Journal of
eISSN: 2373-4426


Case Report Volume 1 Issue 7
Department of Paediatric Surgery, TNMC & BYL Nair Hospital, India
Correspondence: Hemanshi Shah, Professor and H.O.D, Dept of Paediatric Surgery, TNMC and BYL Nair Hospital, Mumbai 400008, Maharashtra
Received: September 10, 2014 | Published: December 10, 2014
Citation: Tiwari C, Sandlas G, Jayaswal S, Shah H (2014) Unique Presentation of Hydrocolpos as a Perineal Hernia in an Infant with Cloaca. J Pediatr Neonatal Care 1(7): 00049. DOI: 10.15406/jpnc.2014.01.00049
Perineal hernias are very rare and more so in the paediatric age group. We report a case of perineal hernia in an infant with cloaca. The patient presented as a gluteal mass with the hydrocolpos presenting as a perineal hernia because of the congenital hypoplastic and grossly deficient pelvic muscles. The pre-existing literature on perineal hernia has also been reviewed in this case report.
Keywords: cloaca, hydrocolpos, pelvic musculature, perineal hernia
Perineal hernias are rare occurrence and may present as a mass in the perineum with a diagnostic dilemma. They are even rarer in children and may present as a gluteal mass as in this case and require correct diagnosis to avoid complications. The management is controversial with many approaches mentioned in the literature.
A child with cloaca was operated for transverse loop colostomy on day 1 of life and presented with acute obstruction at 1 month-jejunal resection and anastomosis was done for jejunal gangrene. There was no evidence of hydrocolpos. She presented at 5 months with complaints of stomal diarrhea, failure to thrive and a bulge through the perineum (Figure 1). On examination, her general condition was poor with weight 2.6kg, pallor, sunken anterior fontanelle, dry and wrinkled skin; abdominal distention with sunken stoma but there was no guarding and bowel sounds were present. There was a bulge in the perineum with positive cry impulse in the right gluteal region from which seropurulent fluid was aspirated (Figured 2&3).

Figure 2 CT Scan: A large cystic structure with air-fluid level with complex morphology in the abdomen & pelvis.
Figure 3 CT Scan: A large cystic structure with air-fluid level with complex morphology in the abdomen & pelvis.
Investigations revealed anaemia, leucocytosis, deranged electrolytes and metabolic acidosis. USG was suggestive of a suspicious obturator hernia on right side. CT scan was suggestive of bulging of a large complex cystic structure with air-fluid level on the right side. Sagittal reformations also suggested the inferior descent of the cystic structure through the perineal floor (Figures 4 &5). The deranged laboratory parameters were corrected and the child was taken for emergency exploration. Intra-operatively, it was found that the massive hydrocolpos was protruding through the perineum as the bulge. There was no perineal or obturator defect. Drainage of the massive hydrocolpos was done by an abdominal vaginostomy (Figures 6&7).
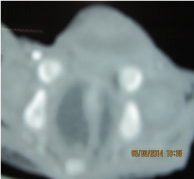
Figure 4 Axial scan at the level of perineum s/o bulging of the fluid filled structure on the right side.
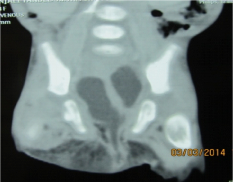
Figure 5 Sagittal reformations also s/o the inferior descent of the cystic structure through the perineal floor.
Vaginostomy functioned well in the post operative period and the distention decreased. There was a discharge of clear fluid from the perineal site for about 8 to 10 days postoperatively which stopped spontaneously. She is thriving well on follow-up (Figure 8).
Pelvic floor hernias are very rare1,2 and even rarer in paediatric age group. These hernias include obturator, perineal and sciatic hernias3,4 and may contain fat, bowel, rectum or bladder. Perineal hernias are described as anterior and posterior based on their position relative to transverse perineii muscle. The anterior form is in relation to the urogenital diaphragm and presents as a prolapsed in the area of the labia. The posterior perineal hernia is in relation to the levator ani and coccygeus muscle and usually present as a mass in between the rectum and ischial tuberosities.
Perineal hernias are also described as either primary (congenital or acquired) or secondary to some operative procedure involving the pelvic floor.3-7 Primary perineal hernias occur as a result of the developmental defect in the muscles of the pelvic floor.8,9 Perineal hernias may present a diagnostic dilemma and may be mistaken for a number of perineal masses like hematomas, lipomas, fibromas, rectoceles, cystocoeles, rectal prolapse or abscesses. A correct preoperative diagnosis is therefore very necessary to avoid complications.
The symptoms of perineal hernias are not usually very pronounced and they may present as a soft, reducible mass in the perineum. In infants, they may present as a triad of change in bowel movements, mass in the gluteal region and an abnormal rectal position.10,11 These hernias rarely incarcerate the neck is wide and surrounded by relatively elastic tissue. An anterior perineal hernia may cause difficulty in micturition because of the presence of a portion of the bladder in the hernia sac. A posterior hernia usually presents as difficulty in defecation.
A posterior perineal hernia usually protrudes below the fibres of gluteus maximus muscle and presents as a unilateral gluteal mass. This must be differentiated for a sciatic hernia which occurs through a greater or lesser sciatic foramen and manifests as a mass along the inferior margin of gluteus maximus muscle. This differentiation is done clinically by palpating the defect in the pelvic floor in a case of perineal hernia. The various investigations to support the diagnosis are Ultrasonography,12 Computed Tomography,5 Magnetic Resonance Imaging,13,14 or Herniography.15
The management is very controversial. Many approaches have been described in Literature. Some advocate the transabdominal approach,16,17 while others prefer the perineal approach.7,18 Some also recommend a combined abdominoperineal approach.19,20 Many tissues have been described for the closure of the pelvic defect like muscular flaps from the rectus abdominis, the gluteus maximus or the gracilis.21,22 Even the bladder has been used for closing the pelvic defect.23 Direct suturing or the use of a synthetic alloplastic mesh material has also been advised.24,25 Laparoscopic approaches have also been described in the literature.26 In children, good success has been reported by using perineal approach with primary closure.1,10,11
In patients with high anorectal malformations, the perineum & the pelvic musculature are severely underdeveloped and hypoplastic.27 The fibres of levator ani and the neuromuscular innervation are grossly deficient in the midline. Anal sphincter and the puborectalis sling are invariably absent. In patients with cloaca, hydrocolpos is a significant problem requiring early attention and treatment, especially during the first surgery itself. Hydrocolpos is vaginal distension with urine and cervical fluid accumulation due to a combination of stimulated secretory glands and vaginal obstruction.28 This in turn leads to a multitude of problems like recurrent urinary tract infections, hydrocolpos infection, sepsis, failure to thrive, ruptured hydrocolpos and development of hydronephrosis in previously normal kidneys.29
In this patient, the massive hydrocolpos was responsible for the perineal bulge which presented as a perineal hernia. This caused a diagnostic dilemma as there was no perineal defect at surgery and the hydrocolpos was effectively managed by abdominal vaginostomy.
A perineal hernia is a rare entity and may confront the physician with a diagnostic dilemma. A correct diagnosis is therefore necessary to avoid undue risks and complications. Unlike in adults, perineal hernias in children may be safely and successfully treated by primary surgical repair with a perineal approach. In this case, there was no perineal defect per se but the massively distended hydrocolpos together with the hypoplastic & poorly developed pelvic muscles in the cachexic patient were the cause for the bulge. The management of hydrocolpos alone in the form of abdominal vaginostomy was sufficient and no surgical intervention was required for the perineal bulge.
None.
None.
None.

©2014 Tiwari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.