Journal of
eISSN: 2475-5540


Short Communication Volume 1 Issue 7
1Department of Biochemistry, Acharya Nagarjuna University, India
2Centre for Cellular and Molecular Biology, India
Correspondence: Rajeswari Jinka, Assistant professor, Department of Biochemistry, Acharya Nagarjuna University, Guntur-522 510, India
Received: November 17, 2016 | Published: December 30, 2016
Citation: Jinka R, Raj A, Gunda S, et al. Inherent properties of extracellular vesicles collected from re-differentiated cancer stem cells. J Stem Cell Res Ther. 2016;1(7):276-279. DOI: 10.15406/jsrt.2016.01.00048
The focus on Stem cells provides a considerable attention in translational medicine for their potential capacity in terms of tissue regeneration, repair and as drug delivery. Recent evidences showed that stem cells secrete small vesicles into the extracellular milieu, known as extracellular vesicles (EVs). They are known to carry a repertoire of mRNAs, miRNAs, DNA, proteins, and lipids that can be transferred to neighboring cells, modifying their phenotype as well as the microenvironment. Stem cell-Extracellular vesicles may provide the opportunity to overcome the hurdles or complications raised in stem cell therapeutic strategies. Our data showed that the extracellular vesicles secreted by the spheroids, constituted by the stem cells obtained by the dedifferentiation process are positive for CD133 and negative for the multi-drug resistance and tumorigenecity.
Keywords: non adherent cells, spheroids, cancer stem cells, phagosomes, metastasis
Cancer as defined is initiated by inconsistent changes occur in normal cells by altering the cell adhesion, several signaling mechanisms; accumulation of genetic and epigenetic changes consecutively enhances the cellular growth. Several changes have been reported earlier which constitute the in situ changes in the microenvironment as well as cellular phenomenon. Cellular transformation is ignited in adult stem/progenitor cells during oxidative stress, intense injury, inflammation and ageing may lead to genetic and epigenetic alterations and are designated as cancer-initiating cells. These cells in due course of time gain all the hall mark properties such as sustained proliferative signaling, evasion of growth suppressors, resistance to cell death, replicative immortality, copious angiogenesis, active invasion and metastasis in generating the bulk mass of heterogeneous and differentiated cancer cells within tumour. These cells are often referred to as Cancer stem cells (CSC).1 These cells are attributed to be a sub set of cells in the heterogeneous population of tumors. Cancer stem cells like cells are rare in cancer, but play an important role in maintenance of cancer homeostasis. Hypothetically, CSCs are not only the source of the tumor itself but form the basis for tumor progression, metastasis, resistance to therapy, and subsequent tumor recurrence.1,2 Isolation of cancer stem cells is critical; however, the existence of cell surface markers such as CD133, ALDH1 and CD44 could be beneficial in the isolation process. It is shown colorectal CSCs were isolated based on the existence of CD133 marker and showed that the CD133+ subpopulation could form xenograft tumors.3,4
Recently it is proposed that the stem cells secrete small vesicles in the form of extracellular vesicles (EVs) in to extracellular milieu. EVs are submicron particles, derived directly from pinching of plasma membrane and carry a repertoire of parental mRNAs, miRNAs, DNA, proteins and lipids and can be transferred between cells via EVs.5 Emerging evidences reveal that functional aspects of stem cells i.e., such as self differentiation, maturation, self renewal could be mimicked by the stem cell associated EVs.6,7 However, isolation of EVs from the early transformed cells is not yet studied. In this study we report the secretion of EVs from the embryonic bodies obtained by re-differentiated cancer stem like cells.
All experiments were performed by using a normal rat (Fischer strain) fibroblast cell line, F111, the origin of which has been described earlier.3 F111 cells were maintained in Dulbecco’s Modified Eagle’s medium (DMEM) supplemented with 10% Fetal Calf Serum (FCS), penicillin (100 U/ml) and streptomycin (50 mg/ml) and were used within five passages after revival from cryo-preservation.
Preparation of extracellular vesicular bodies from the spheroids and their execution in nude mice
Preparation and collection of Adherent (A) and non-adherent (NA) cells from F111 cells is described earlier by Jinka et al.2 After collecting the Non-adherent cells at 16 hours time point (NA16) from the agarose coated surface, 5ml of complete medium was added to the few cells that were remained on top of the agarose layer and were further incubated at 37°C in presence of 5% CO2 by monitoring the cells continuously for 7-10days till the formation of spheroids. The spheroids formed were collected by mild centrifugation and were disturbed mildly with the help of 26 Gauss needle and were kept undisturbed for a period of 72 hours in a CO2 incubator in a six well plate. After 72 hours the vesicles shed by the stem cells were collected by centrifugation at 10,000rpm for 10-15 minutes at 4°C temperature and the cell free vesicles collected in PBS were injected subcutaneously in to a 4-6 week old, homozygous nude mice (NIH strain, Nu/Nu). All experimental procedures were approved by the Institutional Animal Ethical Committee (IAEC 132/2007 dated May 19th 2008).
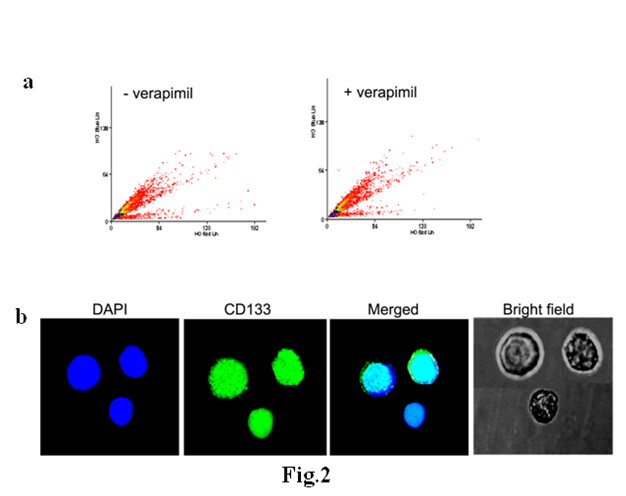
Side population (SP) cell analysis
The extracellular vesicles were incubated with 2.5μg/mL Hoechst 33342 (Sigma) for 90 minutes at 37°C and were collected after centrifugation at 10000rpm in a refrigerated centrifuge and washed once in HBSS (Hank’s balanced salt solution) and re-suspended in ice-cold HBSS, Propidium iodide (50μg/ml) was added just before analyzing the vesicles on a MoFlo cell sorter (Dako Cytomation Glostrup, Denmark). Inhibitory action on the Hoechst efflux was checked with 50mM Verapamil.
Immunoflourescence
Single vesicular suspensions were fixed in 70% ethanol followed by careful washes with PBS. Mild cell permeabilization was done with 0.1% triton-X 100 and were stained for CD-133 (Purchased from Abcam) incubating cells at 4°C for 1hr with corresponding primary antibodies (1:100) and the experiment is done as was done earlier for non adherent cells. After washing, the vesicles were treated with appropriate fluorescent labeled secondary Ig antibodies. Stained cells were observed under a Leica Confocal microscope with a 63X, Plan Apo objective.
Previous results implicate that the normal adherent rat fibroblast cells are undergoing transformation upon suspension and there by inducing tumors in in vivo and form colonies in in vitro conditions. An attempt is made to study the fate of non adherent cells that were remained on the surface of agarose coated surface after collecting the cells at 16hours time point. These cells were cultured further in complete DMEM medium for another 7-10 days till the formation of spheroids.
The cells on agarose coated surface remain round and only a few cells were seen on the surface as shown in Figure 1A. The earlier report showed that the activation of hypoxia inducible factor 1 (Hif-1), a transcriptional factor could function as a key regulator under stress conditions of non adhesion where the transformation is induced by up regulation of all the hall mark properties of cancer.2 We observed the formation of a tube like structure generated in the suspension (Figures 1B & 1C), probably with the aid of dissolution of cells by the process of autolysis. During unavoidable conditions and for the survival benefits of the leftover non adherent cells, the autophagic process starts with the elongation and probably by merging the cellular membrane in the formation of a double membrane vesicle (autophagosome), which engulfs bulk cytosolic material and targeted cellular organelles that come across. The lumen of phagosome activates hydrolytic enzymes that degrade the content of the autolysosome, giving rise to amino acids, fatty acids, nucleosides and other metabolites released into the cytosol and recycled in anabolic cellular metabolism as described by.8 It is also observed that the remaining suspended cells, which are already in transformed state, could adhere to this double membrane phagosome and further aggregates in the formation of spheroids (Figures 1D & 1E). The results were compared with spheroids of human colon cancer cells, HT29, Caco2, and SW480 cells cultured in a suspensions.9 By disrupting the embryonic bodies, we observed that a few cells detached from the embryonic bodies could adhere superficially and gently to the plastic and are found to be round with less cytoplasmic and higher nuclear space, which could be recognized as cancer stem cells (Figure 1F), based on the previous observations of increasing in stemness of the non adherent cells3 at the 16 hour time point of the suspension. Induced autophagy at the later time points may also play a key role in modulating the stemness of the dedifferentiated cells similar to that of mesenchymal stem cells (MSC) of bone marrow.10

Further, we observed the appearance of small vesicles which were represented as shedding of stem cells. Earlier observation showed that the non adherent cells are de differentiated by attributing the properties of side population, one of the assets to the stem cells. In this context when observed for the characteristics of stem cells. Side population analysis showed that the vesicles are smaller in size pertaining DNA as they were stained with Hoechest dye but were not inhibited with varapimil (Figure 2A). Indicating that they do not belong to the side population cells, though the parental non-adherent cells persists the higher multidrug resistance (MDR) activity when compared to that of adherent cells.3 It was clearly showed that these vesicles possess CD 133 expression (Figure 2B) as they were stained for CD133 antibodies. Emerging evidence reveals that secreted vesicles from stem cells could mimic a spectrum of stem like phenotype by trafficking stem cell associated transcription factors such as Nanog, Oct-4, HoxB4, and Rex-1 operating at the level of pluripotent stem cells and CD105, prominin-1/CD133 and KIT as MSC markers.11
In several studies it is showed that EVs carry biological messages from parent cells that interact with recipient cells and there by influence their normal physiology and there by their overall fate.12 Extra cellular vesicles, when injected in to nude mice no tumor formation was observed and animal was very active for the entire period of control cells (NA16 cells) sustaining as tumors in nude mice. The results indicate that the vesicles collected in this way from spheroids are homogeneous and require the tumor microenvironment to sustain as a tumor in nude mice. In contradiction to this, the vesicles were injected in to healthy nude mice, where the microenvironment is normal and also injected vesicles may be providing protection against cancer due to presence of a prominent pluripotent marker, CD133. This indicates that the microenvironment with a minimum heterogeneous population of cancer may be required for the communication of the vesicles shed from spheroid bodies of non adherent cells to grow in the form of tumor as observed for NA16 cells. EV communication with the microenvironment is also observed for cancer stem cells in the process of tumorigenecity and heterogenecity.13,14
In the current study, the steps involved in the formation of extracellular vesicles are critical and can be attributed for liable applications in normal and diseased conditions. Recent evidences reiterate that EVs play a central role in paracrine response that therapeutic cells elicit in diseased or damaged tissues. Cell free EVs of MSC, dendritic cells, cardiospheres and neural stem cells are found to be potential and alternative source for stem cell derivative therapeutics.15 The methodology adopted in the current study is cost effective and efficient in the production of non tumourigenic and homogeneous EVs from the re differentiated cancer stem cells. Further study is required for its therapeutic applications in the suppression of cancer growth.
This work was supported by a DST grant, under SERC, Fast Track Scheme (No. SR/FT/L-07/2005), Government of India.
The author declares no conflict of interest.

©2016 Jinka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.