenerative potential of the kidney and no existing medical treatment to reverse CKD warrants an alternative remedy to buffer the current dire disease burden. Stem cells used in current cell therapy to treat CKD are of various types and origin. These include bone-marrow-derived cells (BMDCs), embryonic stem (ES) cells, autologous adipose-derived mesenchymal stem cells (ADMSCs), induced pluripotent stem (iPS) cells and renal progenitor cells.10,15,18,23,24,28‒31 Adipose-derived mesenchymal stem cells (ADMSCs) have the capacity to differentiate into fat, bone, cartilage and muscle cells. These cells possess anti-inflammatory and immunomodulating functions and are easily accessible for harvesting and culturing in high volume. Unfortunately, these cells have not been proven to actively regenerate into renal cells, hence rendering it not beneficial in treating chronic kidney disease.32,33
The bone-marrow-derived mesenchymal stem cells (MSCs) have been the most widely used cell in the treatment of chronic kidney disease and end stage renal failure. The usage of this has been well established and has proven to yield results.34 The bone marrow contains two types of stem cell namely the hematopoietic and mesenchymal stem cells, accounting to about 0.01% of the marrow content. These cells may also be derived from fat tissue, amniotic fluid, umbilical cord, placenta. Records of scientific reports on the efficacy of MSCs in treating CKD or ESRF have been contentious.33‒36
Studies conducted in animals have proven that using the whole bone marrow yielded beneficial results, compared to BMDSCs which didn’t exhibit any positive effects. Some studies have shown that in comparative usage of mesenchymal and hematopoietic stem cells, only hematopoietic stem cells were found in the injured kidney cells. These hematopoietic cells were found to express markers in line with endothelial progenitors; hence they promote vascular and tubular regeneration, on a low scale though.37 BMDMSCs improve renal function via the anti-inflammatory effects of suppressing the cytokines namely IL-1β, TNF-α, and interferon-C and increasing immunosuppressive factor IL-10. It also promotes proximal tubular epithelial cells proliferation, reduce apoptosis and improve renal tissue oxygenation.33,35,38 The effects of MSCs’ in renal fibrosis have been debated. A particular animal study recorded the MSCs’ reno-protective property against fibrosis. However, this is largely due to protection from further insults rather than due to regeneration of the damaged renal parenchyma. Other studies failed to prove any beneficial clinical effect of MSCs. Though these studies may suggest varying effects of MSCs, collectively, MSCs have minimal nephrogenic differentiation potential.39,40
Embryonic stem cells (ESC) are the pluripotent stem cells derived from the inner cell mass of a blastocyst. These cells are capable to differentiate into any germ cell line: mesoderm, endoderm and ectoderm. Hence, in the past, these cells’ therapeutic potential was thought to be useful in regenerative therapy (Figure 2).
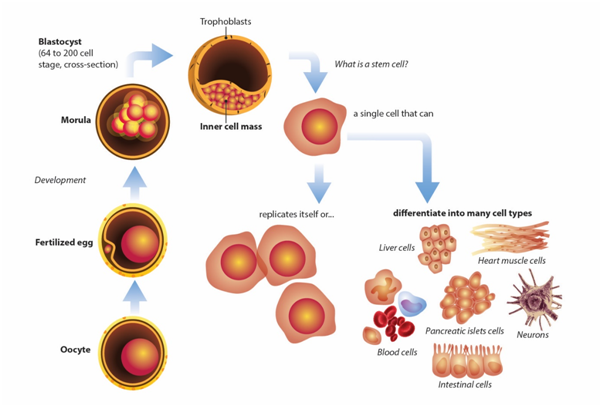
Figure 2 Stem cells and phases of cell differentiation: from totipotent stem cells to unipotent and differentiated cells.
A number of experiments have established that ES cells can differentiate into renal epithelial cells and once introduced directly into developing metanephros can differentiate to tubular epithelia with nearly absolute efficiency. Unfortunately, studies have also confirmed that this can also give rise to spontaneous teratomas as ES may differentiate into all three types of germ lines. There are still many uncertainties regarding the usage of ES in regenerative medicine. Studies have shown that the development of teratoma depends on the site of implantation. It also largely depends on the host immune status, another down fall. According to the study by Yamamoto et al., ES cells can develop a teratoma 14 days and 28 days after transplantation into mice.41 Attempts have been made to prevent teratoma formation in the usage of ES in regenerative medicine. One such potential way is by eliminating undifferentiated cells by selectively removing them based on their well-defined cell-surface marker profile (SSEA-4+, Tra1-60+ and Tra1-81+) using a combination of antibodies.41,42
Takahashi and Yamanaka, in 2006, discovered a new avenue in the field of cell transdifferentiation by using Induced pluripotent stem cells (iPSCs) in kidney regeneration. This was initially done by genetically reprogramming fibroblast into pluripotent stem cells by combined overexpression of four specific transcription factors – Oct-4, Sox2, Klf4 and c-Myc – introduced via retroviral delivery. These studies generated pluripotent stem cells from adult mouse liver, stomach cells and renal cells. Despite the discovery, IPSCs do have shortcomings as follows:
Management of CKD with xenogenic stem cell transplants
When stem cells are harvested from one species and used to treat a subject of a different species it is called xenogenic stem cell therapy. The major upper hand of this type of stem cell is the easy availability of organ-specific precursor cells. These stem cells, though having lost the pluripotency and totipotency still exhibit the multi and oligopotency that can differentiate into different types of cells that of same germ line.44‒47 In xenogenic cell therapy, the organs of animal foetuses in their last trimester are used. Previous studies show the usage of various species of animal in treatment of a wide range of degenerative disorders.46 For instance, in Japan the porcine-derived cells are used to treat type 1 diabetes mellitus.48 There is multiple data on use of xenogeneic cell therapy in neurodegenerative diseases and many other.49 Sheep and rabbits, however, are preferred source of xenogenic cell therapy materials, owing it to the resistance of these animals to certain diseases and culturally and religiously more widely acceptable. The Specific Pathogen Free colonies of these animals catering for the research institutions and pharmacological industry are also available.50
The animals used in xenogenic stem cell harvest are bred over 30 generations and monitored in a closed colony to ensure free from pathogens. The ambience of closed colony is established based on standard protocol. Continuous monitoring and regular surveillance is carried out. The process of procurement, preparation and manufacturing, storage and transportation is done in optimised temperature, aseptic ambience, efficiently and as quickly as possible to ensure a high quality yield.46,50 The implanted live precursor cells reach the target site via the homing effect and elicit the therapeutic effects via harnessing the existing resident stem cells, arresting inflammation and apoptosis and promoting repair through induction certain cellular factors (Figure 3).

Figure 3 Principles and mechanisms of live precursor cell therapy are based on the “homing effect” and paracrine effect. The paracrine effect promotes reprogramming, regeneration and differentiation of the kidney.
Some cells have been shown to be taken up phagocytes and active cellular substances are released. These cells promote growth and healing by paracrine interaction with resident cells, through the release of growth and anti-inflammatory factors, cytokines, prostaglandins, exosomes, vascular endothelial growth factor, insulin-like growth factor and other related mediators (Figure 4). Similar mechanism explains the clinical efficacy of organ specific cellular extracts, at a lower scale though, compared to precursor cell therapy. The usage of organ specific cellular extracts has been successfully employed in Europe almost a century long. Among the salient advantages of xenogenic fetal precursor stem cells is the array of cell types and the amount of cells available to be harvested for implantation.
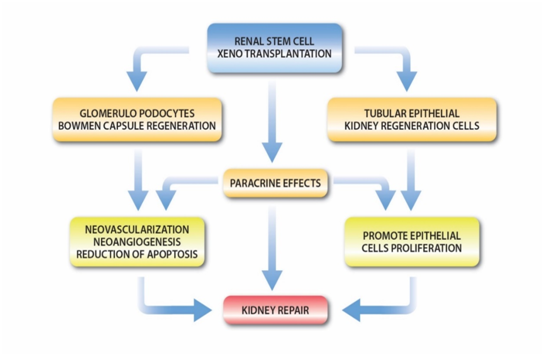
Figure 4 Pathways of kidney regeneration after precursor cell implantation. The kidney regenerates through tubular epithelial cells and glomerular podocyte regeneration, as well as via paracrine effects.
In employing fetal precursor stem cells in treating the CKD, it has been discovered that glomerular defects respond well to the core treatment component being kidney precursor cells. Precursor cells from other organs such as the adrenal cortex, mesenchyme, vascular endothelium and placenta should be used as it will facilitate a better therapeutic outcome. These cells provide a wide range of growth factors and cytokines stimulating the paracrine reactions in repairing the kidney, rendering a better clinical response.48,49
The combination of precursor cells used in treating kidney diseases depends on each patient. It is individualised and custom made. For instance, patients with pre-existing autoimmune conditions should be given precursor cells from thymus or spleen while in patients with diabetes mellitus, the diabetic treatment protocol should be added. There has been no major adverse effects or drug interaction reported in employing precursor cell therapy concurrently with other drugs or treatment modalities. However, it is advisable to withhold the administration of any other drugs within 48–72 hours before and after implantation, for optimal response. Generally, reactions to implantations depend upon each individual and are usually well tolerated. However transient low grade fever and fatigue has been reported. Post therapy, patients are generally advised to rest for few days, avoid physical exercise and certain activities like sunbathing, saunas, spas and heavy outdoor activities. Alcohol consumption and smoking should be ceased. Any vaccination should be withheld for a month. Certain conditions render it unsuitable for the therapy. Among which include recent or current infection, vaccination within one month prior to implantation, acute medical conditions such as myocardial infarction, stroke and other medical emergencies, regular consumption of cytostatic medications or current administration of chemotherapeutic agents, radiotherapy and incurable terminal conditions.51,52
Multimodal approach to treatment of CKD in Biological Regenerative Medicine
Another crucial point for the scenario of successful CKD treatment is an engagement of multimodal approach, which includes pathogenetically substantiated therapeutic modalities targeting cellular mechanisms of longevity, repair and improving renal tissue metabolism. Let us further discuss some aspects of bioregenerative treatment protocols essential for the improvement of renal function.
The interventions targeting the delay of CKD progression include nutritional support, lifestyle modification, and medical management to control blood pressure and glucose and reduce albuminuria.54,55 Albeit the off-label use in management of CKD, N-acetylcysteine (NAC), which is a direct scavenger of free radicals that can improve blood flow through nitric oxide-mediated vasodilation; it is also a precursor for glutathione synthesis. Antioxidant and vasodilatory properties of NAC provide protection against contrast-induced and obstructive nephropathy.56,57 Although exact mechanisms by which NAC reduces risk of ESRF in CKD patients still remain unclear, according to the data of Liao et all, NAC use is associated with 18% reduction of progression of CKD.53
Another possible pathway of decelerating the progression of CKD may be via the elimination of senescent cells, which acquire pro-inflammatory and senescence-associated secretory phenotype. It is known that senolytic drugs, i.e. Quercetin and Dasatinib, specifically target senescent cells by inducing apoptosis of senescent but not non-senescent cells.58 In our practice we selectively and cautiously use Quercetin for CKD patients with the background of metabolic syndrome due to lack of the evidence and clinical data. L-arginine is an essential amino acid that serves as a substrate for the synthesis of nitric oxide (NO), polyamines, and agmatine and influences hormonal release and the synthesis of pyrimidine bases. L-arginine is the main source for the generation of NO via NO synthase, which have been found to be expressed in the kidney.59 In the kidney the endothelial NO synthase is important in the maintenance of glomerular filtration rate, regional vascular tone, and renal blood flow.60 L-arginine is also the substrate for arginases, increased activity of which has been associated with tissue repair and cell growth and may play an important role in renal disease.59‒61 Although L-arginine increases plasma levels of NO and its metabolites, it alone has failed to significantly improve glomerular function. However, when used in combination with other therapeutic tools it may bring certain benefits to CKD patients and ameliorate kidney injury.
L-Carnitine is critical for the transportation of long-chain fatty acids across the inner mitochondrial membrane for subsequent oxidation and energy production. It has been known for many years that patients with ESRF suffer from progressive L-carnitine deficiency, often due to its loss via hemodialysis. Abnormalities in carnitine homeostasis may have profound biochemical effects on serum lipid, red blood cells, cardiac muscle, and skeletal muscle.62,63 In 2003, the USA National Kidney Foundation developed a practice recommendation for the use of L-carnitine in dialysis-related carnitine disorders, most notably erythropoietin-resistant anemia, intradialytic hypotension, cardiomyopathy, and fatigability.64 In our opinion the early inclusion of L-cartinine supplementation in moderate stage of CKD may be beneficial in terms of prevention of development of the profound physiological and biochemical changes associated with renal failure.
The evaluation and tabulation of the outcome of the therapy is a Hercules task. Individualised treatment approach and the cost involved make it difficult to standardise the treatment protocol and prescriptions, however does not mean it is not attempted. Patients undergo holistic treatment according to the concepts and paradigms of the Biological Regenerative Medicine. Patients’ logistics, geographical distribution, contact duration and frequency with the primary physician or the medical institutions they are attached to makes it more cumbersome to evaluate and compare the outcomes.
The clinical data used in this open uncontrolled study was obtained both retrospectively and prospectively. In the previous cohort study we have analysed the results of 23 CKD patients’ treatment using cell therapy.47 Only the patients with CKD stage 3a and 3b were included into the previous study. For the current study we have broadened the inclusion criteria and admitted patient with CKD stage 4. This paper also presents a case study of a patient with ESRF, on regular haemodialysis, who had a great positive response to our treatment.
The current study includes data analysis of 34 patients with CKD stages 3a, 3b and 4 treated for the past 15 years. The study was multi-centric, multi-national, with vast variability of patients in terms of their ethnicity, age and co-morbids. The stage of renal failure was determined according to GFR values by standard commonly-accepted methods.65,66
The entire cohort of 39 patients consisted of 16 patients with CKD stage 3a (GFR ranged 45-59 ml/min/1.73m2); 12 patients with CKD 3b stage (GFR ranged 30-44 ml/min/1.73m2); 11 patients with CKD stage 4 (GFR ranged 15-29 ml/min/1.73m2). The group of CKD stage 3a had 10 males and 6 females, in the age between 39-65 years (mean age 45); group of patients with CKD stage 3b had 8 males and 4 females, age between 37 to 65 years old (mean age 56); group of CKD stage 4 had 8 male patients and 3 females, age between 54 to 67 years (mean age 63).
Prior to implantation all patients signed an informed consent and went through a thorough clinical and biochemical examination to find possible contra-indications to procedure and to document the base-line health profile. The general treatment protocol included such standard regenerative medicine tools as prescription of resveratrol, metformin, senolytic drugs, as well as supplementation with lecithin, L-carnitine, L-arginine and NAC. The treatment protocols were individually adjusted in each case according to the etiology and pathogenesis of the disease. The hallmark of the treatment was organ specific cell therapy with renal precursor/progenitor cells: progenitor glomerular podocytes and progenitor tubular epithelial cells. Apart from renal precursor cells the holistic longevity treatment cell therapy protocol that was given to observed patients included precursors of hepatocytes, islets of pancreas, mesenchymal cell, vascular endothelial cells, cardiac myocytes, neuronal cells, cells of adrenal cortex, gonads. Cell therapy prescriptions were individually prepared for each case according to the standard protocols of cellular materials’ handling.46,50‒52 In continuation to cell therapy after precursor cell implantation patients received organ specific kidney peptides/cell extracts (MitoOrganelles, MF+™). The outcomes of the therapy were evaluated 6, 12 and 18 months post treatment.
Obtained results
Upon enrolment to the study the baseline mean GFR level in male patients with CKD 3a stage was 54 ml/min/1.73m2; in female patients - 44 ml/min/1.732/m2. In the CKD stage 3b group the mean GFR level in male patients was 38 ml/min/1.73m2 and in female patients –37 ml/min/1.73m2. In the group of patients with CKD stage 4 male subjects had mean GFR was 25 ml/min/1.73m2, and in female patients – 23 ml/min/1.73m2. According to our observations nearly all patients experience a progressive shift in their well-being essentially from the beginning of their Biological Regenerative Medicine treatment protocol. The progress mainly consisted in greater physical performance and cognitive function, reduction of fatigue, enhanced ability to recover after exercise, and improved sexual performance and quality of sleep. Patients with metabolic syndrome and diabetes type 2 are usually responding well by normalizing the blood pressure, reduction of visceral and subcutaneous abdominal fat, and better parameters of glycaemic control and blood lipids profile. During the entire observation period majority of patients have demonstrated clinical improvements of a different degree with regards to their underlying medical conditions. Even those patients who did not gain significant improvements in their kidney function had experienced notable progress in the performance status, state of well-being and achieved positive dynamics in terms of diabetes, metabolic syndrome, serum lipids and hormonal profiles.
As a result of the treatment within 6 months in the group of patients with CKD stage 3a mean GFR level has improved from 54 ml/min/1.73m2 to 69 ml/min/1.73m2 in male subjects and from 44 ml/min/1.73m2 to 61 ml/min/1.73m2 in female subjects. Patients continued to receive cycles of maintenance treatment with essential supplements mentioned above and kidney cell extracts (Mito Organelles, MF+™). Such approach enabled us to maintain steady results and preserve achieved mean GFR levels in the group within the same range until the end of the trial period (chart 1). Downstaging of CKD in the group of patients with CKD stage 3a took place in 12 patient out of 16 – 75%.
Mean GFR level in a group of patients with CKD stage 3b had improved from 38 ml/min/1.73m2 to 55 ml/min/1.73m2 in male patients and from 37 ml/min/1.73m2 to 48 ml/min/1.73m2 in females. During the subsequent 12 months of follow up and treatment mean GFR did not deteriorate much from the achieved levels (chart 1). Overall dowstaging rate in patients with CKD 3b was 7 out of 12 subjects – 58.3%.
In the group of patients with CKD 4 downstaging to stage 3a-3b was achieved in 6 patients out of 11 (54.5%). Mean GFR level in this group increased from 23-25 ml/min/1.73m2 to 39 ml/min/1.73m2 in both males and females (see chart 1).
CKD stage 5 case presentation
To this date reversal of ESRF was an extremely challenging if not to say impossible task. In the November 2018 we had a pleasant 68-year old gentleman presented to us. The history of his disease had a series of unfortunate events starting from acute cardiac event, coronary stenting with various complications resulted in open heart surgery and heart valve replacement ending with ESRF. Upon presentation patient was 8 months on regular haemodialysis three times per week. Baseline GFR level was 9 ml/min/1.73m2.
The treatment protocol consisted of precursor/progenitor stem cells, frozen organ specific cells (xenogeneics), MitoOrganelles™ specific to kidney and heart (twice weekly for 4 months), NAC and other essential components described above.
Within two months after treatment protocol was initiated we observed increase of the GFR. By the third month patient’s GFR increased to a level sufficient for the patient to be removed from regular haemodialysis (chart 2).
The long term follow up of this patient has shown stable renal function for more than a year without further tendency to reduce. On the same note, Regenerative Medicine protocols using xenogeneics has proven remarkable efficacy when used properly according to strictly defined indications and contraindications. We haven’t observed any significant adverse reaction or complications after cell therapy.
Adult kidney consists of almost one million nephrons - the functional units of kidney. Chronic kidney disease is associated with injury of different cell types including glomerular podocytes, tubular epithelial cells, mesangial cells, or endothelial cells. According to the current understanding of this pathology, there are four key processes of kidney regeneration, including reprogramming of endogenous renal cell, migration of MSCs from bone marrow and macrophage into kidney, renal progenitor cell differentiation, and neoangiogenesis. Although in theory there are some similarities between renal regeneration and renal development through cell dedifferentiation, in reality human kidney is lacking of intrinsic regenerative potential.
During the fetal stage of development, condensed mesenchyme around the tips of the branching ureteric bud contains self-renewing cells capable of generating all other elements of the nephrons, interstitium, and vasculature. The cells of condensed mesenchyme are regarded as the renal stem cell population. Formation of new nephron in humans is complete by 36th week of gestation, while it continues for 1-2 weeks after birth in rodents and some other mammals. The fact that renal stem cells are exhausted prior to the perinatal stage suggests that complete regeneration involving a complete replacement of the nephron lost does not occur in human kidney.
Renal progenitor cells are the lineage-restricted type of cells, which have limited differentiation and self-renewal potential.67 Renal progenitors are identified by cell marker CD133 and CD24. CD133 is a marker of several types of adult tissue stem cells. CD24 is a surface molecule that is expressed in human metanephric mesenchyme. In the adult mammalian nephron, renal progenitor cells gather at the urinary pole and disperse over the Bowman capsule, the proximal tubule, the thick ascending limb and the distal convoluted tubule at the point of connection with the ureter. Renal progenitor cells at the urinary pole can differentiate into glomerular as well as tubular epithelial cells. Tubular progenitor cells represent 2-6% of all tubular epithelial cells in healthy adult kidneys and express CD133 and CD24, as well vimentin, cytokeratin 7 and 19, Pax2, and nestin that are not expressed by differentiated tubular epithelial cells. Glomerular progenitor cells localize within the Bowman capsule and can differentiate toward the podocyte phenotype. Tubular progenitor cells cannot express CD106, whereas glomerular progenitor cells can express this surface marker.68
Renal progenitor cells have higher resistance to injury in comparison to all other differentiated cells of the kidney. When injected in severe combined immunodeficient mice affected by rhabdomyolysis-induced AKI, both of these populations displayed the capacity to integrate into the tubules, generate novel tubular epithelial cells, and improve renal function.69
Because stem cells cannot be manipulated easily to differentiate to desired renal cells, less potency but reliable differentiation process makes renal progenitor cells more applicable in kidney regeneration medicine. Compared to stem cells, renal progenitor cells have advantages, such as that knowledge of intermediate cell culture conditions is not required and renal progenitor cells can transit directly from one phenotype into another.68
In another experimental study 6 and 10 weeks after fetal kidney precursor cell transplantation, the transplants showed the reconstitution of tubular and glomerular structures in the reconstituted regions of the remnant recipient kidneys. The newly formed glomeruli were structurally similar to normal glomeruli after 6 weeks (Figure 5).
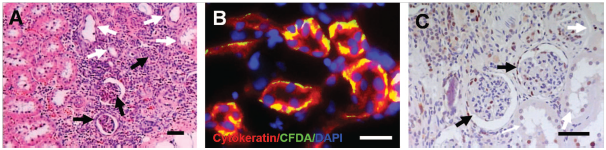
Figure 5 Histological micrographs of transplants retrieved 6 weeks after transplantation. (A) Regenerated glomeruli (solid arrow) and tubules (open arrow) were observed in the fetal kidney precursor cell transplantation group. (B) Fluorescently labelled kidney precursor cells (green fluorescence) were detected in the reconstituted kidney tubules (red fluorescence). (C) Immunostaining for PCNA showed the presence of actively proliferating cells in the reconstituting glomeruli and tubules of the cell transplantation group.68
The labelled progenitor cells were detected in the glomerulus at 10 weeks after transplantation (Figure 6). Immunohistochemical analyses using antibodies against PCNA indicated intensive proliferating activity in the transplanted fetal kidney precursor cells in the reconstituted regions of the transplants. Transplantation of fetal kidney precursor cells attenuated the progression of glomerulosclerosis. The average glomeruli number per unit area in the remaining kidney was highest in the fetal kidney precursor cell transplantation group.
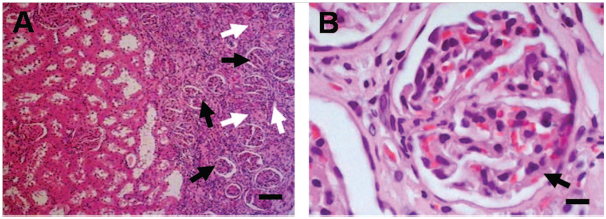
Figure 6 Histological micrographs of transplants retrieved 10 weeks after transplantation. (A, B) Regenerated glomeruli (solid arrow) and tubules (open arrow) were observed in the fetal kidney precursor cell transplantation group.68
Available experimental and clinical data obtained from the current study and other available resources provide evidence that fetal precursor stem cells are arguably the safest and most effective method of kidney regeneration. Fetal precursor cell xenotransplantation allows slowing down and even reversing the stage of chronic renal failure stage in a large number of CKD patients. The provided treatment has also demonstrated a good stability of outcomes, as within more than a year there were no adverse reactions noted and achieved progress in improvement of renal function was preserved for at least 18 months of follow up.
As this study has clearly shown the downstaging of CKD stage 3a is possible in 75% of cases, downstaging of CKD 3b may be achieved in 58.3%. As for the CKD stage 4, the current study demonstrated an astounding 54.5% rate of downstaging. However, in reality this rate is expected to be less due to the fact that we did a very meticulous selection of patients – candidates for bioregenerative therapies.
Complexity of the kidney’s structure makes its regeneration an extremely challenging task. Further studies are necessary to enhance the therapeutic efficacy of this approach. To better understand how fetal kidney precursor cell transplantation exerts its beneficial effects, further studies concerning markers for kidney stem/progenitor cells and the characterization of the cell population in the fetal kidney precursor cells are required. One of the further research directions is to find out whether the kidney regeneration is possible with only renal precursor cells or with combination of renal precursor cells and other stem cells, for instance MSCs. Apart from this, the entire kidney regeneration protocols of Biological Regenerative Medicine requires optimization in terms of establishing exact protocols of number of transplanted cells and administering of specific growth factors and kidney-specific cell extracts, which may support structural and functional renal reconstitution.
Authors declare no conflict of interests either commercial benefit from publication of these materials.

©2020 Klokol, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.